Key Words: bronchoscopy, foreign body, pneumonia, aspiration
Abstract
Foreign body aspiration is a rare but life-threatening event. Most accidental aspiration events occur in children. In adults, it can represent up to 25% of cases. Bronchoscopy remains the gold standard for diagnosing and treating foreign body aspiration from the lower respiratory tract. A 63-year-old female smoker with a history of chronic alcoholism and exposure to pyrotechnic smoke presented a productive cough, with whitish expectoration, dyspnea and pleuritic chest pain on the right side. On chest X-ray, she presented opacity in 2/3 of the right hemithorax. Computed axial tomography revealed consolidation with an air bronchogram on the right hemithorax, cylindrical bronchiectasis, ground glass pattern and centrilobular nodules. Bronchoscopic examination revealed a foreign body covered with granulation tissue in the right segmental bronchus (B6). The granulation tissue was integrated into the foreign body. In a second attempt, the foreign body could be removed, which was of bone consistency, seemingly a bird bone, confirmed by pathological anatomy results. After further questioning, the patient reported that two years before, she had choked when eating chicken. She had a cough and an episode of hemoptysis, but she chose not to ask for medical advice.
|
Main messages
|
Introduction
Foreign body aspiration is a rare but life-threatening event, accounting for 0.16 to 0.33% of bronchoscopic procedures in adults [1]. Most accidental aspiration events occur in children; in adults, it can represent up to 25% of cases [2],[3]. It usually presents with a choking event followed by a persistent cough, but it is not uncommon for it to mimic more chronic diseases such as COPD, asthma, and obstructive pneumonia when the initial event goes unnoticed [1],[2],[4],[5],[6],[7]. When the diagnosis is not established immediately, the retained foreign body can cause recurrent pneumonia, bronchiectasis, recurrent hemoptysis, among other complications [8]. Bronchoscopy is the gold standard for diagnosing and treating foreign body aspiration from the lower airways [9]. We present an atypical case of foreign body aspiration with a history of recurrent pneumonia.
Patient information and clinical findings
We present the case of a 63-year-old woman who smokes seven packs/year, with a history of chronic alcoholism and exposure to pyrotechnic smoke for forty years. She consulted for a productive cough, with whitish expectoration, dyspnea on medium efforts, and pleuritic chest pain on the right side of 3 days of evolution. The physical examination revealed hypotension (blood pressure: 70/50mmHg, mean arterial pressure: 56.7), 38°C fever, oxygen saturation at 93% with a fraction of inspired oxygen at 0.21. She awakens with tachypnea. No cyanosis. On auscultation, vesicular murmurs and decreased vocal thrill were evidenced at the base of the right lung. She was admitted to the Hospital Regional Docente de Trujillo emergency and later hospitalized in the Pneumology Section.
Table 1. Hospitalization calendar.
Diagnostic evaluation
With the diagnostic hypothesis of recurrent bacterial pneumonia, studies were carried out to determine the etiology. In the chest X-ray requested upon admission, a radiopacity was observed in the 2/3 of the right hemithorax (Figure 1).
Figure 1. Initial chest X-ray.
Laboratory tests: Leukocytosis 22 090 without shift to the left, Hb: 8.5 gr / L; platelet count: 749,000 x mm3; arterial gas analysis: PCO2: 32.4; PO2: 60.6; PaO2 / FiO2: 288.5; A-aDO2: 49.5. The computerized axial tomography, six days after admission, revealed consolidation with air bronchogram at the base of the right hemithorax, cylindrical bronchiectasis with patchy aeration (entrapment), a heterogeneous subpleural ground-glass pattern associated with centrilobular nodules (Figures 2 and 3). She received antibiotic therapy with ceftriaxone 2 grams for seven days associated with inhalation therapy plus salbutamol. In the first bronchoscopy, 13 days after admission, an endobronchial lesion was seen in B6 of approximately 4 cm in diameter that obstructed the lumen. A biopsy (4 samples) was carried out in an erythematous area.
Figure 2. Tomographic image of the chest (pulmonary window).
A second bronchoscopy was performed seven days after the first (Figure 4A, 4B, 4C) because of persisting alterations in the right hemithorax in the clinical-radiological control. A foreign body covered with granulation tissue was observed in the right segmental bronchus (S6). The granulation tissue was poorly integrated with the foreign body, allowing it to move from the first bronchoscopy's initial position.
Figure 3. Tomographic image of the chest (mediastinal window).
Figure 4. second bronchoscopy image.
The foreign body turned out to be of bone consistency compatible with the naked eye with a bird bone, which was confirmed by pathological anatomy results 13 days after the second bronchoscopy (Figure 5A, 5B).
When we questioned the patient and her relatives again, they mentioned that she had a chronic cough after choking two years ago when eating chicken, which she did not consider. They also reported that three months before her current hospitalization, she presented an episode of hemoptysis (that lasted two days). She was hospitalized and later discharged with improvement in symptoms with a final diagnosis of pneumonia and bronchiectasis (Figure 5C).
Figure 5. Follow-up images of the foreign body.
Discussion
Foreign body aspiration is rare in healthy adults and occurs most commonly in children and the elderly. In adults, the incidence peaks in the sixth decade of life. Adults with foreign body aspiration often have an underlying risk factor, such as neuromuscular disease, altered mental status, facial trauma, endotracheal intubation, dental procedures, underlying lung disease, or either use of sedatives or alcohol. Additionally, adults with a decreased swallowing reflex due to underlying medical conditions are also at increased risk for aspiration. Commonly aspirated foreign bodies include metal objects (pins, screws, and nails), organic objects, including food particles, plastic objects, and teeth. The diagnosis is often challenging to establish, as some patients may not have a clear history of aspiration or may present late. Furthermore, patients can be misdiagnosed with chronic pneumonia, bronchitis, asthma, or malignancy [10].
Foreign bodies usually end up lodged in the lower bronchi or the intermediate bronchus of the bronchial tree and can sometimes be contained for a long time. In the United States, a case was reported of a 42-year-old man who had an aluminum beverage container part chronically retained in the left main bronchus for 12 years [10]. Occasionally, chest radiography shows a radiopaque body or consolidation, atelectasis, or airway effusion. A hyperdense image is often seen on chest computed tomography. Flexible bronchoscopy has become the procedure of choice for the diagnosis of foreign body aspirations in adults. In a case series of 38 314 patients who underwent flexible bronchoscopy, 94 were diagnosed with foreign bodies in the lower respiratory tract, 43 (46%) of them did not have a categorical history of aspiration or visible foreign body in their chest radiography or computed tomography (CT) [11]. Complications of foreign body aspiration include asphyxia, hemoptysis, infection, and post-obstruction bronchiectasis atelectasis. In secondary respiratory tract infections, the inhaled foreign body can act as a carrier of infectious material.
A study of 103 adult patients who underwent bronchoscopy removal of foreign bodies from the airways at a Seoul Tertiary Hospital between January 1999 and March 2017 found that 45 patients did not report to the hospital immediately due to symptoms post-aspiration respiratory tract infections. In 31 of the reported cases, airway foreign bodies were diagnosed during the work-up of recurrent pneumonia [12]. In a case published in Rome, flexible bronchoscopy showed the medial subsegmental bronchus completely obstructed by a foreign body and the lateral one occluded by a mucus-infected plug. The occlusive body turned out to be a peanut. After removing the foreign body, the patient's recovery was rapid, and atelectasis resolved [13]. In cases where the foreign body is lined with bulky and brittle granulation tissue, glucocorticoids may be helpful [14]. In difficult cases, successful extraction often requires the use of a rigid bronchoscope, which allows coaxial passage of various instruments, such as toothed forceps and a suction catheter. This technique presents specific problems because the anesthesiologist and the surgeon share the same space, i.e., the airway, which can lead to various complications (bleeding inside the airway, difficulties with ventilation, among others), so it is not considered as a first option [15]. In the present case, it was possible to extract the bird bone by flexible video bronchoscopy without complications, so it was not necessary to resort to rigid bronchoscopy.
In this patient, despite the absence of information on a foreign body's aspiration, flexible bronchoscopy was requested on two occasions during her last hospitalization due to recurrent pneumonia in the right lower lobe. After two years, a foreign body could be identified and removed from the target area, finally relieving the patient of its symptoms and resolving the infectious pulmonary process.
Conclusions
The current case shows the importance of obtaining a good medical history and being alert to the presence of recurrent bronchopulmonary infection. The clinical history of aspiration seems to be the most common predisposing factor, which, if this information does not exist, can result in a significant delay in diagnosis.
Notes
Roles of contribution
LARH: conceptualization, research, writing (review and editing), supervision, project management and acquisition of funds. LACU: methodology, validation, fund acquisition. JHV: formal analysis, resources, writing (review and editing), supervision and acquisition of funds. JLCP: Research. DCRC: data curation, project management. DLRV: writing (original draft preparation).
Competing interests
The authors declare not having any competing interests.
Funding
There was no funding for this work.
Ethical aspects
The family member/guardian's informed consent was obtained both for the diagnostic procedure and for the authorization of the publication of the clinical case.
From the editors
This article was originally submitted in Spanish, the language in which it was peer-reviewed. This English version is a translation provided by the authors that was lightly copyedited by the journal.

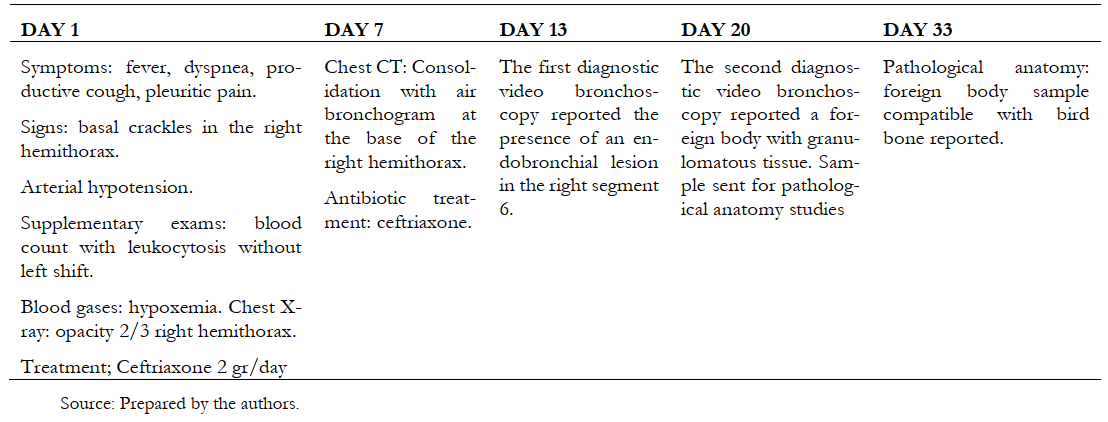 Table 1. Hospitalization calendar.
Table 1. Hospitalization calendar.

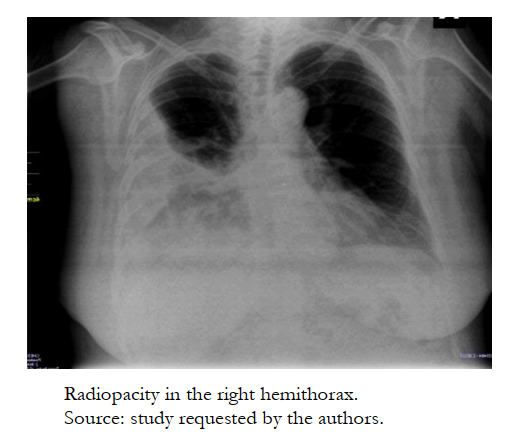 Figure 1. Initial chest X-ray.
Figure 1. Initial chest X-ray.

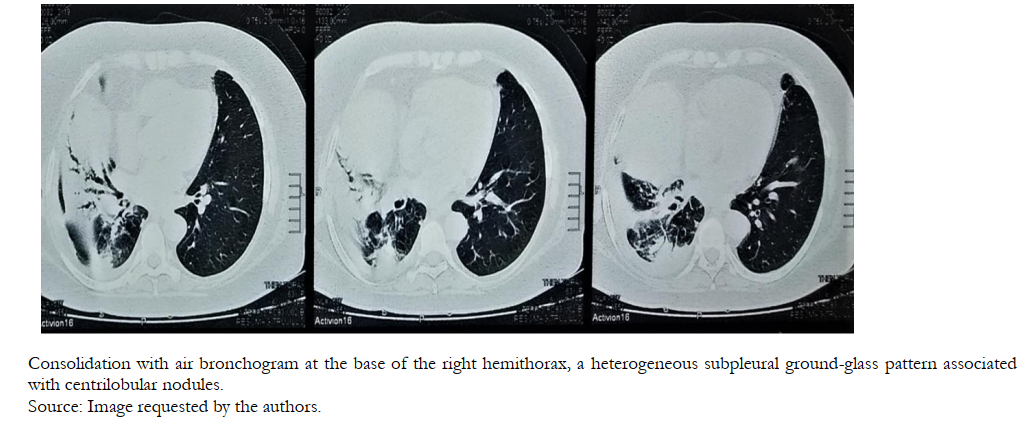 Figure 2. Tomographic image of the chest (pulmonary window).
Figure 2. Tomographic image of the chest (pulmonary window).

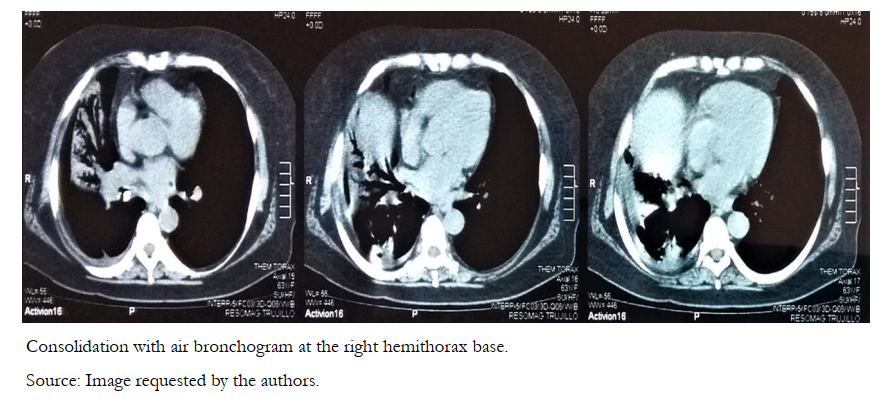 Figure 3. Tomographic image of the chest (mediastinal window).
Figure 3. Tomographic image of the chest (mediastinal window).

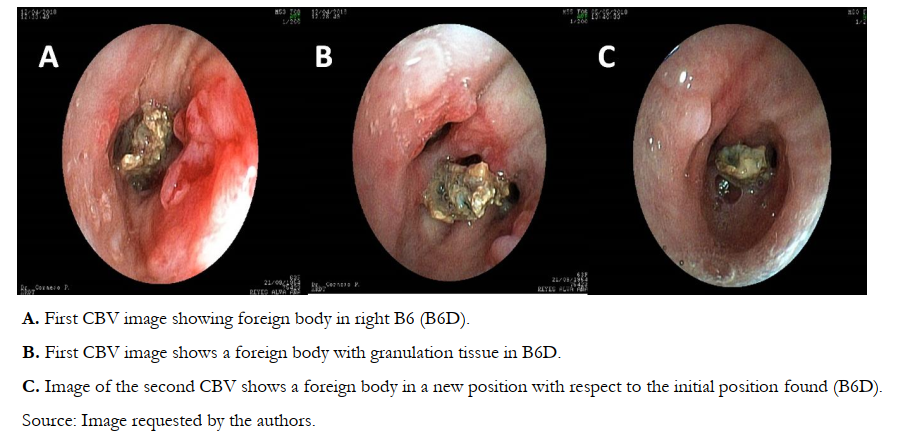 Figure 4. second bronchoscopy image.
Figure 4. second bronchoscopy image.

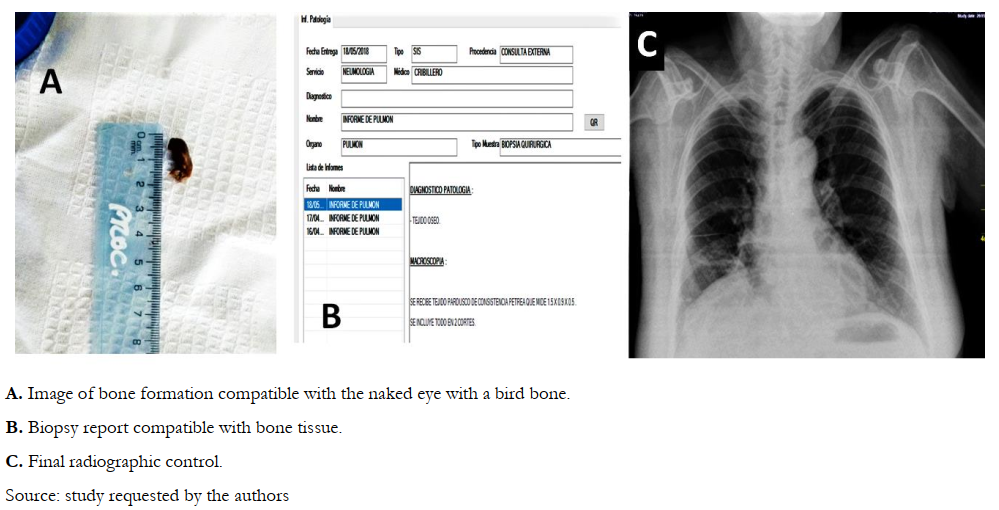 Figure 5. Follow-up images of the foreign body.
Figure 5. Follow-up images of the foreign body.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

La aspiración de cuerpo extraño es un evento poco frecuente en adultos, la mayoría de los eventos de aspiración accidental ocurren en niños, en los adultos puede representar hasta el 25% de los casos. La broncoscopía es el estándar de oro para el diagnóstico y el tratamiento de la aspiración de cuerpo extraño de las vías respiratorias bajas. Se reporta el caso de una mujer de 63 años fumadora, con antecedente de alcoholismo crónico y exposición frecuente a humo de pirotecnia. La paciente presentó tos productiva, con expectoración blanquecina, disnea y dolor torácico pleurítico en lado derecho. En la radiografía de tórax presentó opacidad en 2/3 del hemitórax derecho. La tomografía axial computarizada reveló consolidación con broncograma aéreo en la base del hemitórax derecho, bronquiectasias cilíndricas, patrón vidrio deslustrado y nódulos centrilobulillares. A través del examen broncoscópico se observó la presencia de un cuerpo extraño recubierto de tejido de granulación en el bronquio segmentario derecho (B6). El tejido de granulación estaba integrado al cuerpo extraño. En el segundo intento se pudo remover el cuerpo extraño, que resultó ser a simple vista de consistencia ósea, compatible con hueso de ave, lo que fue confirmado con resultados de anatomía patológica. En ampliación de historia clínica se obtuvo el dato que dos años antes tuvo atragantamiento al comer pollo; presentó tos y episodio de hemoptisis que la paciente prefirió no buscar atención médica.
 Authors:
Luis Alejandro Rodríguez Hidalgo[1,2], Luis Alberto Concepción-Urteaga[1,2], Julio Hilario-Vargas[2], Jorge Luis Cornejo-Portella[1], Diana Cecilia Ruiz-Caballero[1], Deysi Leslie Rojas-Vergara[1]
Authors:
Luis Alejandro Rodríguez Hidalgo[1,2], Luis Alberto Concepción-Urteaga[1,2], Julio Hilario-Vargas[2], Jorge Luis Cornejo-Portella[1], Diana Cecilia Ruiz-Caballero[1], Deysi Leslie Rojas-Vergara[1]
Affiliation:
[1] Hospital Regional Docente de Trujillo, Trujillo, Perú
[2] Facultad de Medicina de la Universidad Nacional de Trujillo, Trujillo, Perú
E-mail: alejandrorh@outlook.com
Author address:
[1] Manzana “A” Lote 1-M, Urbanización Los Portales del Golf Perú

Citation: Rodríguez Hidalgo LA, Concepción-Urteaga LA, Hilario-Vargas J, Cornejo-Portella JL, Ruiz-Caballero DC, Rojas-Vergara DL. Case report of recurring pneumonia due to unusual foreign body aspiration in the airway. Medwave 2021;21(02):e8136 doi: 10.5867/medwave.2021.02.8136
Submission date: 31/7/2020
Acceptance date: 3/3/2021
Publication date: 25/3/2021
Origin: Not commissioned
Type of review: Externally peer-reviewed by five reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Sehgal IS, Dhooria S, Ram B, Singh N, Aggarwal AN, Gupta D, et al. Foreign Body Inhalation in the Adult Population: Experience of 25,998 Bronchoscopies and Systematic Review of the Literature. Respir Care. 2015 Oct;60(10):1438-48. | CrossRef | PubMed |
- Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999 May;115(5):1357-62. | CrossRef | PubMed |
- Hsu Wc, Sheen Ts, Lin Cd, Tan Ct, Yeh Th, Lee Sy. Clinical experiences of removing foreign bodies in the airway and esophagus with a rigid endoscope: a series of 3217 cases from 1970 to 1996. Otolaryngol Head Neck Surg. 2000 Mar;122(3):450-4. | CrossRef | PubMed |
- Boyd M, Watkins F, Singh S, Haponik E, Chatterjee A, Conforti J, et al. Prevalence of flexible bronchoscopic removal of foreign bodies in the advanced elderly. Age Ageing. 2009 Jul;38(4):396-400. | CrossRef | PubMed |
- Dong YC, Zhou GW, Bai C, Huang HD, Sun QY, Huang Y, et al. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med. 2012;51(18):2515-9. | CrossRef | PubMed |
- Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990 Apr 15;112(8):604-9. | CrossRef | PubMed |
- Lin L, Lv L, Wang Y, Zha X, Tang F, Liu X. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin Interv Aging. 2014 Sep 24;9:1613-8. | CrossRef | PubMed |
- al-Majed SA, Ashour M, al-Mobeireek AF, al-Hajjaj MS, Alzeer AH, al-Kattan K. Overlooked inhaled foreign bodies: late sequelae and the likelihood of recovery. Respir Med. 1997 May;91(5):293-6. | CrossRef | PubMed |
- Hewlett JC, Rickman OB, Lentz RJ, Prakash UB, Maldonado F. Foreign body aspiration in adult airways: therapeutic approach. J Thorac Dis. 2017 Sep;9(9):3398-3409. | CrossRef | PubMed |
- Reddy RZ, Carter YM, Hsia DW. Successful Removal of a Chronic Aspirated Foreign Body after Twelve Years. Case Rep Pulmonol. 2018 May 31;2018:8241591. | CrossRef | PubMed |
- Fang YF, Hsieh MH, Chung FT, Huang YK, Chen GY, et al. Flexible bronchoscopy with multiple modalities for foreign body removal in adults. PLoS One. 2015 Mar 13;10(3):e0118993. | CrossRef | PubMed |
- Ng J, Kim S, Chang B, Lee K, Um SW, Kim H, et al. Clinical features and treatment outcomes of airway foreign body aspiration in adults. J Thorac Dis. 2019 Mar;11(3):1056-1064. | CrossRef | PubMed |
- Scarlata S, Rossi Bartoli I, Pedone C, Antonelli Incalzi R. Obstructive atelectasis of the lung. Postgrad Med J. 2016 Jun;92(1088):365. | CrossRef | PubMed |
- Rodríguez HL, Cornejo PJ, Ruiz CD. Cuerpo extraño inusual en la vía aérea del adulto. Archivos de Bronconeumologia. 2018;54 (Supl Congr 2):30-31. [On line] | Link |
- Dincq AS, Gourdin M, Collard E, Ocak S, D'Odémont JP, Dahlqvist C, et al. Anesthesia for adult rigid bronchoscopy. Acta Anaesthesiol Belg. 2014;65(3):95-103. | PubMed |
 Sehgal IS, Dhooria S, Ram B, Singh N, Aggarwal AN, Gupta D, et al. Foreign Body Inhalation in the Adult Population: Experience of 25,998 Bronchoscopies and Systematic Review of the Literature. Respir Care. 2015 Oct;60(10):1438-48. | CrossRef | PubMed |
Sehgal IS, Dhooria S, Ram B, Singh N, Aggarwal AN, Gupta D, et al. Foreign Body Inhalation in the Adult Population: Experience of 25,998 Bronchoscopies and Systematic Review of the Literature. Respir Care. 2015 Oct;60(10):1438-48. | CrossRef | PubMed | Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999 May;115(5):1357-62. | CrossRef | PubMed |
Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999 May;115(5):1357-62. | CrossRef | PubMed | Hsu Wc, Sheen Ts, Lin Cd, Tan Ct, Yeh Th, Lee Sy. Clinical experiences of removing foreign bodies in the airway and esophagus with a rigid endoscope: a series of 3217 cases from 1970 to 1996. Otolaryngol Head Neck Surg. 2000 Mar;122(3):450-4. | CrossRef | PubMed |
Hsu Wc, Sheen Ts, Lin Cd, Tan Ct, Yeh Th, Lee Sy. Clinical experiences of removing foreign bodies in the airway and esophagus with a rigid endoscope: a series of 3217 cases from 1970 to 1996. Otolaryngol Head Neck Surg. 2000 Mar;122(3):450-4. | CrossRef | PubMed | Boyd M, Watkins F, Singh S, Haponik E, Chatterjee A, Conforti J, et al. Prevalence of flexible bronchoscopic removal of foreign bodies in the advanced elderly. Age Ageing. 2009 Jul;38(4):396-400. | CrossRef | PubMed |
Boyd M, Watkins F, Singh S, Haponik E, Chatterjee A, Conforti J, et al. Prevalence of flexible bronchoscopic removal of foreign bodies in the advanced elderly. Age Ageing. 2009 Jul;38(4):396-400. | CrossRef | PubMed | Dong YC, Zhou GW, Bai C, Huang HD, Sun QY, Huang Y, et al. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med. 2012;51(18):2515-9. | CrossRef | PubMed |
Dong YC, Zhou GW, Bai C, Huang HD, Sun QY, Huang Y, et al. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med. 2012;51(18):2515-9. | CrossRef | PubMed | Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990 Apr 15;112(8):604-9. | CrossRef | PubMed |
Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990 Apr 15;112(8):604-9. | CrossRef | PubMed | Lin L, Lv L, Wang Y, Zha X, Tang F, Liu X. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin Interv Aging. 2014 Sep 24;9:1613-8. | CrossRef | PubMed |
Lin L, Lv L, Wang Y, Zha X, Tang F, Liu X. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin Interv Aging. 2014 Sep 24;9:1613-8. | CrossRef | PubMed | al-Majed SA, Ashour M, al-Mobeireek AF, al-Hajjaj MS, Alzeer AH, al-Kattan K. Overlooked inhaled foreign bodies: late sequelae and the likelihood of recovery. Respir Med. 1997 May;91(5):293-6. | CrossRef | PubMed |
al-Majed SA, Ashour M, al-Mobeireek AF, al-Hajjaj MS, Alzeer AH, al-Kattan K. Overlooked inhaled foreign bodies: late sequelae and the likelihood of recovery. Respir Med. 1997 May;91(5):293-6. | CrossRef | PubMed | Hewlett JC, Rickman OB, Lentz RJ, Prakash UB, Maldonado F. Foreign body aspiration in adult airways: therapeutic approach. J Thorac Dis. 2017 Sep;9(9):3398-3409. | CrossRef | PubMed |
Hewlett JC, Rickman OB, Lentz RJ, Prakash UB, Maldonado F. Foreign body aspiration in adult airways: therapeutic approach. J Thorac Dis. 2017 Sep;9(9):3398-3409. | CrossRef | PubMed | Reddy RZ, Carter YM, Hsia DW. Successful Removal of a Chronic Aspirated Foreign Body after Twelve Years. Case Rep Pulmonol. 2018 May 31;2018:8241591. | CrossRef | PubMed |
Reddy RZ, Carter YM, Hsia DW. Successful Removal of a Chronic Aspirated Foreign Body after Twelve Years. Case Rep Pulmonol. 2018 May 31;2018:8241591. | CrossRef | PubMed | Fang YF, Hsieh MH, Chung FT, Huang YK, Chen GY, et al. Flexible bronchoscopy with multiple modalities for foreign body removal in adults. PLoS One. 2015 Mar 13;10(3):e0118993. | CrossRef | PubMed |
Fang YF, Hsieh MH, Chung FT, Huang YK, Chen GY, et al. Flexible bronchoscopy with multiple modalities for foreign body removal in adults. PLoS One. 2015 Mar 13;10(3):e0118993. | CrossRef | PubMed | Ng J, Kim S, Chang B, Lee K, Um SW, Kim H, et al. Clinical features and treatment outcomes of airway foreign body aspiration in adults. J Thorac Dis. 2019 Mar;11(3):1056-1064. | CrossRef | PubMed |
Ng J, Kim S, Chang B, Lee K, Um SW, Kim H, et al. Clinical features and treatment outcomes of airway foreign body aspiration in adults. J Thorac Dis. 2019 Mar;11(3):1056-1064. | CrossRef | PubMed | Scarlata S, Rossi Bartoli I, Pedone C, Antonelli Incalzi R. Obstructive atelectasis of the lung. Postgrad Med J. 2016 Jun;92(1088):365. | CrossRef | PubMed |
Scarlata S, Rossi Bartoli I, Pedone C, Antonelli Incalzi R. Obstructive atelectasis of the lung. Postgrad Med J. 2016 Jun;92(1088):365. | CrossRef | PubMed | Rodríguez HL, Cornejo PJ, Ruiz CD. Cuerpo extraño inusual en la vía aérea del adulto. Archivos de Bronconeumologia. 2018;54 (Supl Congr 2):30-31. [On line] | Link |
Rodríguez HL, Cornejo PJ, Ruiz CD. Cuerpo extraño inusual en la vía aérea del adulto. Archivos de Bronconeumologia. 2018;54 (Supl Congr 2):30-31. [On line] | Link | Dincq AS, Gourdin M, Collard E, Ocak S, D'Odémont JP, Dahlqvist C, et al. Anesthesia for adult rigid bronchoscopy. Acta Anaesthesiol Belg. 2014;65(3):95-103. | PubMed |
Dincq AS, Gourdin M, Collard E, Ocak S, D'Odémont JP, Dahlqvist C, et al. Anesthesia for adult rigid bronchoscopy. Acta Anaesthesiol Belg. 2014;65(3):95-103. | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








