Key Words: aortic aneurysm, pseudoaneursym, hemoptysis
Abstract
Pseudoaneurysm is defined as a reperfused pulsatile hematoma, encapsulated and communicated with the damaged vessel's lumen. It originates when there is a disruption of the arterial wall. Hemoptysis is a very rare sign/symptom of a thoracic aortic aneurysm or pseudoaneurysm. There is little information on hemoptysis associated with aortic aneurysm rupture, whose mechanisms are not explained by the presence of an aortopulmonary fistula. Among the hypotheses to explain this phenomenon, is the ability of the bronchial arteries to become hyperplasic and tortuous in the presence of a lesion that modifies the pulmonary architecture, being more susceptible to rupture. There are also descriptions of direct lung parenchymal injury from ruptured aneurysm. The present case illustrates that we must consider the hemoptysis as a warning sign in differential diagnosis of aortic aneurysms and pseudo aneurysms, among other causes, that it can be fatal in a short time due to massive hemorrhage.
|
Main messages
|
Introduction
Hemoptysis is a rare presentation of a thoracic aortic aneurysm. Even with emergency handling, it is a warning sign of life-threatening, usually fatal, complications[1].
Pseudoaneurysm is defined as an encapsulated, reperfused, pulsatile hematoma in communication with a damaged vessel’s lumen. It originates from a disruption of the arterial wall due to arterial pressure. The blood dissects in the adjacent tissues to the damaged artery and causes an aneurysmal sac that communicates with the arterial lumen[2]. Thoracic aortic aneurysms expand slowly and, generally, silently. This silent process makes it difficult to diagnose early. There is a difference between pseudoaneurysm and aneurysm: the latter is formed histologically by all the arterial layers[1].
Hemoptysis is a very rare sign/symptom of the presentation of thoracic aortic aneurysms and, therefore, of thoracic aortic pseudoaneurysms[3],[4]. Parenchyma or airway pulmonary erosion induces the coughing up of blood and massive hemoptysis, which is potentially dangerous and deadly[5]. Among the studies to be performed, the chest X-ray is the first examination to locate the issue, showing mediastinal widening. On the other hand, ultrasound in the patient’s bed is used widely by emergency physicians to help diagnose life-threatening pathological cardiovascular conditions, such as aortic aneurysm[6]; additionally, the performance of a thoracic tomography with contrast confirms the presence of thoracic aortic aneurysms and aortic pseudoaneurysms[7].
This report aims to communicate a rare presentation of hemoptysis in a pseudoaneurysm of the thoracic aorta.
Patient information
An 82-year-old male patient, who in November 2019 presented a moderate amount of hemoptysis (approx. ± 300 ml), went to the emergency room at the Hospital Regional Docente de Trujillo. After being attended to, he requested a voluntary discharge from the hospital. In January 2020, he presented a new hemoptysis episode, was readmitted to the emergency department, and then to the pulmonology service.
Two months before being admitted to the pulmonology service, he reported having dyspnea, chest pain, and a coughing episode with hemoptoic sputum. When he was treated in our hospital’s emergency room, a chest X-ray was requested, reporting: ectasia of the aortic arch + signs of right basal interstitium and two sputum smear microscopies that were negative. When symptoms improved, the patient requested voluntary discharge.
Clinical findings
On admission (01/29/2020): physical examination, BP: 90/60 mmHg RR: 20x ‘HR: 83x’ SatO2: 93% FIO2: 21%.
General assessment: patient in apparent regular general condition, regular nutritional status, and regular hydration status, spontaneously ventilating without supplemental oxygen.
Skin and mucosa: Pale + / +++, capillary refill <2 seconds.
Respiratory system: Decreased vocal thrill, decreased vocal resonance and decreased vesicular murmur in left hemithorax.
Cardiovascular system: Rhythmic and regular heart sounds, no murmurs, synchronous heart sounds with radial pulses. Tibial and pedial pulses present ++ / +++.
Blood pressure values in limbs were:
- Right upper limb: 110/70 millimeters of mercury.
- Left upper limb: 100/70 millimeters of mercury.
- Right lower limb: 90/60 millimeters of mercury.
- Left lower limb: 80/60 millimeters of mercury.
Additional tests: Hb: 8.8 gr/dl. Hematocrit: 27.8%. Hemogram: leukocytosis with no left shift. Platelets: 507 mm3.
Diagnostic assessment
Chest radiography (Figure 1): Opacification at the level of the mid and upper field of the left hemithorax with irregular contours in relation to pneumonia, elevation of the left hemidiaphragm, no caverns, and normal cardiac area.
Day 2 of hospitalization
Control exams: Hto: 25%, PT: 31.2 seconds, PTT: 13.5 seconds, e INR: 0.97, Reticulocytes: 1.27% and Platelets: 478 000.
High-resolution computed tomography (HRCT) of the lungs (Figure 2) reported: thoracic aortic pseudoaneurysm, declining pleural fluid associated with areas of left-side aneumatosis and nonspecific subacute interstitial lung disease, mediastinal lymphadenopathy, left hemidiaphragm, and dorsal osteoarthrosis.
Day 16 of hospitalization
Aortic angiotomography with and without contrast in 3D (Figure 3) concluded: atherosclerosis + aortic elongation + saccular aneurysm of descending aorta. Segmental atelectasis of the left lower lobe with hemidiaphragm elevation and ipsilateral pleural effusion. Signs of pulmonary fibrosis. Dorsal spondyloarthritis.
Table 1. Schedule of procedures and discharge.
Therapeutic intervention
Due to the decrease in hematocrit, a packet of blood was transfused on day 16 of hospitalization, raising the hematocrit to 28%.
Follow-up and outcomes
During his hospitalization in the Pneumology Department, the patient remained in complete rest and did not show any discomfort despite having four hemoptysis episodes of approximately 50 ml, the penultimate episode coming on day 17 of hospitalization with approximately 10 ml of bleeding.
During the wait for a transfer to a high-resolution capacity hospital (Lima), daily coordination was carried out to manage complicated cardiovascular disease. Before transferring the patient, on day 28 of hospitalization, he presented sudden massive hemoptysis and died.
Discussion
Most aortic aneurysms are asymptomatic and are found during radiological evaluation for other causes[1],[8]. The aorta is very susceptible to tearing in two places: immediately adjacent to the heart at the aorta’s origin and, posteriorly, distal to the left subclavian, where the aorta is fixed in the region of the spinal column. The tear in the first place usually causes sudden death, preventing the aneurysm from developing. In other cases, the intima and media may divide transversely. However, if the adventitia remains intact, a pulsatile hematoma forms and later causes a false aneurysm (pseudoaneurysm)[2]. The resulting hematoma can prevent bleeding for hours or weeks if sudden death does not occur. More prolonged survival is associated with forming a false aneurysm[9],[10].
Aneurysms can produce respiratory manifestations due to compression and obstruction of either the bronchia or trachea. Less frequently, an aortobronchial fistula occurs, which, as in the case we described, can be fatal in a short time due to massive hemorrhage[11],[12]. The primary manifestation was hemoptysis of mild to moderate intensity that disappeared spontaneously and was maintained for approximately three months until the moment of the patient’s death as a result of massive hemoptysis.
There is little information on hemoptysis associated with a ruptured aortic aneurysm; the presence of an aortopulmonary fistula does not explain its mechanism. Among the hypotheses used to explain this phenomenon is the bronchial arteries’ ability to become hyperplastic and tortuous in the presence of a lesion that modifies the lung architecture—as it is more susceptible to rupture. There are also descriptions of the pulmonary parenchyma’s direct lesions due to a ruptured aneurysm[13],[14].
This case illustrates that we must consider the differential diagnosis of hemoptysis, aortic aneurysms, and pseudoaneurysms, among other causes.
This case illustrates why we must consider hemoptysis as a warning sign in the differential diagnosis of aortic aneurysms and pseudoaneurysms that place people at risk of death.
Patient perspective
He was not aware of the seriousness of the case. The patient died on day 28 of hospitalization.
Conclusion
Early diagnosis for possible treatment with endovascular techniques such as the placement of a “stent” to carry out a selective embolization of the pseudoaneurysm sac is warranted[15].
Notes
Authorship roles
LRH, DRC: Conceptualization, methodology, software, validation, formal analysis, investigation, resources, data curation, writing original draft, writing review and editing, visualization, supervision, project administration, funding acquisition. LCU, JHV: Conceptualization, methodology, validation, software, formal analysis, investigation, resources, writing original draft, writing review and editing, visualization.
Conflicts of interest
The authors declare no conflicts of interest and sent the ICMJE formats to Medwave.
Financing
The authors declare that they have not received any funding for this study.
Ethical considerations
The patient’s granddaughter has signed the informed consent requested by Medwave. Patient privacy has been scrupulously respected. The Hospital authorized the study by reviewing the medical history. A consent copy was sent to the publisher of the magazine.
From the editors
The original version of this manuscript was submitted in Spanish. This English version was submitted by the authors and has been copyedited by the Journal.

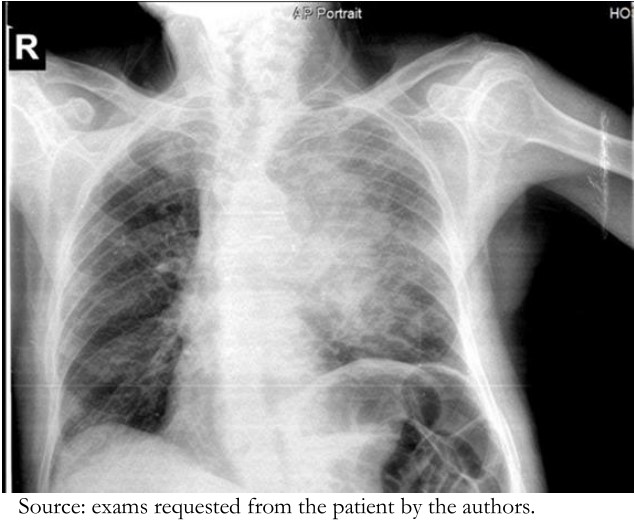 Figure 1. Chest X-ray (admission hospitalization): Opacification at the level of the mid and upper field of the left hemithorax with irregular contours in relation to pneumonia. Elevation of the left hemidiaphragm.
Figure 1. Chest X-ray (admission hospitalization): Opacification at the level of the mid and upper field of the left hemithorax with irregular contours in relation to pneumonia. Elevation of the left hemidiaphragm.

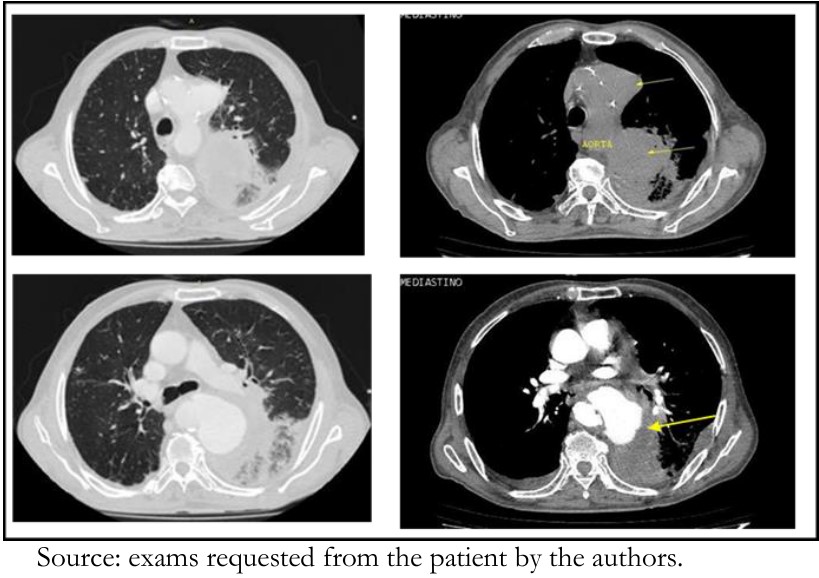 Figure 2. HRCT of the lungs (Day 2 of hospitalization): Pseudoaneurysm of the thoracic aorta (arrow), with signs of acute rupture. Decline in pleural fluid.
Figure 2. HRCT of the lungs (Day 2 of hospitalization): Pseudoaneurysm of the thoracic aorta (arrow), with signs of acute rupture. Decline in pleural fluid.

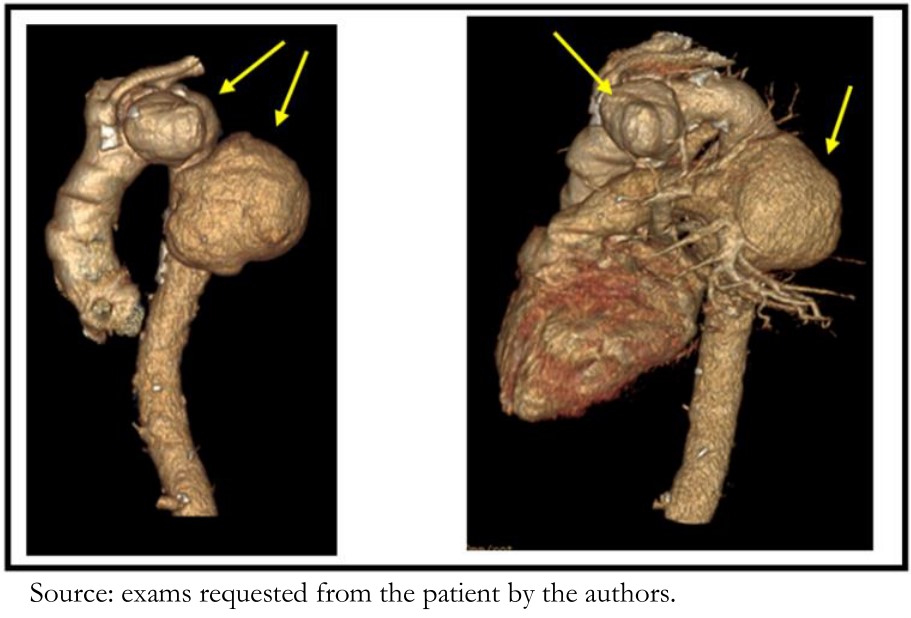 Figure 3. Angiotomography 3D (Day 16 of hospitalization): Atherosclerosis + aortic elongation + Saccular aneurysm of descending aorta (arrows).
Figure 3. Angiotomography 3D (Day 16 of hospitalization): Atherosclerosis + aortic elongation + Saccular aneurysm of descending aorta (arrows).

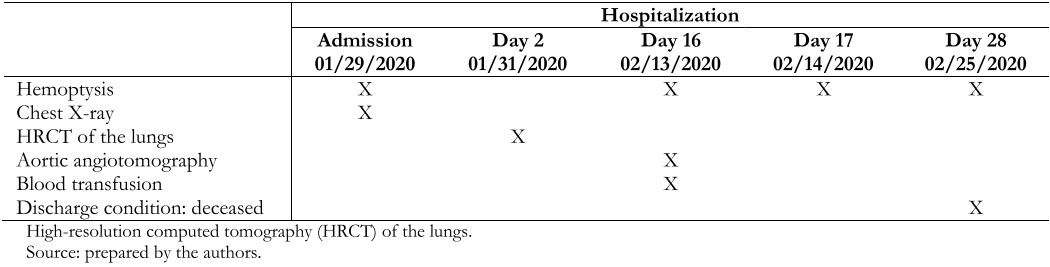 Table 1. Schedule of procedures and discharge.
Table 1. Schedule of procedures and discharge.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

El pseudoaneurisma se define como un hematoma pulsátil repermeabilizado, encapsulado y en comunicación con la luz de un vaso dañado. Se origina cuando hay una disrupción de la pared arterial. La hemoptisis es un signo/síntoma de presentación muy rara de aneurisma aórtico torácico y de pseudoaneurisma aórtico torácico. Hay poca información sobre la hemoptisis asociada con la ruptura del aneurisma aórtico cuyo mecanismo no se explica por la presencia de una fístula aortopulmonar. Entre las hipótesis para explicar este fenómeno, se encuentra la capacidad de las arterias bronquiales de volverse hiperplásicas y tortuosas en presencia de una lesión que modifica la arquitectura pulmonar, siendo más susceptibles a la ruptura. También hay descripciones de lesiones directas del parénquima pulmonar por aneurisma roto. El presente caso nos ilustra que debemos considerar a la hemoptisis como signo de alarma en el diagnóstico diferencial de los aneurismas y pseudoaneurismas aórticos entre otras causas que puede ser fatal en breve tiempo por una hemorragia masiva.
 Authors:
Luis Alejandro Rodríguez-Hidalgo[1,2], Luis Alberto Concepción-Urteaga[1,2], Julio Santos Hilario-Vargas[3], Diana Cecilia Ruiz-Caballero[1,2]
Authors:
Luis Alejandro Rodríguez-Hidalgo[1,2], Luis Alberto Concepción-Urteaga[1,2], Julio Santos Hilario-Vargas[3], Diana Cecilia Ruiz-Caballero[1,2]
Affiliation:
[1] Centro de Excelencia para Manejo de Tuberculosis Luz Caviedes Rojas-Hospital Regional Docente de Trujillo, Trujillo, Perú
[2] Departamento de Medicina, Facultad de Medicina, Universidad Nacional de Trujillo, Trujillo, Perú
[3] Departamento de Fisiología, Facultad de Medicina, Universidad Nacional de Trujillo, Trujillo, Perú
E-mail: alejandrorh@outlook.com
Author address:
[1] Manzana A Lote 1-M, Urbanización Los Portales del Golf Víctor Larco Trujillo, Perú

Citation: Rodríguez-Hidalgo LA, Concepción-Urteaga LA, Hilario-Vargas JS, Ruiz-Caballero DC. Hemoptysis as a warning sign of thoracic aorta pseudoaneurysm: A case report. Medwave 2021;21(1):e8112 doi: 10.5867/medwave.2021.01.8112
Submission date: 30/4/2020
Acceptance date: 20/11/2020
Publication date: 9/2/2021
Origin: Not commissioned
Type of review: Externally peer-reviewed by four reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Akbari F, Rezaeetalab F, Mozdourian M. Hemoptysis as a rare presentation of thoracic aorta aneurysm. J Cardiothoracic Med. 2020;8(1):581-583. | CrossRef |
- Abadal JM, Del Toro A, Pasinati G. Tratamiento de aneurismas y pseudoaneurismas. Revista radiológica. [On line]. | Link |
- Oğuz Ş, Bekirçavuşoğlu S, Pulathan Z. Endovascular Treatment of Thoracic Aortic Aneurysm Causing Life-Threatening Hemoptysis: Two Case Reports. Case Rep Vasc Med. 2018 May 15;2018:7014170. | CrossRef | PubMed |
- Larici AR, Franchi P, Occhipinti M, Contegiacomo A, del Ciello A, Calandriello L, et al. Diagnosis and management of hemoptysis. Diagn Interv Radiol. 2014 Jul-Aug;20(4):299-309. | CrossRef | PubMed |
- Bashir M, Fok M, Hammoud I, Rimmer L, Shaw M, Field M, et al. A Perspective on Natural History and Survival in Nonoperated Thoracic Aortic Aneurysm Patients. Aorta (Stamford). 2013 Aug 1;1(3):182-9. | CrossRef | PubMed |
- Cheng CY, Pan HY, Kung CT. Point-of-care ultrasound diagnosis of thoracic aortic aneurysm in a patient presenting with hemoptysis. Ultrasound in Medicine and Biology. 2019;45:S85. | CrossRef |
- Ashida-Urata N, Nomura T, Kamiya H, Keira N. Hemoptysis is a critical sign of aortobronchial fistula. Intern Med. 2017;56(19):2683-4. | CrossRef |
- Stembergh WC, Gonze MD, Garrarrd CL, Money SR. Abdominal and thoracoabdominal aortic aneurysm. Surg Clin North Am. 1998;78(5):827-43. | CrossRef |
- Vega J, Gonzalez D, Yankovic W, Oroz J, Guamán R, Castro N. Aneurismas de la aorta torácica. Historia natural, diagnóstico y tratamiento. Rev Chil Cardiol. 2014;33(2):127-135. [On line]. | Link |
- Pino APP, Gassiot C, Páez I, Rodríguez JC, Hernández Y. Pseudoaneurisma de la aorta con fístula aortobronquial como causa de hemoptisis. Rev Cubana Med. 1999;38(3):212-4. [On line]. | Link |
- Son SA, Lee DH, Kim GJ. Effective strategy in the treatment of aortobronchial fistula with recurrent hemoptysis. Yeungnam Univ J Med. 2020 Apr;37(2):141-146. | CrossRef | PubMed |
- Johansson G, Markström U, Swedenborg J. Ruptured thoracic aortic aneurysms: A study of incidence and mortality rates. J Vasc Surg. 1995;21(6):985-8. | CrossRef |
- Tayal N, Joshi S, Gupta R. Haemoptysis: a rare presentation of aortic pseudoaneurysm. Egypt J Chest Dis Tuberc. 2019;68(2):263-5. [On line]. | Link |
- Pereira T, Lipari L, Rodrigues C, Costa JV, AlencarJ, Morinaga Ch, et al. Hemoptysis as a rare clinical manifestation of ruptured aortic aneurysm. The European Emergency Medicine Congress, October 2019. Prague. [On line]. | Link |
- Lamprecht Y, Gallardo AE, Marín DE, Montes FE, Fernández LV, Yllera CE. Pseudoaneurysms: all you need to know. Congress: ECR 2018. Poster Number:C-3142. | CrossRef |
 Akbari F, Rezaeetalab F, Mozdourian M. Hemoptysis as a rare presentation of thoracic aorta aneurysm. J Cardiothoracic Med. 2020;8(1):581-583. | CrossRef |
Akbari F, Rezaeetalab F, Mozdourian M. Hemoptysis as a rare presentation of thoracic aorta aneurysm. J Cardiothoracic Med. 2020;8(1):581-583. | CrossRef | Abadal JM, Del Toro A, Pasinati G. Tratamiento de aneurismas y pseudoaneurismas. Revista radiológica. [On line]. | Link |
Abadal JM, Del Toro A, Pasinati G. Tratamiento de aneurismas y pseudoaneurismas. Revista radiológica. [On line]. | Link | Oğuz Ş, Bekirçavuşoğlu S, Pulathan Z. Endovascular Treatment of Thoracic Aortic Aneurysm Causing Life-Threatening Hemoptysis: Two Case Reports. Case Rep Vasc Med. 2018 May 15;2018:7014170. | CrossRef | PubMed |
Oğuz Ş, Bekirçavuşoğlu S, Pulathan Z. Endovascular Treatment of Thoracic Aortic Aneurysm Causing Life-Threatening Hemoptysis: Two Case Reports. Case Rep Vasc Med. 2018 May 15;2018:7014170. | CrossRef | PubMed | Larici AR, Franchi P, Occhipinti M, Contegiacomo A, del Ciello A, Calandriello L, et al. Diagnosis and management of hemoptysis. Diagn Interv Radiol. 2014 Jul-Aug;20(4):299-309. | CrossRef | PubMed |
Larici AR, Franchi P, Occhipinti M, Contegiacomo A, del Ciello A, Calandriello L, et al. Diagnosis and management of hemoptysis. Diagn Interv Radiol. 2014 Jul-Aug;20(4):299-309. | CrossRef | PubMed | Bashir M, Fok M, Hammoud I, Rimmer L, Shaw M, Field M, et al. A Perspective on Natural History and Survival in Nonoperated Thoracic Aortic Aneurysm Patients. Aorta (Stamford). 2013 Aug 1;1(3):182-9. | CrossRef | PubMed |
Bashir M, Fok M, Hammoud I, Rimmer L, Shaw M, Field M, et al. A Perspective on Natural History and Survival in Nonoperated Thoracic Aortic Aneurysm Patients. Aorta (Stamford). 2013 Aug 1;1(3):182-9. | CrossRef | PubMed | Cheng CY, Pan HY, Kung CT. Point-of-care ultrasound diagnosis of thoracic aortic aneurysm in a patient presenting with hemoptysis. Ultrasound in Medicine and Biology. 2019;45:S85. | CrossRef |
Cheng CY, Pan HY, Kung CT. Point-of-care ultrasound diagnosis of thoracic aortic aneurysm in a patient presenting with hemoptysis. Ultrasound in Medicine and Biology. 2019;45:S85. | CrossRef | Ashida-Urata N, Nomura T, Kamiya H, Keira N. Hemoptysis is a critical sign of aortobronchial fistula. Intern Med. 2017;56(19):2683-4. | CrossRef |
Ashida-Urata N, Nomura T, Kamiya H, Keira N. Hemoptysis is a critical sign of aortobronchial fistula. Intern Med. 2017;56(19):2683-4. | CrossRef | Stembergh WC, Gonze MD, Garrarrd CL, Money SR. Abdominal and thoracoabdominal aortic aneurysm. Surg Clin North Am. 1998;78(5):827-43. | CrossRef |
Stembergh WC, Gonze MD, Garrarrd CL, Money SR. Abdominal and thoracoabdominal aortic aneurysm. Surg Clin North Am. 1998;78(5):827-43. | CrossRef | Vega J, Gonzalez D, Yankovic W, Oroz J, Guamán R, Castro N. Aneurismas de la aorta torácica. Historia natural, diagnóstico y tratamiento. Rev Chil Cardiol. 2014;33(2):127-135. [On line]. | Link |
Vega J, Gonzalez D, Yankovic W, Oroz J, Guamán R, Castro N. Aneurismas de la aorta torácica. Historia natural, diagnóstico y tratamiento. Rev Chil Cardiol. 2014;33(2):127-135. [On line]. | Link | Pino APP, Gassiot C, Páez I, Rodríguez JC, Hernández Y. Pseudoaneurisma de la aorta con fístula aortobronquial como causa de hemoptisis. Rev Cubana Med. 1999;38(3):212-4. [On line]. | Link |
Pino APP, Gassiot C, Páez I, Rodríguez JC, Hernández Y. Pseudoaneurisma de la aorta con fístula aortobronquial como causa de hemoptisis. Rev Cubana Med. 1999;38(3):212-4. [On line]. | Link | Son SA, Lee DH, Kim GJ. Effective strategy in the treatment of aortobronchial fistula with recurrent hemoptysis. Yeungnam Univ J Med. 2020 Apr;37(2):141-146. | CrossRef | PubMed |
Son SA, Lee DH, Kim GJ. Effective strategy in the treatment of aortobronchial fistula with recurrent hemoptysis. Yeungnam Univ J Med. 2020 Apr;37(2):141-146. | CrossRef | PubMed | Johansson G, Markström U, Swedenborg J. Ruptured thoracic aortic aneurysms: A study of incidence and mortality rates. J Vasc Surg. 1995;21(6):985-8. | CrossRef |
Johansson G, Markström U, Swedenborg J. Ruptured thoracic aortic aneurysms: A study of incidence and mortality rates. J Vasc Surg. 1995;21(6):985-8. | CrossRef | Tayal N, Joshi S, Gupta R. Haemoptysis: a rare presentation of aortic pseudoaneurysm. Egypt J Chest Dis Tuberc. 2019;68(2):263-5. [On line]. | Link |
Tayal N, Joshi S, Gupta R. Haemoptysis: a rare presentation of aortic pseudoaneurysm. Egypt J Chest Dis Tuberc. 2019;68(2):263-5. [On line]. | Link | Pereira T, Lipari L, Rodrigues C, Costa JV, AlencarJ, Morinaga Ch, et al. Hemoptysis as a rare clinical manifestation of ruptured aortic aneurysm. The European Emergency Medicine Congress, October 2019. Prague. [On line]. | Link |
Pereira T, Lipari L, Rodrigues C, Costa JV, AlencarJ, Morinaga Ch, et al. Hemoptysis as a rare clinical manifestation of ruptured aortic aneurysm. The European Emergency Medicine Congress, October 2019. Prague. [On line]. | Link | Lamprecht Y, Gallardo AE, Marín DE, Montes FE, Fernández LV, Yllera CE. Pseudoaneurysms: all you need to know. Congress: ECR 2018. Poster Number:C-3142. | CrossRef |
Lamprecht Y, Gallardo AE, Marín DE, Montes FE, Fernández LV, Yllera CE. Pseudoaneurysms: all you need to know. Congress: ECR 2018. Poster Number:C-3142. | CrossRef |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








