Key Words: rhinoplasty, nasal dorsum, irregularities.
Abstract
Palpable irregularities along the nasal dorsum are a frequent complication of dorsal handling in rhinoplasty because resection techniques are used. This is often a result of improper management of the dorsum after resection. The surgical technique for handling of dorsal irregularities following dorsal resection is described. The key steps to avoid irregularities are diamond rasps, autospreader and morselized cartilage as camouflage. Following resection of the hump, the anatomy of the nasal dorsum should be adequately restructured; thereby we achieve an adequate aesthetic result and ideally preventing irregularities on palpation.
Introduction
The anatomy of the nasal dorsum is complex and requires intimate knowledge of this in order to ensure that it is properly managed. Dorsal hump reduction is a commonly performed rhinoplasty technique and proper reconstruction is essential to restoring nasal function and aesthetic contour [1].
The middle nasal vault is comprised of paired upper lateral cartilages (ULC), which are articulated superiorly with the distal end of the nasal bones and medially with the cartilaginous septum [2]. The medial edges of the upper lateral cartilages adhere to the lateral anterior septal extension in an end to end form. This union sets an angle of approximately 15 degrees, forming the apex of the internal nasal valve[3].
The nasal skin is thin and the subcutaneous tissue almost inexistent overlying the union of the upper lateral cartilage and bony vault. It is at this location where particular care should be taken in order to achieve a smooth dorsum and continuous aesthetic lines [4].
The sequelae of inadequate management of this area include palpable dorsal irregularities, open roof, inverted V and excessive narrowing of the middle nasal vault. These unwanted surgical stigmata are often the main indications for secondary rhinoplasty [3],[4],[5].
In order to avoid these complications, surgical instruments used in dorsal hump reduction have become more conservative. Currently, the use of rasps has displaced other tools including saws and osteotomes [4]. Additionally there has been a transition from en bloc resection to component resections [4].
Although the visual aesthetic and functional outcome are the most important parameters that determine a successful procedure, the importance of avoiding palpable irregularities cannot be understated. Regardless of the fact that irregularities may not be visible, there is a significant psychological component if the patient can feel abnormalities. Hence, in order to maximize patient satisfaction, every effort should be made to employ available techniques to prevent this complication.
Multiple techniques have been used to camouflage the nasal dorsum including fascia [6], tissue resected from the hump [7], skin grafts [8], alloplastic materials and the more commonly used cartilage [9]. Several authors have used morselized cartilage to conceal irregularities on the nasal dorsum [10],[11],[12],[13].
In the present article, an approach for resection of the hump and restructuring of the nasal dorsum is described. The aim of this technique is to restructure the dorsum anatomy by avoiding palpation of irregularities.
Surgical technique
The septum and dorsum are addressed via open or closed technique (intercartilaginous). The management of the dorsum does not vary by technical approach.
Mucoperichondrium dissection
After the septoplasty, the mucoperichondrium is dissected under the upper lateral cartilages as cephalic as possible [14],[15] (Figure 1).
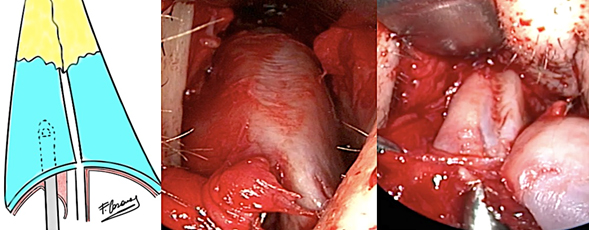
Figure 1: Dissection of the septal mucoperichondrium is continued toward the upper lateral cartilages, performing a lateral semicircular movement to free the mucoperichondrium from the superior aspect of the upper lateral cartilages.
Upper lateral cartilages disarticulation of the septum and nasal bones
Upper lateral cartilages are disarticulated from the septum with scissors or scalpel, then are detached from the nasal bones [14],[15] (Figure 2).
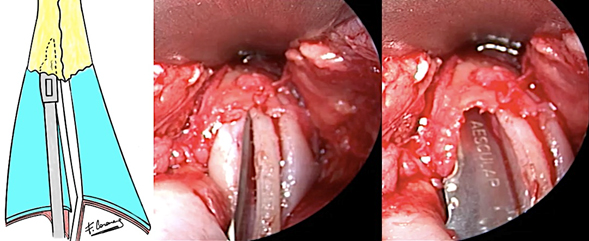
Figure 2: Disarticulation of the upper lateral cartilages of the nasal bones, making semicircular movement toward lateral, respecting upper lateral cartilages portion which is inserted under the bone.
Cartilaginous hump resection: Cartilaginous hump reduction is performed with a scalpel or scissors.
Resection of the bony hump with a coarse rasp. The upper lateral cartilages are folded inward for protection (Figure 3A). The bony hump is resected with a coarse push rasp (Figure 3B).
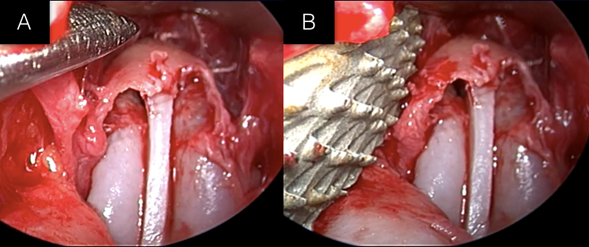
Figure 3: Rasping of the bony hump. 3A Detachment and infolding of the upper lateral cartilages insertion under the nasal bones for protection. 3B Rasping with a coarse rasp.
Smoothing and contouring of nasal bones: This is performed with diamond rasps. Careful sculpting of the nasal bones is performed to both further reduce the hump and smooth any irregularities. The final result should be a smooth and regular dorsum without visual or palpable imperfections (Figure 4). The radix may also be reduced with this technique (Figure 5).
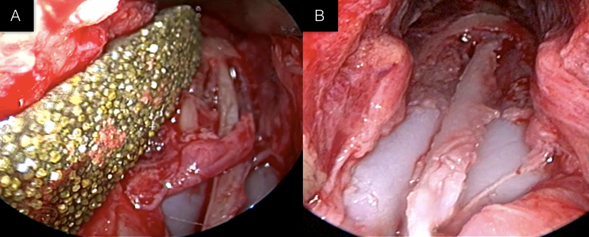
Figure 4A: Contouring of the nasal dorsum with a diamond rasp. 4B: The result is a smooth and soft bony dorsum void of palpable bony irregularities.
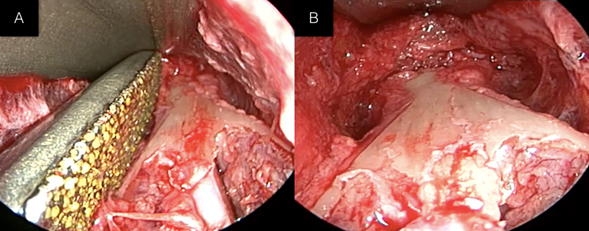
Figure 5A: Sculpting Radix with diamond rasp. 5B: Sculpted radix.
Further contouring following osteotomies: After completion of the osteotomies, palpable bony spicules can be generated; these are contoured leaving a smooth and regular dorsum (Figure 6).
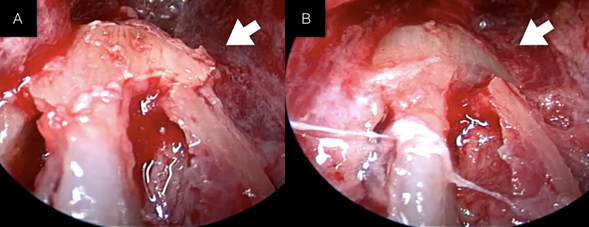
Figure 6: Contouring of bony spicules generated by osteotomies. If they are not properly sculpted, these may result in a visible or palpable irregularity. 6A: Bone spicule. 6B: Contoured spicule with a smooth and soft dorsum.
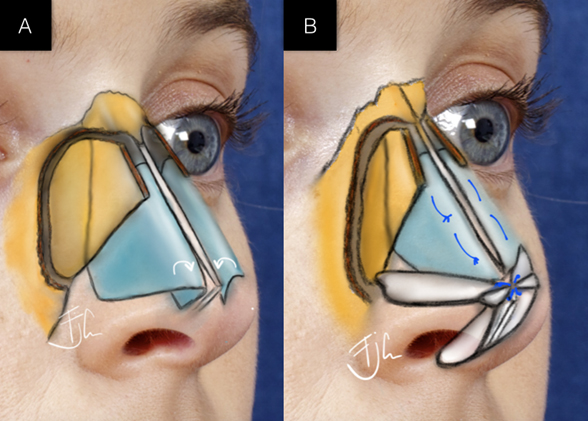
Cartilaginous dorsum closure
the ULC are turned in and sutured to the septal cartilage, functioning as autospreader [14],[15],[16] . Preservation of the cephalic aspect of the upper lateral cartilages that under-ride the nasal bones allow the cartilage to occupy the space between the nasal bones. (Figure 7A, B).
 ULC: upper lateral cartilages
ULC: upper lateral cartilages
Figure 7: Cartilaginous dorsum is closed using the autospreader technique. 7A: The ULC are folded on themselves. 7B: The ULC are sutured to the septum, and the cephalic portions of the ULC fill the area between the nasal bones. This cephalic in-fold prevents excessive medial movement of the nasal bones.
Molding
After closure of the dorsum, there space between the nasal bones is usually palpable. This space can be filled and molded with morselized cartilage (Figure 8 A, B, C).
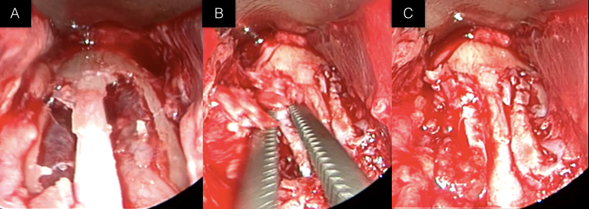
Figure 8A: Residual space between nasal bones is often present after osteotomies. 8B: The space between the nasal bones is filled with morselized cartilage. 8C: After molding of the nasal dorsum.
An additional sheet of thin morselized cartilage in the shape of the dorsum is overlaid, covering any residual imperfections [5] (Figure 9).
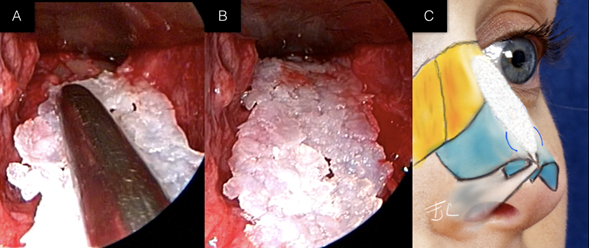
Figures 9A, 9B: Camouflage of the dorsum using a morselized sheet of cartilage. 9C: Ideal placement of the morselized cartilage sheet
Clinical results using the surgical technique described are displayed: Figure 10, 11 and 12.

Figure 10: Clinical outcomes.

Figure 11: Clinical outcomes.

Figure 12: Clinical outcomes of nasal dorsum in oblique view, where appropriate continuity and transition from the bony to cartilaginous region are visualized. There are no stigmas of inverted V, the dorsa are visualized smooth and natural looking.
Discussion
The anatomy of the nasal dorsum is complex, so the restructuring after resection of the hump is a challenge. It is very important to achieve an aesthetically pleasing and natural dorsum, which should feel soft and smooth when touched.
We often find that patients who underwent rhinoplasty complain about the presence of irregularities after palpation of the nasal dorsum including subsidences and bone spicules, among others. These issues are a major cause of secondary rhinoplasty [3],[4],[5], due to an open roof or resection not performed properly [5],[9],[10],[11],[17].
It is essential in the final result the protection and formation of the dorsum aesthetic lines (Figures 10, 11 and 12), because they define the appearance of the dorsum in the frontal and oblique view. This can be achieved by performing an accurate resection of the bony hump, respecting the lateral cartilages and restructuring the anatomy of the nasal dorsum properly (Figure 7).
Multiple camouflage techniques are available for restructuring of the nasal dorsum, but the use of autologous cartilage provides many advantages including minimal resorption, infection and extrusion ranges [18].
Studies with morselized cartilage have exposed its properties as a long-term graft, which shows a direct relationship between the proliferation of chondrocytes and the different degrees of crushed [10],[11]. Light crushed degrees achieve higher levels of chondrocyte proliferation, preserving its viability. While severe degrees of crushed inhibit chondrocyte proliferation altering the viability and obtaining an unpredictable loss of volume graft [10],[11]. Therefore, a graft from mild to moderate crushed grade, delivers excellent tool adjustment, filler and camouflage on the nasal dorsum [5] (Figure 9).
From the author perspective, in order to avoid the apparition of irregularities on the dorsum, there are three key steps: 1. Sculpting of nasal bones with diamond rasp will provide a more regular surface by eliminating bony spicules (Figure 6); 2. Use of morselized cartilage sheet as camouflage (Figure 9); 3. Use of autospreader (Figure 7) as the upper lateral cartilage is protected; this subsequently fills the open roof area between the nasal bones, especially in the osteochondral joint area.
Conclusion
The anatomy of the nasal dorsum following resection of the hump must be structured properly. Thereby we avoid any palpation of irregularities and an adequate cosmetic result is achieved.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
Informed consent forms, requested by Medwave, have been signed by the patients. A copy of each was sent to the editorship of the Journal.
Conflicts of interest
The authors completed the ICMJE conflict of interest declaration form, translated into Spanish by Medwave, and declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years, and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Funding
The authors declare there were no financing from external sources.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Las complicaciones de un inadecuado manejo del dorso nasal son frecuentes, destacando entre estas la palpación de irregularidades, debido a que en el manejo de la giba nasal se utilizan técnicas resectivas. Se describe una técnica quirúrgica para el manejo del dorso nasal, con énfasis en evitar irregularidades. Los pasos claves para evitar la palpación de irregularidades son: el uso de raspa diamantada, autoespaciador y lámina de cartílago morcelizado como camuflaje. Posterior a la resección de la giba se debe reestructurar de forma adecuada la anatomía del dorso nasal, de esta forma lograremos un resultado estético adecuado e idealmente evitar irregularidades a la palpación.
 Autores:
Fernando Javier Casanueva [1], Felipe Cardemil [2,3 ]
Autores:
Fernando Javier Casanueva [1], Felipe Cardemil [2,3 ]
Affiliation:
[1] Servicio Otorrinolaringología, Hospital San Vicente de Arauco, Concepción, Chile
[2] Servicio Otorrinolaringología, Hospital San Juan de Dios, Universidad de Chile, Santiago, Chile
[3] Servicio Otorrinolaringología, Clínica Las Condes, Santiago, Chile
E-mail: fjcasanueva@gmail.com
Author address:
[1] 0677 South West
Lowell Street
Portland
Oregon
USA

Citation: Casanueva FJ , Cardemil F . Avoiding irregularities on the nasal dorsum in rhinoplasty. Medwave 2016 Mar;16(2):e6416 doi: 10.5867/medwave.2016.02.6416
Submission date: 22/2/2016
Acceptance date: 15/3/2016
Publication date: 30/3/2016
Origin: not requested

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Rohrich RJ, Muzaffar AR, Janis JE. Component dorsal hump reduction: the importance of maintaining dorsal aesthetic lines in rhinoplasty. Plast Reconstr Surg. 2004 Oct;114(5):1298-308; discussion 1309-12. | PubMed |
- de Pochat VD, Alonso N, Ribeiro EB, da Rocha EA, Tenório EG, Meneses JV. Anatomical variations of the upper lateral cartilages and their implications in rhinoplasty. Aesthetic Plast Surg. 2012 Apr;36(2):285-9. | CrossRef | PubMed |
- Sheen JH. Spreader graft: a method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plast Reconstr Surg. 1984 Feb;73(2):230-9. | PubMed |
- Palhazi P, Daniel RK, Kosins AM. The osseocartilaginous vault of the nose: anatomy and surgical observations. Aesthet Surg J. 2015 Mar;35(3):242-51. | CrossRef | PubMed |
- Cakmak O, Buyuklu F. Crushed cartilage grafts for concealing irregularities in rhinoplasty. Arch Facial Plast Surg. 2007 Sep-Oct;9(5):352-7. | PubMed |
- Skoog T. A method of hump reduction in rhinoplasty. A technique for preservation of the nasal roof. Arch Otolaryngol. 1966 Mar;83(3):283-7. | PubMed |
- Reich J. The application of dermis grafts in deformities of the nose. Plast Reconstr Surg. 1983 Jun;71(6):772-82. | PubMed |
- Baker TM, Courtiss EH. Temporalis fascia grafts in open secondary rhinoplasty. Plast Reconstr Surg. 1994 Apr;93(4):802-10. | PubMed |
- McKinney P, Loomis MG, Wiedrich TA. Reconstruction of the nasal cap with a thin septal graft. Plast Reconstr Surg. 1993 Aug;92(2):346-51. | PubMed |
- Cakmak O, Bircan S, Buyuklu F, Tuncer I, Dal T, Ozluoglu LN. Viability of crushed and diced cartilage grafts: a study in rabbits. Arch Facial Plast Surg. 2005 Jan-Feb;7(1):21-6. | PubMed |
- Cakmak O, Buyuklu F, Yilmaz Z, Sahin FI, Tarhan E, Ozluoglu LN. Viability of cultured human nasal septum chondrocytes after crushing. Arch Facial Plast Surg. 2005 Nov-Dec;7(6):406-9. | CrossRef | PubMed |
- Hamra ST. Crushed cartilage grafts over alar dome reduction in open rhinoplasty. Plast Reconstr Surg. 1993 Aug;92(2):352-6. | PubMed |
- Stoksted P, Ladefoged C. Crushed cartilage in nasal reconstruction. J Laryngol Otol. 1986 Aug;100(8):897-906. | PubMed |
- Casanueva F, Astudillo D, Santamaría A, Cardemil F. Autoespaciador en rinoplastía abierta y cerrada. Rev. Otorrinolaringol. Cir. Cabeza Cuello 2015; 75: 106-113. | Link |
- Gruber RP, Park E, Newman J, Berkowitz L, Oneal R. The spreader flap in primary rhinoplasty. Plast Reconstr Surg. 2007 May;119(6):1903-10. | PubMed |
- Eren SB, Tugrul S, Ozucer B, Meric A. Autospreading Spring Flap Technique for Reconstruction of the MiddleVault. Aesthetic Plast Surg. 2014 Apr;38(2):322-8.
- Sheen JH. The ideal dorsal graft: a continuing quest. Plast Reconstr Surg.1998 Dec;102(7):2490-3. | PubMed |
- Parker Porter J. Grafts in rhinoplasty: alloplastic vs. autogenous. Arch Otolaryngol Head Neck Surg. 2000 Apr;126(4):558-61. | PubMed |
 Rohrich RJ, Muzaffar AR, Janis JE. Component dorsal hump reduction: the importance of maintaining dorsal aesthetic lines in rhinoplasty. Plast Reconstr Surg. 2004 Oct;114(5):1298-308; discussion 1309-12. | PubMed |
Rohrich RJ, Muzaffar AR, Janis JE. Component dorsal hump reduction: the importance of maintaining dorsal aesthetic lines in rhinoplasty. Plast Reconstr Surg. 2004 Oct;114(5):1298-308; discussion 1309-12. | PubMed | de Pochat VD, Alonso N, Ribeiro EB, da Rocha EA, Tenório EG, Meneses JV. Anatomical variations of the upper lateral cartilages and their implications in rhinoplasty. Aesthetic Plast Surg. 2012 Apr;36(2):285-9. | CrossRef | PubMed |
de Pochat VD, Alonso N, Ribeiro EB, da Rocha EA, Tenório EG, Meneses JV. Anatomical variations of the upper lateral cartilages and their implications in rhinoplasty. Aesthetic Plast Surg. 2012 Apr;36(2):285-9. | CrossRef | PubMed | Sheen JH. Spreader graft: a method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plast Reconstr Surg. 1984 Feb;73(2):230-9. | PubMed |
Sheen JH. Spreader graft: a method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plast Reconstr Surg. 1984 Feb;73(2):230-9. | PubMed | Palhazi P, Daniel RK, Kosins AM. The osseocartilaginous vault of the nose: anatomy and surgical observations. Aesthet Surg J. 2015 Mar;35(3):242-51. | CrossRef | PubMed |
Palhazi P, Daniel RK, Kosins AM. The osseocartilaginous vault of the nose: anatomy and surgical observations. Aesthet Surg J. 2015 Mar;35(3):242-51. | CrossRef | PubMed | Cakmak O, Buyuklu F. Crushed cartilage grafts for concealing irregularities in rhinoplasty. Arch Facial Plast Surg. 2007 Sep-Oct;9(5):352-7. | PubMed |
Cakmak O, Buyuklu F. Crushed cartilage grafts for concealing irregularities in rhinoplasty. Arch Facial Plast Surg. 2007 Sep-Oct;9(5):352-7. | PubMed | Skoog T. A method of hump reduction in rhinoplasty. A technique for preservation of the nasal roof. Arch Otolaryngol. 1966 Mar;83(3):283-7. | PubMed |
Skoog T. A method of hump reduction in rhinoplasty. A technique for preservation of the nasal roof. Arch Otolaryngol. 1966 Mar;83(3):283-7. | PubMed | Reich J. The application of dermis grafts in deformities of the nose. Plast Reconstr Surg. 1983 Jun;71(6):772-82. | PubMed |
Reich J. The application of dermis grafts in deformities of the nose. Plast Reconstr Surg. 1983 Jun;71(6):772-82. | PubMed | Baker TM, Courtiss EH. Temporalis fascia grafts in open secondary rhinoplasty. Plast Reconstr Surg. 1994 Apr;93(4):802-10. | PubMed |
Baker TM, Courtiss EH. Temporalis fascia grafts in open secondary rhinoplasty. Plast Reconstr Surg. 1994 Apr;93(4):802-10. | PubMed | McKinney P, Loomis MG, Wiedrich TA. Reconstruction of the nasal cap with a thin septal graft. Plast Reconstr Surg. 1993 Aug;92(2):346-51. | PubMed |
McKinney P, Loomis MG, Wiedrich TA. Reconstruction of the nasal cap with a thin septal graft. Plast Reconstr Surg. 1993 Aug;92(2):346-51. | PubMed | Cakmak O, Bircan S, Buyuklu F, Tuncer I, Dal T, Ozluoglu LN. Viability of crushed and diced cartilage grafts: a study in rabbits. Arch Facial Plast Surg. 2005 Jan-Feb;7(1):21-6. | PubMed |
Cakmak O, Bircan S, Buyuklu F, Tuncer I, Dal T, Ozluoglu LN. Viability of crushed and diced cartilage grafts: a study in rabbits. Arch Facial Plast Surg. 2005 Jan-Feb;7(1):21-6. | PubMed | Cakmak O, Buyuklu F, Yilmaz Z, Sahin FI, Tarhan E, Ozluoglu LN. Viability of cultured human nasal septum chondrocytes after crushing. Arch Facial Plast Surg. 2005 Nov-Dec;7(6):406-9. | CrossRef | PubMed |
Cakmak O, Buyuklu F, Yilmaz Z, Sahin FI, Tarhan E, Ozluoglu LN. Viability of cultured human nasal septum chondrocytes after crushing. Arch Facial Plast Surg. 2005 Nov-Dec;7(6):406-9. | CrossRef | PubMed | Hamra ST. Crushed cartilage grafts over alar dome reduction in open rhinoplasty. Plast Reconstr Surg. 1993 Aug;92(2):352-6. | PubMed |
Hamra ST. Crushed cartilage grafts over alar dome reduction in open rhinoplasty. Plast Reconstr Surg. 1993 Aug;92(2):352-6. | PubMed | Stoksted P, Ladefoged C. Crushed cartilage in nasal reconstruction. J Laryngol Otol. 1986 Aug;100(8):897-906. | PubMed |
Stoksted P, Ladefoged C. Crushed cartilage in nasal reconstruction. J Laryngol Otol. 1986 Aug;100(8):897-906. | PubMed | Casanueva F, Astudillo D, Santamaría A, Cardemil F. Autoespaciador en rinoplastía abierta y cerrada. Rev. Otorrinolaringol. Cir. Cabeza Cuello 2015; 75: 106-113. | Link |
Casanueva F, Astudillo D, Santamaría A, Cardemil F. Autoespaciador en rinoplastía abierta y cerrada. Rev. Otorrinolaringol. Cir. Cabeza Cuello 2015; 75: 106-113. | Link | Gruber RP, Park E, Newman J, Berkowitz L, Oneal R. The spreader flap in primary rhinoplasty. Plast Reconstr Surg. 2007 May;119(6):1903-10. | PubMed |
Gruber RP, Park E, Newman J, Berkowitz L, Oneal R. The spreader flap in primary rhinoplasty. Plast Reconstr Surg. 2007 May;119(6):1903-10. | PubMed | Eren SB, Tugrul S, Ozucer B, Meric A. Autospreading Spring Flap Technique for Reconstruction of the MiddleVault. Aesthetic Plast Surg. 2014 Apr;38(2):322-8.
Eren SB, Tugrul S, Ozucer B, Meric A. Autospreading Spring Flap Technique for Reconstruction of the MiddleVault. Aesthetic Plast Surg. 2014 Apr;38(2):322-8.  Sheen JH. The ideal dorsal graft: a continuing quest. Plast Reconstr Surg.1998 Dec;102(7):2490-3. | PubMed |
Sheen JH. The ideal dorsal graft: a continuing quest. Plast Reconstr Surg.1998 Dec;102(7):2490-3. | PubMed | Parker Porter J. Grafts in rhinoplasty: alloplastic vs. autogenous. Arch Otolaryngol Head Neck Surg. 2000 Apr;126(4):558-61. | PubMed |
Parker Porter J. Grafts in rhinoplasty: alloplastic vs. autogenous. Arch Otolaryngol Head Neck Surg. 2000 Apr;126(4):558-61. | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








