Key Words: Post-mastectomy radiotherapy, Autologous breast reconstruction, Prosthetic breast reconstruction, postoperative morbidity, Epistemonikos, GRADE.
Abstract
INTRODUCTION
Radiotherapy is frequently used after breast reconstruction in patients with locally advanced breast cancer or metastases in axillary lymph nodes. However, there might be differences between autologous and prosthetic reconstruction in terms of effectiveness and safety of post-reconstruction radiotherapy.
METHODS
To answer this question we searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified five systematic reviews including nine primary studies overall, of which all were observational studies. We concluded that in patients who will undergo post reconstructive radiotherapy, autologous breast reconstruction could reduce reoperations due to general complications compared to prosthetic breast reconstruction. However, it probably increases the risk of skin or flap necrosis. It is not clear whether there are differences in other outcomes as the certainty of evidence has been assessed as very low.
Problem
In 2017, 252,710 women were diagnosed with invasive breast cancer in the United States. It is estimated that over a third would undergo a total mastectomy, and 32% of them to breast reconstruction surgery [1],[2],[3]. There are two main techniques for breast reconstruction: autologous breast reconstruction with pedicled myocutaneous flaps or microsurgical free flaps, and prosthetic reconstruction, either with tissue expanders or definitive implants [4]. Once breast reconstruction has been conducted in locally advanced breast cancer or with metastatic involvement of axillary lymph nodes, it is common practice to apply radiotherapy, since it would reduce loco-regional recurrence and increase disease-free survival [5]. However, this can also negatively affect the results of breast reconstruction, with worse aesthetic results, need for post-radiation reoperation and even failure of breast reconstruction [6]. So, it has been proposed that depending on the type of breast reconstruction conducted prior to radiotherapy, different results could be obtained in relation to the final aesthetic reconstruction.
Methods
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found five systematic reviews [6],[7],[8],[9],[10] that included nine primary studies overall [11],[12],[13],[14],[15],[16],[17],[18],[19], of which all corresponded to observational studies. Three non-comparative studies were excluded from this summary [12],[16],[18]. This table and general summary are based in six observational studies [11],[13],[14],[15],[17],[19] as no randomized trials were found that answered the question of interest. |
|
What types of patients were included* |
The effect of radiotherapy on breast reconstruction was evaluated for both groups. Six studies evaluated patients with post reconstructive radiotherapy [11],[13],[14],[15],[17],[19] and two of these studies also included patients with pre reconstruction radiotherapy [11],[15], whose subgroup was not considered for the analysis. No study described the average dose of radiotherapy used in patients. Two studies reported confusing potential variables such as body mass index, smoking habit or diabetes [11],[15], while four did not report it. |
|
What types of interventions were included* |
In relation to breast reconstruction, three studies included patients with primary breast reconstruction [11],[15],[19] and three studies did not specify it [13],[14],[17]. In relation to type of reconstruction, six studies compared tissue expander/implant against autologous tissue. Of the latter, one study included autologous reconstruction with pedicled transverse rectus abdominis myocutaneous (TRAM) flap [15], two studies included TRAM flap not specified [11],[19] and three studies did not reported the type of autologous reconstruction [13],[14],[17]. |
|
What types of outcomes |
The studies measured multiple outcomes that were organized by the systematic reviews as follows:
The average follow-up of the studies was 30 months with a range between 1 and 153 months. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
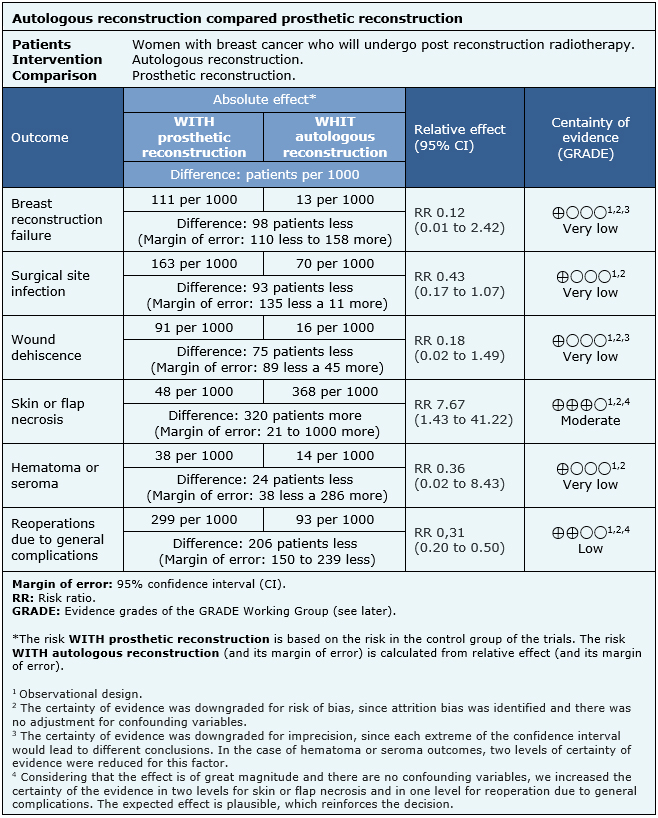
Summary of findings
The information on the effects of autologous breast reconstruction versus prosthetic reconstruction in women with breast cancer who will undergo post reconstructive radiotherapy is based on six observational cohort studies including 478 patients in total.One study reported the outcome reconstruction failure (48 patients) [15], five studies reported surgical site infection (337 patients) [11],[13],[14],[15],[19], two studies reported wound dehiscence (98 patients) [15],[19], three studies reported skin or flap necrosis (183 patients) [11],[15],[19], one study reported hematoma or seroma (50 patients) [19] and five studies reported reoperation due to general complications (428 patients) [11],[13],[14],[15],[17].
The summary of findings is as follows:
- We are uncertain whether autologous breast reconstruction compared to prosthetic breast reconstruction reduces breast reconstruction failure in patients who underwent post reconstructive radiotherapy, as the certainty of the evidence has been assessed as very low.
- We are uncertain whether autologous breast reconstruction compared to prosthetic breast reconstruction reduces surgical site infection in patients who underwent post reconstructive radiotherapy, as the certainty of the evidence has been assessed as very low.
- We are uncertain whether autologous breast reconstruction compared to prosthetic breast reconstruction reduces wound dehiscence in patients who underwent post reconstructive radiotherapy, as the certainty of the evidence has been assessed as very low.
- Autologous breast reconstruction compared to prosthetic breast reconstruction probably increases skin or flap necrosis in patients who underwent post reconstructive radiotherapy (moderate certainty of evidence).
- We are uncertain whether autologous breast reconstruction compared to prosthetic breast reconstruction reduces hematoma or seroma in patients who underwent post reconstructive radiotherapy, as the certainty of the evidence has been assessed as very low.
- Autologous breast reconstruction compared to prosthetic breast reconstruction may reduce reoperations due to general complications in patients who underwent post reconstructive radiotherapy (low certainty of evidence).
|
Follow the link to access the interactive version of this table (Interactive Summary of Findings - iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
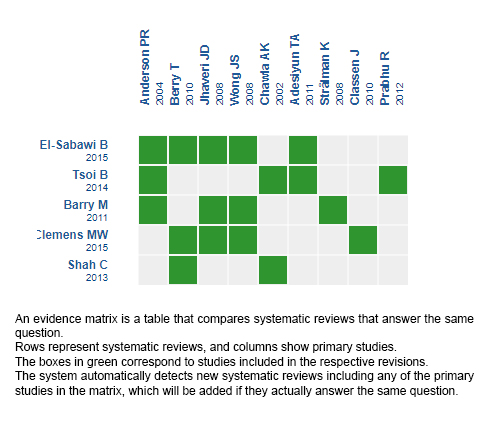
Follow the link to access the interactive version: Autologous reconstruction versus prosthetic reconstruction in women who will undergo radiotherapy post reconstruction.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
La radioterapia se utiliza cada vez con más frecuencia después de la reconstrucción mamaria en pacientes con cáncer de mama localmente avanzado o con metástasis en linfonodos axilares. Sin embargo, se ha propuesto que podrían existir diferencias en la efectividad y seguridad de la radioterapia post reconstrucción dependiendo de qué tipo de reconstrucción mamaria se utilice, ya sea esta reconstrucción autóloga o protésica.
MÉTODOS
Para responder esta pregunta utilizamos Epistemonikos, la mayor base de datos de revisiones sistemáticas en salud, la cual es mantenida mediante búsquedas en múltiples fuentes de información, incluyendo MEDLINE, EMBASE, Cochrane, entre otras. Extrajimos los datos desde las revisiones identificadas, re analizamos los datos de los estudios primarios, realizamos un metanálisis y preparamos una tabla de resumen de los resultados utilizando el método GRADE.
RESULTADOS Y CONCLUSIONES
Identificamos cinco revisiones sistemáticas que en conjunto incluyeron nueve estudios primarios, todos los cuales corresponden a estudios observacionales. Concluimos que la reconstrucción mamaria autóloga podría disminuir las reoperaciones atribuidas a complicaciones generales en comparación a la reconstrucción mamaria protésica en pacientes sometidas a radioterapia post reconstrucción, pero probablemente aumenta el riesgo de necrosis de piel o colgajo. No está claro si existen diferencias en otros desenlaces, debido a que la certeza de la evidencia ha sido evaluada como muy baja.
 Authors:
Francisco Rubilar[1,2], Alfonso Navia[2,3], Bruno Dagnino[2,3]
Authors:
Francisco Rubilar[1,2], Alfonso Navia[2,3], Bruno Dagnino[2,3]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Sección de Cirugía Plástica y Reconstructiva, División de Cirugía, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Centro Evidencia UC
E-mail: bdagnino@med.puc.cl
Author address:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Diagonal Paraguay 476 Santiago Chile

Citation: Rubilar F, Navia A, Dagnino B. Autologous versus prosthetic reconstruction for women with breast cancer who will undergo post-reconstruction radiotherapy. Medwave 2019;19(10):e7727 doi: 10.5867/medwave.2019.11.7727
Submission date: 4/12/2018
Acceptance date: 28/12/2018
Publication date: 29/11/2019
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Epistemonikos Evidence Synthesis Project.
Errata
1. Part of the content was corrected | Link |

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015 Jan;150(1):9-16. | PubMed |
- Agarwal S, Kidwell KM, Farberg A, Kozlow JH, Chung KC, Momoh AO. Immediate Reconstruction of the Radiated Breast: Recent Trends Contrary to Traditional Standards. Ann Surg Oncol. 2015 Aug;22(8):2551-9. | CrossRef | PubMed | PMC |
- Frasier LL, Holden S, Holden T, Schumacher JR, Leverson G, Anderson B, Greenberg CC, Neuman HB. Temporal Trends in Postmastectomy Radiation Therapy and Breast Reconstruction Associated With Changes in National Comprehensive Cancer Network Guidelines. JAMA Oncol. 2016 Jan;2(1):95-101. | CrossRef | PubMed | PMC |
- Kronowitz SJ, Hunt KK, Kuerer HM, Babiera G, McNeese MD, Buchholz TA, Strom EA, Robb GL. Delayed-immediate breast reconstruction. Plast Reconstr Surg. 2004 May;113(6):1617-28. | PubMed |
- Truong PT, Woodward WA, Bucholz TA Optimizing locoregional control and survival for women with breast cancer: a review of current developments in postmastectomy radiation. Expert Rev Anticancer Ther. 2006; 6:205–216.
- Clemens MW, Kronowitz SJ. Current perspectives on radiation therapy in autologous and prosthetic breast reconstruction. Gland Surg. 2015 Jun;4(3):222-31. | CrossRef | PubMed | PMC |
- Shah C, Kundu N, Arthur D, Vicini F. Radiation therapy following postmastectomy reconstruction: a systematic review. Ann Surg Oncol. 2013 Apr;20(4):1313-22. | CrossRef | PubMed |
- Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O'Reilly D, Goeree R. Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. Plast Reconstr Surg. 2014 Feb;133(2):234-49. | CrossRef | PubMed |
- El-Sabawi B, Sosin M, Carey JN, Nahabedian MY, Patel KM. Breast reconstruction and adjuvant therapy: A systematic review of surgical outcomes. J Surg Oncol. 2015 Oct;112(5):458-64. | CrossRef | PubMed |
- Barry M, Kell MR. Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat. 2011 May;127(1):15-22. | CrossRef | PubMed |
- Anderson PR, Hanlon AL, Fowble BL, McNeeley SW, Freedman GM. Low complication rates are achievable after postmastectomy breast reconstruction and radiation therapy. Int J Radiat Oncol Biol Phys. 2004 Jul 15;59(4):1080-7. | PubMed |
- Berry T, Brooks S, Sydow N, Djohan R, Nutter B, Lyons J, Dietz J. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010 Oct;17 Suppl 3:202-10. | CrossRef | PubMed |
- Strålman K, Mollerup CL, Kristoffersen US, Elberg JJ. Long-term outcome after mastectomy with immediate breast reconstruction. Acta Oncol. 2008;47(4):704-8. | CrossRef | PubMed |
- Jhaveri JD, Rush SC, Kostroff K, Derisi D, Farber LA, Maurer VE, Bosworth JL. Clinical outcomes of postmastectomy radiation therapy after immediate breast reconstruction. Int J Radiat Oncol Biol Phys. 2008 Nov 1;72(3):859-65. | CrossRef | PubMed |
- Chawla AK, Kachnic LA, Taghian AG, Niemierko A, Zapton DT, Powell SN. Radiotherapy and breast reconstruction: complications and cosmesis with TRAM versus tissue expander/implant. Int J Radiat Oncol Biol Phys. 2002 Oct 1;54(2):520-6. | CrossRef |
- Adesiyun TA, Lee BT, Yueh JH, Chen C, Colakoglu S, Anderson KE, Nguyen MD, Recht A. Impact of sequencing of postmastectomy radiotherapy and breast reconstruction on timing and rate of complications and patient satisfaction. Int J Radiat Oncol Biol Phys. 2011 Jun 1;80(2):392-7. | CrossRef | PubMed |
- Wong JS, Ho AY, Kaelin CM, Bishop KL, Silver B, Gelman R, Harris JR, Hergrueter CA. Incidence of major corrective surgery after post-mastectomy breast reconstruction and radiation therapy. Breast J. 2008 Jan-Feb;14(1):49-54. | CrossRef | PubMed |
- Classen J, Nitzsche S, Wallwiener D, Kristen P, Souchon R, Bamberg M, Brucker S. Fibrotic changes after postmastectomy radiotherapy and reconstructive surgery in breast cancer. A retrospective analysis in 109 patients. Strahlenther Onkol.2010 Nov;186(11):630-6. | CrossRef | PubMed |
- Prabhu R, Godette K, Carlson G, Losken A, Gabram S, Fasola C, O'Regan R, Zelnak A, Torres M. The impact of skin-sparing mastectomy with immediate reconstruction in patients with Stage III breast cancer treated with neoadjuvant chemotherapy and postmastectomy radiation. Int J Radiat Oncol Biol Phys. 2012 Mar 15;82(4):e587-93. | CrossRef | PubMed |
- Potter S, Brigic A, Whiting PF, Cawthorn SJ, Avery KN, Donovan JL, Blazeby JM. Reporting clinical outcomes of breast reconstruction: a systematic review. J Natl Cancer Inst. 2011 Jan 5;103(1):31-46. | CrossRef | PubMed |
- Ho AY, Hu ZI, Mehrara BJ, Wilkins EG. Radiotherapy in the setting of breast reconstruction: types, techniques, and timing. Lancet Oncol. 2017 Dec;18(12):e742-e753. | CrossRef | PubMed |
 Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide trends in
mastectomy for early-stage breast cancer. JAMA Surg. 2015 Jan;150(1):9-16.
| PubMed |
Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide trends in
mastectomy for early-stage breast cancer. JAMA Surg. 2015 Jan;150(1):9-16.
| PubMed | Agarwal S, Kidwell KM, Farberg A, Kozlow JH, Chung KC, Momoh AO. Immediate
Reconstruction of the Radiated Breast: Recent Trends Contrary to Traditional
Standards. Ann Surg Oncol. 2015 Aug;22(8):2551-9. | CrossRef | PubMed | PMC |
Agarwal S, Kidwell KM, Farberg A, Kozlow JH, Chung KC, Momoh AO. Immediate
Reconstruction of the Radiated Breast: Recent Trends Contrary to Traditional
Standards. Ann Surg Oncol. 2015 Aug;22(8):2551-9. | CrossRef | PubMed | PMC | Frasier LL, Holden S, Holden T, Schumacher JR, Leverson G, Anderson B,
Greenberg CC, Neuman HB. Temporal Trends in Postmastectomy Radiation Therapy and
Breast Reconstruction Associated With Changes in National Comprehensive Cancer
Network Guidelines. JAMA Oncol. 2016 Jan;2(1):95-101.
| CrossRef | PubMed | PMC |
Frasier LL, Holden S, Holden T, Schumacher JR, Leverson G, Anderson B,
Greenberg CC, Neuman HB. Temporal Trends in Postmastectomy Radiation Therapy and
Breast Reconstruction Associated With Changes in National Comprehensive Cancer
Network Guidelines. JAMA Oncol. 2016 Jan;2(1):95-101.
| CrossRef | PubMed | PMC | Kronowitz SJ, Hunt KK, Kuerer HM, Babiera G, McNeese MD, Buchholz TA, Strom EA, Robb GL. Delayed-immediate breast reconstruction. Plast Reconstr Surg. 2004 May;113(6):1617-28. | PubMed |
Kronowitz SJ, Hunt KK, Kuerer HM, Babiera G, McNeese MD, Buchholz TA, Strom EA, Robb GL. Delayed-immediate breast reconstruction. Plast Reconstr Surg. 2004 May;113(6):1617-28. | PubMed | Truong PT, Woodward WA, Bucholz TA Optimizing locoregional control and survival for women with breast cancer: a review of current developments in postmastectomy radiation. Expert Rev Anticancer Ther. 2006; 6:205–216.
Truong PT, Woodward WA, Bucholz TA Optimizing locoregional control and survival for women with breast cancer: a review of current developments in postmastectomy radiation. Expert Rev Anticancer Ther. 2006; 6:205–216.  Clemens MW, Kronowitz SJ. Current perspectives on radiation therapy in autologous and prosthetic breast reconstruction. Gland Surg. 2015 Jun;4(3):222-31. | CrossRef | PubMed | PMC |
Clemens MW, Kronowitz SJ. Current perspectives on radiation therapy in autologous and prosthetic breast reconstruction. Gland Surg. 2015 Jun;4(3):222-31. | CrossRef | PubMed | PMC | Shah C, Kundu N, Arthur D, Vicini F. Radiation therapy following postmastectomy reconstruction: a systematic review. Ann Surg Oncol. 2013 Apr;20(4):1313-22. | CrossRef | PubMed |
Shah C, Kundu N, Arthur D, Vicini F. Radiation therapy following postmastectomy reconstruction: a systematic review. Ann Surg Oncol. 2013 Apr;20(4):1313-22. | CrossRef | PubMed | Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O'Reilly D, Goeree R. Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. Plast Reconstr Surg. 2014 Feb;133(2):234-49. | CrossRef | PubMed |
Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O'Reilly D, Goeree R. Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. Plast Reconstr Surg. 2014 Feb;133(2):234-49. | CrossRef | PubMed | El-Sabawi B, Sosin M, Carey JN, Nahabedian MY, Patel KM. Breast reconstruction and adjuvant therapy: A systematic review of surgical outcomes. J Surg Oncol. 2015 Oct;112(5):458-64. | CrossRef | PubMed |
El-Sabawi B, Sosin M, Carey JN, Nahabedian MY, Patel KM. Breast reconstruction and adjuvant therapy: A systematic review of surgical outcomes. J Surg Oncol. 2015 Oct;112(5):458-64. | CrossRef | PubMed | Barry M, Kell MR. Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat. 2011 May;127(1):15-22. | CrossRef | PubMed |
Barry M, Kell MR. Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat. 2011 May;127(1):15-22. | CrossRef | PubMed | Anderson PR, Hanlon AL, Fowble BL, McNeeley SW, Freedman GM. Low complication rates are achievable after postmastectomy breast reconstruction and radiation therapy. Int J Radiat Oncol Biol Phys. 2004 Jul 15;59(4):1080-7. | PubMed |
Anderson PR, Hanlon AL, Fowble BL, McNeeley SW, Freedman GM. Low complication rates are achievable after postmastectomy breast reconstruction and radiation therapy. Int J Radiat Oncol Biol Phys. 2004 Jul 15;59(4):1080-7. | PubMed | Berry T, Brooks S, Sydow N, Djohan R, Nutter B, Lyons J, Dietz J. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010 Oct;17 Suppl 3:202-10. | CrossRef | PubMed |
Berry T, Brooks S, Sydow N, Djohan R, Nutter B, Lyons J, Dietz J. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010 Oct;17 Suppl 3:202-10. | CrossRef | PubMed | Strålman K, Mollerup CL, Kristoffersen US, Elberg JJ. Long-term outcome after mastectomy with immediate breast reconstruction. Acta Oncol. 2008;47(4):704-8. | CrossRef | PubMed |
Strålman K, Mollerup CL, Kristoffersen US, Elberg JJ. Long-term outcome after mastectomy with immediate breast reconstruction. Acta Oncol. 2008;47(4):704-8. | CrossRef | PubMed | Jhaveri JD, Rush SC, Kostroff K, Derisi D, Farber LA, Maurer VE, Bosworth JL. Clinical outcomes of postmastectomy radiation therapy after immediate breast reconstruction. Int J Radiat Oncol Biol Phys. 2008 Nov 1;72(3):859-65. | CrossRef | PubMed |
Jhaveri JD, Rush SC, Kostroff K, Derisi D, Farber LA, Maurer VE, Bosworth JL. Clinical outcomes of postmastectomy radiation therapy after immediate breast reconstruction. Int J Radiat Oncol Biol Phys. 2008 Nov 1;72(3):859-65. | CrossRef | PubMed | Chawla AK, Kachnic LA, Taghian AG, Niemierko A, Zapton DT, Powell SN. Radiotherapy and breast reconstruction: complications and cosmesis with TRAM versus tissue expander/implant. Int J Radiat Oncol Biol Phys. 2002 Oct 1;54(2):520-6. | CrossRef |
Chawla AK, Kachnic LA, Taghian AG, Niemierko A, Zapton DT, Powell SN. Radiotherapy and breast reconstruction: complications and cosmesis with TRAM versus tissue expander/implant. Int J Radiat Oncol Biol Phys. 2002 Oct 1;54(2):520-6. | CrossRef | Adesiyun TA, Lee BT, Yueh JH, Chen C, Colakoglu S, Anderson KE, Nguyen MD, Recht A. Impact of sequencing of postmastectomy radiotherapy and breast reconstruction on timing and rate of complications and patient satisfaction. Int J Radiat Oncol Biol Phys. 2011 Jun 1;80(2):392-7. | CrossRef | PubMed |
Adesiyun TA, Lee BT, Yueh JH, Chen C, Colakoglu S, Anderson KE, Nguyen MD, Recht A. Impact of sequencing of postmastectomy radiotherapy and breast reconstruction on timing and rate of complications and patient satisfaction. Int J Radiat Oncol Biol Phys. 2011 Jun 1;80(2):392-7. | CrossRef | PubMed | Wong JS, Ho AY, Kaelin CM, Bishop KL, Silver B, Gelman R, Harris JR, Hergrueter CA. Incidence of major corrective surgery after post-mastectomy breast reconstruction and radiation therapy. Breast J. 2008 Jan-Feb;14(1):49-54. | CrossRef | PubMed |
Wong JS, Ho AY, Kaelin CM, Bishop KL, Silver B, Gelman R, Harris JR, Hergrueter CA. Incidence of major corrective surgery after post-mastectomy breast reconstruction and radiation therapy. Breast J. 2008 Jan-Feb;14(1):49-54. | CrossRef | PubMed | Classen J, Nitzsche S, Wallwiener D, Kristen P, Souchon R, Bamberg M, Brucker S. Fibrotic changes after postmastectomy radiotherapy and reconstructive surgery in breast cancer. A retrospective analysis in 109 patients. Strahlenther Onkol.2010 Nov;186(11):630-6. | CrossRef | PubMed |
Classen J, Nitzsche S, Wallwiener D, Kristen P, Souchon R, Bamberg M, Brucker S. Fibrotic changes after postmastectomy radiotherapy and reconstructive surgery in breast cancer. A retrospective analysis in 109 patients. Strahlenther Onkol.2010 Nov;186(11):630-6. | CrossRef | PubMed | Prabhu R, Godette K, Carlson G, Losken A, Gabram S, Fasola C, O'Regan R, Zelnak A, Torres M. The impact of skin-sparing mastectomy with immediate reconstruction in patients with Stage III breast cancer treated with neoadjuvant chemotherapy and postmastectomy radiation. Int J Radiat Oncol Biol Phys. 2012 Mar 15;82(4):e587-93. | CrossRef | PubMed |
Prabhu R, Godette K, Carlson G, Losken A, Gabram S, Fasola C, O'Regan R, Zelnak A, Torres M. The impact of skin-sparing mastectomy with immediate reconstruction in patients with Stage III breast cancer treated with neoadjuvant chemotherapy and postmastectomy radiation. Int J Radiat Oncol Biol Phys. 2012 Mar 15;82(4):e587-93. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








