Key Words: Pneumatic retinopexy, rhegmatogenous retinal detachment, Epistemonikos, GRADE.
Abstract
INTRODUCTION
Rhegmatogenous retinal detachment is caused by a tear in the retina and is a frequent cause of vision loss. Its treatment is mainly surgical and the following alternatives can be identified: scleral buckling or classic surgery, pneumatic retinopexy and vitrectomy. Between the first two options, most professionals prefer scleral buckling over pneumatic retinopexy, but the latter is a simpler, cheaper and lower-risk procedure, so it is still considered as an option for selected patients. However, there is little evidence comparing both interventions.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified three systematic reviews including six studies overall, of which three were randomized trials. We concluded the anatomic result might be better with scleral buckling in terms of retinal reattachment and risk of recurrence, but the risk of ocular adverse events might be lower with pneumatic retinopexy.
Problem
Rhegmatogenous retinal detachment is the most common cause of retinal detachment and is caused by a full-thickness break in the retina, leading to a separation between the neurosensory retina and the retinal pigment epithelium. If left untreated, rhegmatogenous retinal detachments can progress and cause severe visual loss. The treatment is surgical and the main goal is to improve visual outcome, that depends mainly on the macular attachment or detachment and the time of evolution. Three surgical interventions are used for retinal detachment: pneumatic retinopexy, scleral buckling and vitrectomy.
Pneumatic retinopexy is performed by injecting a bubble of gas into the vitreous cavity, which pushes against the retina, allowing to use photocoagulation or cryotherapy for the retinopexy. Scleral buckling consists in using an encircling element, usually made of silicone, to achieve apposition of the neurosensory retina and the retinal pigment epithelium, with the subsequent repair of the break with photocoagulation or cryotherapy.
Our objective is to determine, using existing evidence, if scleral buckling is truly superior to pneumatic retinopexy.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a section of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found three systematic reviews [1],[2],[3], including six primary studies reported in nine references [4],[5],[6],[7],[8],[9],[10],[11],[12], of which three corresponded to randomized trials reported in five references [4],[5],[6],[7],[8] because one of these studies was reported in several publications [4],[5],[6]. This table and the summary in general are based on the randomized trials since the observational studies did not increase the certainty of the existing evidence or provide additional relevant information. |
|
What types of patients were included* |
All trials included participants with phakic and non phakic eyes (aphakic and pseudophakic), with or without macular detachment. All participants were good candidates to pneumatic retinopexy (uncomplicated retinal detachments, with single or multiple retinal tears, less or equal to one clock hour size, located in the superior half of the retina). |
|
What types of interventions were included* |
All trials compared scleral buckling versus pneumatic retinopexy. Also, one of them [2] analized retinopexy options for scleral buckling and other surgical techniques such as vitrectomy. |
|
What types of outcomes |
All trials reported reattachment of the retina with single intervention and the need of a second procedure to achieve it. Other reported outcomes were recurrence of retinal detachment at 6 months of follow-up, visual success, ocular adverse events and occurrence of proliferative vitreoretinopathy. Follow-up was for at least 6 months (6-90 months) in two trials [4],[7], and of 4.3 months in the other trial [8]. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
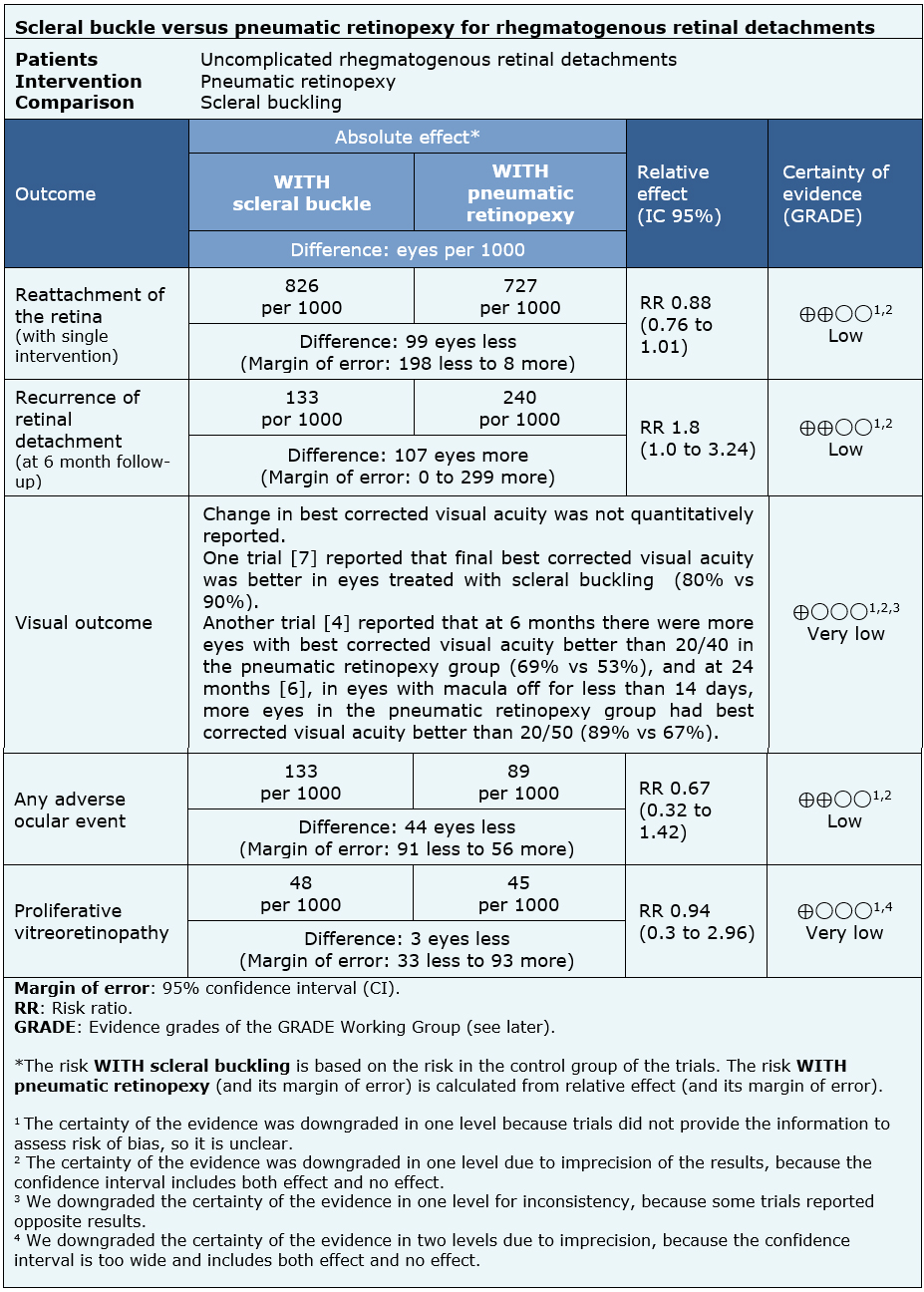
Summary of Findings
The information about scleral buckling versus pneumatic retinopexy is based on three randomized trials [4],[7],[8].
All trials reported reattachment of the retina with single intervention, including 238 eyes. Two trials reported recurrence of retinal detachment at 6 months and visual outcome at 6 months [4],[7] (218 eyes). One trial reported visual success at 24 months [6].
Two trials [4],[7] (218 eyes) reported ocular adverse events (vitreous hemorrhage, subretinal hemorrhage, vitreous or retinal incarceration, hyphema, retinal perforation) and development of proliferative vitreoretinopathy, which is the main cause of surgery failure.
The summary of findings is as follows:
- Scleral buckling might be better than pneumatic retinopexy in achieving reattachment of the retina, but the certainty of the evidence is low.
- Scleral buckling might have a lower risk of recurrence of retinal detachment, but the certainty of the evidence is low.
- It is not clear whether pneumatic retinopexy improves visual success because the certainty of the evidence is very low.
- Pneumatic retinopexy might have less adverse ocular events, but the certainty of the evidence is low.
- It is not clear whether pneumatic retinopexy improves the development of proliferative vitreoretinopathy because the certainty of the evidence is very low.
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
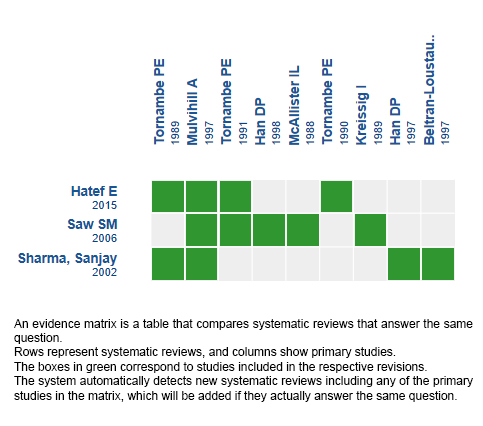
Follow the link to access the interactive version: Scleral buckle versus pneumatic retinopexy for rhegmatogenous retinal detachments
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
El desprendimiento de retina de tipo regmatógeno es aquel causado por un desgarro o ruptura de la retina, y es causa frecuente de pérdida de visión. Dentro del manejo quirúrgico existen varias opciones, entre ellas el implante de silicona o cirugía convencional y la retinopexia neumática. A pesar de que la mayoría de los profesionales prefiere el uso de implante de silicona, la retinopexia neumática es un procedimiento más simple, de menor costo y sigue siendo considerada como alternativa en algunos casos de desprendimiento de retina regmatógeno, sin embargo hay poca evidencia que compare ambas intervenciones.
MÉTODOS
Para responder esta pregunta utilizamos Epistemonikos, la mayor base de datos de revisiones sistemáticas en salud, la cual es mantenida mediante búsquedas en múltiples fuentes de información, incluyendo MEDLINE, EMBASE, Cochrane, entre otras. Extrajimos los datos desde las revisiones identificadas, reanalizamos los datos de los estudios primarios, realizamos un metanálisis y preparamos una tabla de resumen de los resultados utilizando el método GRADE.
RESULTADOS Y CONCLUSIONES
Identificamos tres revisiones sistemáticas que en conjunto incluyeron seis estudios primarios, de los cuales tres corresponden a ensayos aleatorizados. Concluimos que el resultado anatómico podría ser mejor con el uso de implante de silicona en términos de re-aplicación de la retina y del riesgo de recurrencia del desprendimiento, pero la retinopexia neumática podría disminuir la incidencia de efectos adversos quirúrgicos oculares.
 Authors:
María-Teresa Martínez-Mujica[1,2], José Retamal[1,2], Raúl González[2,3]
Authors:
María-Teresa Martínez-Mujica[1,2], José Retamal[1,2], Raúl González[2,3]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Departamento de Oftalmología, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Departamento de Oftalmología, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
E-mail: raulgonzalezc@gmail.com
Author address:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Diagonal Paraguay 476 Santiago Chile

Citation: Martínez-Mujica MT, Retamal J, González R. Scleral buckle versus pneumatic retinopexy for rhegmatogenous retinal detachments. Medwave 2018;18(6):e7277 doi: 10.5867/medwave.2018.06.7277
Submission date: 27/8/2018
Acceptance date: 8/9/2018
Publication date: 5/10/2018
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Epistemonikos Evidence Synthesis Project.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Elham Hatef, Dayse F Sena, Katherine A Fallano, Jonathan Crews4, Diana V Do. Pneumatic retinopexy versus scleral buckle for repairing simple rhegmatogenous retinal detachments [Pneumatic retinopexy versus scleral buckle for repairing simple rhegmatogenous retinal detachments]. Cochrane Database of Systematic Reviews 2015;(5):Art. No.: CD008350.
- Seang-Mei Saw, Gus Gazzard, Ajeet M. Wagle, Jimmy Lim, Kah-Guan Au Eong. An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment. [An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment.]. Acta ophthalmologica Scandinavica October 2006;84(5):606-612.
- Sanjay Sharma. Meta-Analysis of Clinical Trials Comparing Scleral Bucking Surgery to Pneumatic Retinopexy [Meta-Analysis of Clinical Trials Comparing Scleral Bucking Surgery to Pneumatic Retinopexy]. Evidence-Based Ophthalmology July 2002;3(3)((3)):125-128.
- Tornambe PE, Hilton GF for the Retinal Detachment Study Group. Pneumatic retinopexy: a multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1989;96:772–783.
- Tornambe PE, Hilton GF, Grizzard WS, Hammer ME, Poliner LS, Yarian DL, et al. Pneumatic retinopexy: a two- year randomized controlled follow-up study comparing pneumatic retinopexy with scleral buckling. American Academy of Ophthalmology. 1990:123.
- Tornambe PE, Hilton GF, Brinton DA, Flood TP, Green S, Grizzard WS, Hammer ME, Leff SR, Masciulli L, Morgan CM. Pneumatic retinopexy. A two-year follow-up study of the multicentre clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1991; 98: 1115– 1123.
- Mulvihill A, Fulcher T, Datta V, Acheson R. Pneumatic retinopexy versus scleral buckling: a randomized controlled trial. Ir J Med Sci 1996;165(4): 274–277.
- Beltran-Loustaunau MA, Troconis D, Morales- Canton V, et al. Comparative study of vitrectomy, pneumatic retinopexy and scleral buckling for primary rhegmatogenous retinal detachment. Association of Research in Vision and Ophthalmology 1997;38: S673.
- Han DP, Mohsin N, Guse CE, Hartz AJ, Tarkanian C, Wolf MD, et al. and the Southeastern Wisconsin Pneumatic Retinopexy Group. Comparison of pneumatic retinopexy versus scleral buckling in the management of primary retinal detachment. Association of Research in Vision and Ophthalmology Abstracts 1997;38:S483.
- Han DP, Mohsin NC, Guse CE, Hartz A, Tarkanian CN. Southern Wisconsin Pneumatic Retinopexy Study Group. Comparison of pneumatic retinopexy and scleral buckling in the management of primary rhegmatogenous retinal detachment. American Journal of Ophthalmology 1998 126: 658–668.
- McAllister IL, Meyers SM, Zegarra H, Gut- man FA, Zakov ZN, Beck GJ. Comparison of pneumatic retinopexy with alternative surgical techniques. Ophthalmology 1988; 95: 877–883.
- Kreissig I, Failer J, Lincoff H, Ferrari F. Results of a temporary balloon buckle in the treatment of 500 retinal detachments and a comparison with pneumatic retinopexy. American Journal of Ophthalmology 1989; 107: 381–389.
- BMJ Best Practice. Retinal detachment. Last updated Aug 2017. | Link |
 Elham Hatef, Dayse F Sena, Katherine A Fallano, Jonathan Crews4, Diana V Do. Pneumatic retinopexy versus scleral buckle for repairing simple rhegmatogenous retinal detachments [Pneumatic retinopexy versus scleral buckle for repairing simple rhegmatogenous retinal detachments]. Cochrane Database of Systematic Reviews 2015;(5):Art. No.: CD008350.
Elham Hatef, Dayse F Sena, Katherine A Fallano, Jonathan Crews4, Diana V Do. Pneumatic retinopexy versus scleral buckle for repairing simple rhegmatogenous retinal detachments [Pneumatic retinopexy versus scleral buckle for repairing simple rhegmatogenous retinal detachments]. Cochrane Database of Systematic Reviews 2015;(5):Art. No.: CD008350.  Seang-Mei Saw, Gus Gazzard, Ajeet M. Wagle, Jimmy Lim, Kah-Guan Au Eong. An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment. [An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment.]. Acta ophthalmologica Scandinavica October 2006;84(5):606-612.
Seang-Mei Saw, Gus Gazzard, Ajeet M. Wagle, Jimmy Lim, Kah-Guan Au Eong. An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment. [An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment.]. Acta ophthalmologica Scandinavica October 2006;84(5):606-612.  Sanjay Sharma. Meta-Analysis of Clinical Trials Comparing Scleral Bucking Surgery to Pneumatic Retinopexy [Meta-Analysis of Clinical Trials Comparing Scleral Bucking Surgery to Pneumatic Retinopexy]. Evidence-Based Ophthalmology July 2002;3(3)((3)):125-128.
Sanjay Sharma. Meta-Analysis of Clinical Trials Comparing Scleral Bucking Surgery to Pneumatic Retinopexy [Meta-Analysis of Clinical Trials Comparing Scleral Bucking Surgery to Pneumatic Retinopexy]. Evidence-Based Ophthalmology July 2002;3(3)((3)):125-128.  Tornambe PE, Hilton GF for the Retinal Detachment Study Group. Pneumatic retinopexy: a multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1989;96:772–783.
Tornambe PE, Hilton GF for the Retinal Detachment Study Group. Pneumatic retinopexy: a multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1989;96:772–783.  Tornambe PE, Hilton GF, Grizzard WS, Hammer ME, Poliner LS, Yarian DL, et al. Pneumatic retinopexy: a two- year randomized controlled follow-up study comparing pneumatic retinopexy with scleral buckling. American Academy of Ophthalmology. 1990:123.
Tornambe PE, Hilton GF, Grizzard WS, Hammer ME, Poliner LS, Yarian DL, et al. Pneumatic retinopexy: a two- year randomized controlled follow-up study comparing pneumatic retinopexy with scleral buckling. American Academy of Ophthalmology. 1990:123.  Tornambe PE, Hilton GF, Brinton DA, Flood TP, Green S, Grizzard WS, Hammer ME, Leff SR, Masciulli L, Morgan CM. Pneumatic retinopexy. A two-year follow-up study of the multicentre clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1991; 98: 1115– 1123.
Tornambe PE, Hilton GF, Brinton DA, Flood TP, Green S, Grizzard WS, Hammer ME, Leff SR, Masciulli L, Morgan CM. Pneumatic retinopexy. A two-year follow-up study of the multicentre clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1991; 98: 1115– 1123.  Mulvihill A, Fulcher T, Datta V, Acheson R. Pneumatic retinopexy versus scleral buckling: a randomized controlled trial. Ir J Med Sci 1996;165(4): 274–277.
Mulvihill A, Fulcher T, Datta V, Acheson R. Pneumatic retinopexy versus scleral buckling: a randomized controlled trial. Ir J Med Sci 1996;165(4): 274–277.  Beltran-Loustaunau MA, Troconis D, Morales- Canton V, et al. Comparative study of vitrectomy, pneumatic retinopexy and scleral buckling for primary rhegmatogenous retinal detachment. Association of Research in Vision and Ophthalmology 1997;38: S673.
Beltran-Loustaunau MA, Troconis D, Morales- Canton V, et al. Comparative study of vitrectomy, pneumatic retinopexy and scleral buckling for primary rhegmatogenous retinal detachment. Association of Research in Vision and Ophthalmology 1997;38: S673.  Han DP, Mohsin N, Guse CE, Hartz AJ, Tarkanian C, Wolf MD, et al. and the Southeastern Wisconsin Pneumatic Retinopexy Group. Comparison of pneumatic retinopexy versus scleral buckling in the management of primary retinal detachment. Association of Research in Vision and Ophthalmology Abstracts 1997;38:S483.
Han DP, Mohsin N, Guse CE, Hartz AJ, Tarkanian C, Wolf MD, et al. and the Southeastern Wisconsin Pneumatic Retinopexy Group. Comparison of pneumatic retinopexy versus scleral buckling in the management of primary retinal detachment. Association of Research in Vision and Ophthalmology Abstracts 1997;38:S483.  Han DP, Mohsin NC, Guse CE, Hartz A, Tarkanian CN. Southern Wisconsin Pneumatic Retinopexy Study Group. Comparison of pneumatic retinopexy and scleral buckling in the management of primary rhegmatogenous retinal detachment. American Journal of Ophthalmology 1998 126: 658–668.
Han DP, Mohsin NC, Guse CE, Hartz A, Tarkanian CN. Southern Wisconsin Pneumatic Retinopexy Study Group. Comparison of pneumatic retinopexy and scleral buckling in the management of primary rhegmatogenous retinal detachment. American Journal of Ophthalmology 1998 126: 658–668.  McAllister IL, Meyers SM, Zegarra H, Gut- man FA, Zakov ZN, Beck GJ. Comparison of pneumatic retinopexy with alternative surgical techniques. Ophthalmology 1988; 95: 877–883.
McAllister IL, Meyers SM, Zegarra H, Gut- man FA, Zakov ZN, Beck GJ. Comparison of pneumatic retinopexy with alternative surgical techniques. Ophthalmology 1988; 95: 877–883.  Kreissig I, Failer J, Lincoff H, Ferrari F. Results of a temporary balloon buckle in the treatment of 500 retinal detachments and a comparison with pneumatic retinopexy. American Journal of Ophthalmology 1989; 107: 381–389.
Kreissig I, Failer J, Lincoff H, Ferrari F. Results of a temporary balloon buckle in the treatment of 500 retinal detachments and a comparison with pneumatic retinopexy. American Journal of Ophthalmology 1989; 107: 381–389. Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








