Abstract
INTRODUCTION
Urinary tract infection is the most common bacterial infection and recurrences are common. Probiotics have been proposed as an alternative to decrease this risk. However, it is not clear if they are really effective.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified six systematic reviews including nine studies overall, of which seven were randomized trials. We concluded it is not clear whether probiotics decrease the risk of symptomatic urinary tract infection, because the certainty of the evidence is very low.
Problem
Urinary tract infection is the most frequent bacterial infection. It is associated to important morbidity, such as pyelonephritis, sepsis, abscess and renal failure. It is estimated that 40% of the adult population has presented at least 1 episode of urinary infection, of which 80 % are women. Approximately 20-30% of women with a first episode will experience a recurrence.
Probiotics have been proposed among the alternatives for prophylaxis. They would decrease the risk of urinary tract infection by creating a barrier against infectious pathogens, thus reducing the adherence, growing and colonization of such agents. However, the real efficacy of this intervention is not yet clear.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found six systematic reviews [1],[2],[3],[4],[5],[6] that included nine primary studies [7],[8],[9],[10],[11],[12],[13],[14],[15], seven of which correspond to randomized controlled trials [7],[8],[9],[10],[11],[12],[13]. This table and the summary in general are based on the latter. |
|
What types of patients were included* |
All of the trials included women only. Two trials included patients with recurrent urinary tract infection [9],[11], four with an acute episode or with an episode of urinary tract infection within last year [7],[10],[12],[13] and one included healthy participants [8]. One trial included patients under 18 years [13] and the rest only included adults [7],[8],[9],[10],[11],[12]. Five trials excluded patients with use of prophylactic antibiotics [7],[9],[11],[12],[13], five excluded patients with concomitant disease [7],[9],[10],[11],[13] and three excluded pregnant women [7],[9],[11]. |
|
What types of interventions were included* |
All of the trials used probiotics as intervention. Three trials used oral probiotics; Lactobacillus GG drink 4 x 108 CFU/100 ml 5 days a week for a year [12]; Lactobacillus GG drink 4 x 107 CFU/100 xml 5 times per month for 6 months [13]; Lactobacillus casei var rhamnosus GR-1 y Lactobacillus fermentum RC-14 1 x 109 CFU/100 ml 1 per day for 60 days [8]. The other four trials used probiotics in vaginal suppositories: Lactobacillus casei var rhamnosus GR-1 7.5 x 108 CFU by suppository twice a week for 26 weeks [9]; antibiotic treatment for 3 days with norfloxacin or cotrimoxazol, then lactobacillus casei var rhamnosus GR-1 plus Lactobacillus fermentum B-54 1.6 x 109 CFU by suppository twice a week during 2 weeks and at the end of the next 2 months [7]; Lactin-V 1 x 108 CFU by suppository 1 per day for 5 days [10]; Lactobacillus crispatus CTV-5 5x108 CFU once a day for 5 days [11]. |
|
What types of outcomes |
The outcomes, as they were grouped by the systematic reviews, were the following: symptomatic urinary tract infection episodes, total adverse effects, intervention withdrawal because of adverse effects and serious adverse effects. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of findings
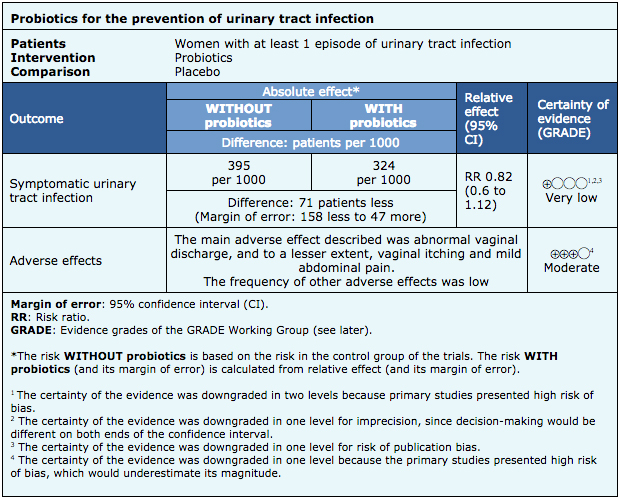
The information about the effects of probiotics is based on six randomized trials [7],[9],[10],[11],[12],[13], that included 352 patients overall. The remaining trial did not report any of the outcomes of interest [8].
All of the trials reported episodes of symptomatic urinary tract infection, three reported total adverse effects [9],[10],[11] and one reported withdrawal due to adverse effects and serious adverse effects [10].
The summary of findings is the following:
- It is not clear whether probiotics decrease the risk of symptomatic urinary tract infection, because the certainty of the evidence is very low.
- Adverse effects of probiotics (abnormal vaginal discharge) are probably rare. The certainty of the evidence is moderate.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
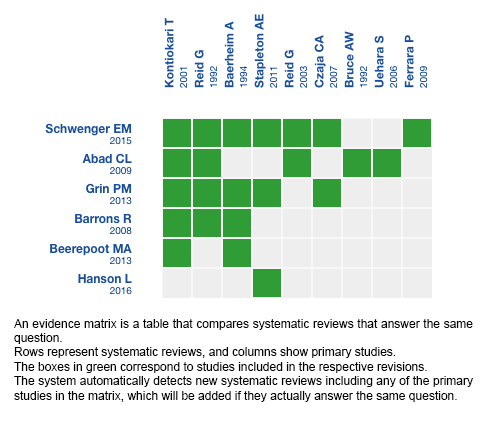
Follow the link to access the interactive version: Probiotics against placebo or no treatment for the prevention of urinary tract infection
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
La infección del tracto urinario es la infección bacteriana más común y su recurrencia es frecuente. Entre las variadas medidas que potencialmente disminuirían este riesgo se ha planteado el uso de probióticos. Sin embargo, no está claro si realmente son efectivos.
MÉTODOS
Para responder esta pregunta utilizamos Epistemonikos, la mayor base de datos de revisiones sistemáticas en salud a nivel mundial, la cual es mantenida mediante búsquedas en múltiples fuentes de información, incluyendo MEDLINE, EMBASE, Cochrane, entre otras. Extrajimos los datos desde las revisiones identificadas, reanalizamos los datos de los estudios primarios, realizamos un metanálisis y preparamos una tabla de resumen de los resultados utilizando el método GRADE.
RESULTADOS Y CONCLUSIONES
Identificamos seis revisiones sistemáticas que en conjunto incluyeron nueve estudios, entre ellos siete ensayos aleatorizados. Concluimos que no está claro si los probióticos disminuyen el riesgo de infección urinaria sintomática, porque la certeza de la evidencia es muy baja.
 Authors:
Juan Canales[1,2], Gabriel Rada[2,3,4,5,6]
Authors:
Juan Canales[1,2], Gabriel Rada[2,3,4,5,6]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Centro Evidencia UC, Pontificia Universidad Católica de Chile, Santiago, Chile
[5] GRADE working group
[6] The Cochrane Collaboration
E-mail: radagabriel@gmail.com
Author address:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Centro de Innovación UC Anacleto Angelini Avda.Vicuña Mackenna 4860 Macul Santiago Chile

Citation: Canales J, Rada G. Are probiotics effective in preventing urinary tract infection?. Medwave 2018 Mar-Abr;18(2):e7185 doi: 10.5867/medwave.2018.02.7185
Submission date: 31/8/2017
Acceptance date: 25/11/2017
Publication date: 4/4/2018
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Epistemonikos Evidence Synthesis Project.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Schwenger EM, Tejani AM, Loewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev. 2015 Dec 23;(12):CD008772. | CrossRef | PubMed |
- Beerepoot MA, Geerlings SE, van Haarst EP, van Charante NM, ter Riet G. Nonantibiotic prophylaxis for recurrent urinary tract infections: a systematic review and meta-analysis of randomized controlled trials. J Urol. 2013 Dec;190(6):1981-9. | CrossRef | PubMed |
- Abad CL, Safdar N. The role of lactobacillus probiotics in the treatment or prevention of urogenital infections--a systematic review. J Chemother. 2009 Jun;21(3):243-52. Review. | PubMed |
- Barrons R, Tassone D. Use of Lactobacillus probiotics for bacterial genitourinary infections in women: a review. Clin Ther. 2008 Mar;30(3):453-68. | CrossRef | PubMed |
- Grin PM, Kowalewska PM, Alhazzan W, Fox-Robichaud AE. Lactobacillus for preventing recurrent urinary tract infections in women: meta-analysis. Can J Urol. 2013 Feb;20(1):6607-14. Review. | PubMed |
- Hanson L, VandeVusse L, Jermé M, Abad CL, Safdar N. Probiotics for Treatment and Prevention of Urogenital Infections in Women: A Systematic Review. J Midwifery Womens Health. 2016 May;61(3):339-55. | CrossRef | PubMed |
- Reid G, Bruce AW, Taylor M. Influence of three-day antimicrobial therapy and lactobacillus vaginal suppositories on recurrence of urinary tract infections. Clin Ther. 1992 Jan-Feb;14(1):11-6. | PubMed |
- Reid G, Charbonneau D, Erb J, Kochanowski B, Beuerman D, Poehner R, Bruce AW. Oral use of Lactobacillus rhamnosus GR-1 and L. fermentum RC-14 significantly alters vaginal flora: randomized, placebo-controlled trial in 64 healthy women. FEMS Immunol Med Microbiol. 2003 Mar 20;35(2):131-4. | PubMed |
- Baerheim A, Larsen E, Digranes A. Vaginal application of lactobacilli in the prophylaxis of recurrent lower urinary tract infection in women. Scand J Prim Health Care. 1994 Dec;12(4):239-43. | PubMed |
- Stapleton AE, Au-Yeung M, Hooton TM, Fredricks DN, Roberts PL, Czaja CA, Yarova-Yarovaya Y, Fiedler T, Cox M, Stamm WE. Randomized, placebo-controlled phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin Infect Dis. 2011 May;52(10):1212-7. | CrossRef | PubMed | PMC |
- Czaja CA, Stapleton AE, Yarova-Yarovaya Y, Stamm WE. Phase I trial of a Lactobacillus crispatus vaginal suppository for prevention of recurrent urinary tract infection in women. Infect Dis Obstet Gynecol. 2007;2007:35387. | CrossRef | PubMed | PMC |
- Kontiokari T, Sundqvist K, Nuutinen M, Pokka T, Koskela M, Uhari M. Randomised trial of cranberry-lingonberry juice and Lactobacillus GG drink for the prevention of urinary tract infections in women. BMJ. 2001 Jun 30;322(7302):1571. | PubMed | PMC |
- Ferrara P, Romaniello L, Vitelli O, Gatto A, Serva M, Cataldi L. Cranberry juice for the prevention of recurrent urinary tract infections: a randomized controlled trial in children. Scand J Urol Nephrol. 2009;43(5):369-72. | CrossRef | PubMed |
- National Collaborating Centre for Chronic Conditions (UK). Urinary tract infections in adults. London: Royal College of Physicians (UK); 2015.
- Talebitaher, Studying the effect of probiotics in the prevention of urinary tract infection among elderlies, IRCT2016111530906N1. | Link |
- Yefet, The Efficacy of Orally Administrated Probiotic Formula in Preventing a Recurrence of a Urinary Tract Infection During Pregnancy, NCT02637986. | Link |
- Fochesato, Can Probiotics be Used in the Prevention of Recurrent UTI in Paediatric Neurogenic Bladder, NCT02044965. | Link |
- Mahmoudi, The Effect of Probiotic Yogurt in Prevention of Urinary Tract Infection, IRCT2013042813154N1. | Link |
- Bonne, A multicentre randomised double-blind, double-dummy placebo-controlled study to assess the efficacy, safety and cost utility of Probiotic prophylaxis of spinal cord injury Urinary Tract Infection. A Therapeutic Trial. (ProSCIUTTU), ACTRN12610000512022. | Link |
- Roth, Probiotics for Girls With Recurring Urinary Tract Infections, NCT00789464. | Link |
- Ducan L, van der Werf-Kok E, Huntley A, Hay A, A systematic review of the evidence for the use of probiotics in preventing recurrent urinary tract infections in women: establishing the optimal probiotic agent(s), dose, route and duration. PROSPERO 2017:CRD42017056374 | Link |
 Schwenger EM, Tejani AM, Loewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev. 2015 Dec 23;(12):CD008772. | CrossRef | PubMed |
Schwenger EM, Tejani AM, Loewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev. 2015 Dec 23;(12):CD008772. | CrossRef | PubMed | Beerepoot MA, Geerlings SE, van Haarst EP, van Charante NM, ter Riet G. Nonantibiotic prophylaxis for recurrent urinary tract infections: a systematic review and meta-analysis of randomized controlled trials. J Urol. 2013 Dec;190(6):1981-9. | CrossRef | PubMed |
Beerepoot MA, Geerlings SE, van Haarst EP, van Charante NM, ter Riet G. Nonantibiotic prophylaxis for recurrent urinary tract infections: a systematic review and meta-analysis of randomized controlled trials. J Urol. 2013 Dec;190(6):1981-9. | CrossRef | PubMed | Abad CL, Safdar N. The role of lactobacillus probiotics in the treatment or prevention of urogenital infections--a systematic review. J Chemother. 2009 Jun;21(3):243-52. Review. | PubMed |
Abad CL, Safdar N. The role of lactobacillus probiotics in the treatment or prevention of urogenital infections--a systematic review. J Chemother. 2009 Jun;21(3):243-52. Review. | PubMed | Barrons R, Tassone D. Use of Lactobacillus probiotics for bacterial genitourinary infections in women: a review. Clin Ther. 2008 Mar;30(3):453-68. | CrossRef | PubMed |
Barrons R, Tassone D. Use of Lactobacillus probiotics for bacterial genitourinary infections in women: a review. Clin Ther. 2008 Mar;30(3):453-68. | CrossRef | PubMed | Grin PM, Kowalewska PM, Alhazzan W, Fox-Robichaud AE. Lactobacillus for preventing recurrent urinary tract infections in women: meta-analysis. Can J Urol. 2013 Feb;20(1):6607-14. Review. | PubMed |
Grin PM, Kowalewska PM, Alhazzan W, Fox-Robichaud AE. Lactobacillus for preventing recurrent urinary tract infections in women: meta-analysis. Can J Urol. 2013 Feb;20(1):6607-14. Review. | PubMed | Hanson L, VandeVusse L, Jermé M, Abad CL, Safdar N. Probiotics for Treatment and Prevention of Urogenital Infections in Women: A Systematic Review. J Midwifery Womens Health. 2016 May;61(3):339-55. | CrossRef | PubMed |
Hanson L, VandeVusse L, Jermé M, Abad CL, Safdar N. Probiotics for Treatment and Prevention of Urogenital Infections in Women: A Systematic Review. J Midwifery Womens Health. 2016 May;61(3):339-55. | CrossRef | PubMed | Reid G, Bruce AW, Taylor M. Influence of three-day antimicrobial therapy and lactobacillus vaginal suppositories on recurrence of urinary tract infections. Clin Ther. 1992 Jan-Feb;14(1):11-6. | PubMed |
Reid G, Bruce AW, Taylor M. Influence of three-day antimicrobial therapy and lactobacillus vaginal suppositories on recurrence of urinary tract infections. Clin Ther. 1992 Jan-Feb;14(1):11-6. | PubMed | Reid G, Charbonneau D, Erb J, Kochanowski B, Beuerman D, Poehner R, Bruce AW. Oral use of Lactobacillus rhamnosus GR-1 and L. fermentum RC-14 significantly alters vaginal flora: randomized, placebo-controlled trial in 64 healthy women. FEMS Immunol Med Microbiol. 2003 Mar 20;35(2):131-4. | PubMed |
Reid G, Charbonneau D, Erb J, Kochanowski B, Beuerman D, Poehner R, Bruce AW. Oral use of Lactobacillus rhamnosus GR-1 and L. fermentum RC-14 significantly alters vaginal flora: randomized, placebo-controlled trial in 64 healthy women. FEMS Immunol Med Microbiol. 2003 Mar 20;35(2):131-4. | PubMed | Baerheim A, Larsen E, Digranes A. Vaginal application of lactobacilli in the prophylaxis of recurrent lower urinary tract infection in women. Scand J Prim Health Care. 1994 Dec;12(4):239-43. | PubMed |
Baerheim A, Larsen E, Digranes A. Vaginal application of lactobacilli in the prophylaxis of recurrent lower urinary tract infection in women. Scand J Prim Health Care. 1994 Dec;12(4):239-43. | PubMed | Stapleton AE, Au-Yeung M, Hooton TM, Fredricks DN, Roberts PL, Czaja CA, Yarova-Yarovaya Y, Fiedler T, Cox M, Stamm WE. Randomized, placebo-controlled phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin Infect Dis. 2011 May;52(10):1212-7. | CrossRef | PubMed | PMC |
Stapleton AE, Au-Yeung M, Hooton TM, Fredricks DN, Roberts PL, Czaja CA, Yarova-Yarovaya Y, Fiedler T, Cox M, Stamm WE. Randomized, placebo-controlled phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin Infect Dis. 2011 May;52(10):1212-7. | CrossRef | PubMed | PMC | Czaja CA, Stapleton AE, Yarova-Yarovaya Y, Stamm WE. Phase I trial of a Lactobacillus crispatus vaginal suppository for prevention of recurrent urinary tract infection in women. Infect Dis Obstet Gynecol. 2007;2007:35387. | CrossRef | PubMed | PMC |
Czaja CA, Stapleton AE, Yarova-Yarovaya Y, Stamm WE. Phase I trial of a Lactobacillus crispatus vaginal suppository for prevention of recurrent urinary tract infection in women. Infect Dis Obstet Gynecol. 2007;2007:35387. | CrossRef | PubMed | PMC | Kontiokari T, Sundqvist K, Nuutinen M, Pokka T, Koskela M, Uhari M. Randomised trial of cranberry-lingonberry juice and Lactobacillus GG drink for the prevention of urinary tract infections in women. BMJ. 2001 Jun 30;322(7302):1571. | PubMed | PMC |
Kontiokari T, Sundqvist K, Nuutinen M, Pokka T, Koskela M, Uhari M. Randomised trial of cranberry-lingonberry juice and Lactobacillus GG drink for the prevention of urinary tract infections in women. BMJ. 2001 Jun 30;322(7302):1571. | PubMed | PMC | Ferrara P, Romaniello L, Vitelli O, Gatto A, Serva M, Cataldi L. Cranberry juice for the prevention of recurrent urinary tract infections: a randomized controlled trial in children. Scand J Urol Nephrol. 2009;43(5):369-72. | CrossRef | PubMed |
Ferrara P, Romaniello L, Vitelli O, Gatto A, Serva M, Cataldi L. Cranberry juice for the prevention of recurrent urinary tract infections: a randomized controlled trial in children. Scand J Urol Nephrol. 2009;43(5):369-72. | CrossRef | PubMed | National Collaborating Centre for Chronic Conditions (UK). Urinary tract infections in adults. London: Royal College of Physicians (UK); 2015.
National Collaborating Centre for Chronic Conditions (UK). Urinary tract infections in adults. London: Royal College of Physicians (UK); 2015.  Talebitaher, Studying the effect of probiotics in the prevention of urinary tract infection among elderlies, IRCT2016111530906N1. | Link |
Talebitaher, Studying the effect of probiotics in the prevention of urinary tract infection among elderlies, IRCT2016111530906N1. | Link | Yefet, The Efficacy of Orally Administrated Probiotic Formula in Preventing a Recurrence of a Urinary Tract Infection During Pregnancy, NCT02637986. | Link |
Yefet, The Efficacy of Orally Administrated Probiotic Formula in Preventing a Recurrence of a Urinary Tract Infection During Pregnancy, NCT02637986. | Link | Fochesato, Can Probiotics be Used in the Prevention of Recurrent UTI in Paediatric Neurogenic Bladder, NCT02044965. | Link |
Fochesato, Can Probiotics be Used in the Prevention of Recurrent UTI in Paediatric Neurogenic Bladder, NCT02044965. | Link | Mahmoudi, The Effect of Probiotic Yogurt in Prevention of Urinary Tract Infection, IRCT2013042813154N1. | Link |
Mahmoudi, The Effect of Probiotic Yogurt in Prevention of Urinary Tract Infection, IRCT2013042813154N1. | Link | Bonne, A multicentre randomised double-blind, double-dummy placebo-controlled study to assess the efficacy, safety and cost utility of Probiotic prophylaxis of spinal cord injury Urinary Tract Infection. A Therapeutic Trial. (ProSCIUTTU), ACTRN12610000512022. | Link |
Bonne, A multicentre randomised double-blind, double-dummy placebo-controlled study to assess the efficacy, safety and cost utility of Probiotic prophylaxis of spinal cord injury Urinary Tract Infection. A Therapeutic Trial. (ProSCIUTTU), ACTRN12610000512022. | Link | Ducan L, van der Werf-Kok E, Huntley A, Hay A, A systematic review of the evidence for the use of probiotics in preventing recurrent urinary tract infections in women: establishing the optimal probiotic agent(s), dose, route and duration. PROSPERO 2017:CRD42017056374 | Link |
Ducan L, van der Werf-Kok E, Huntley A, Hay A, A systematic review of the evidence for the use of probiotics in preventing recurrent urinary tract infections in women: establishing the optimal probiotic agent(s), dose, route and duration. PROSPERO 2017:CRD42017056374 | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








