Abstract
INTRODUCTION
Urinary tract infection commonly affects postmenopausal women, probably because of the changes in vaginal flora secondary to estrogen deficiency. So, the use of vaginal estrogens could revert this process and then decrease the risk of infection. However, it is not clear whether they are really effective.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified seven systematic reviews including four primary studies overall and all were randomized trials. We concluded it is not clear whether vaginal estrogens decrease the risk of symptomatic urinary infection because the certainty of the available evidence is very low.
Problem
Recurrent urinary tract infection is a common condition in women. The risk is higher in postmenopausal women, possibly due to changes in the vaginal flora because of the decreasing of local and systemic estrogens during menopause.
The use of vaginal estrogens has been suggested as a therapeutic strategy. The proposed mechanism is the reduction in vaginal pH, stimulating proliferation of lactobacilli, and avoiding the growth of gram negative uropathogenic bacteria. However, the real impact of this measure is not clear.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found seven systematic reviews [1],[2],[3],[4],[5],[6],[7] which include four randomized controlled trials overall [8],[9],[10],[11]. This table and the summary in general are based on the latter [8],[9],[10],[11] since the inclusion of the observational studies did not increase the certainty of the existing evidence or provide relevant additional information. |
|
What types of patients were included* |
All trials included postmenopausal women with a history of recurrent urinary tract infection. The average age reported in three trials [8],[10],[11], ranged from 58 to 68 years. One trial did not report it [9]. |
|
What types of interventions were included* |
Vaginal estrogens were administered as follows: 2 mg estradiol for 36 months [8]; 25 µg/day estradiol for a week, followed by 25 µg twice a week for five months [9]; 0.5 mg/day estriol for two weeks, followed by 0.5 mg twice a week for eight months [10] and 1 ovule of estriol (1 mg) once a day for two weeks, followed by 2 ovules of estriol once a week for 6 months [11]. |
|
What types of outcomes |
The systematic reviews pooled results of the different trials in the following outcomes: Urinary tract infection at the end of the treatment period, probability of suffering at least one urinary infection, vaginal PH, positive lactobacilli, adverse effects. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
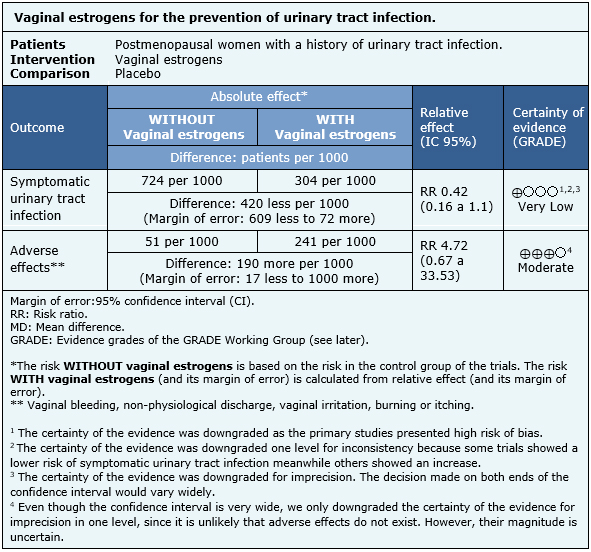
Summary of Findings
The information about the effects of vaginal estrogens for the prevention of urinary tract infection is based on two randomized trials which include 201 patients [8],[10]. It was not possible to reuse data from two trials [9],[11] because they did not report any outcome of interest or none of the identified reviews could extract the data in a way it could be incorporated into a meta-analysis. Both trials reported urinary tract infection at the end of the treatment period and adverse effects (201 patients) [8],[10].
The summary of findings is the following:
- It is not clear whether vaginal estrogens decrease the risk of symptomatic urinary tract infection in postmenopausal women, because certainty of the evidence is very low.
- Adverse effects of vaginal estrogens are probably frequent. The certainty of the evidence is moderate.
Follow the link to access the interactive version of this table (Interactive Summary of Findings- iSoF)

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
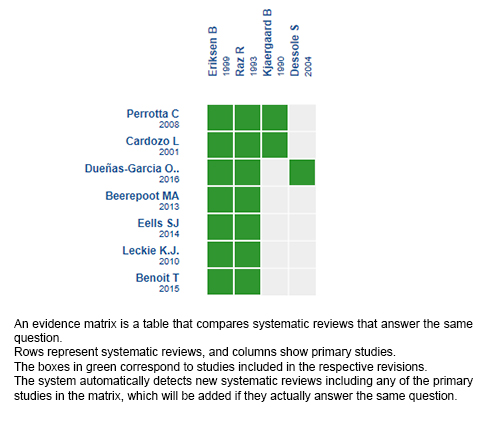
Follow the link to access the interactive version: Estrogens for preventing urinary tract infection in postmenopausal women
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
Urinary tract infection commonly affects postmenopausal women, probably because of the changes in vaginal flora secondary to estrogen deficiency. So, the use of vaginal estrogens could revert this process and then decrease the risk of infection. However, it is not clear whether they are really effective.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified seven systematic reviews including four primary studies overall and all were randomized trials. We concluded it is not clear whether vaginal estrogens decrease the risk of symptomatic urinary infection because the certainty of the available evidence is very low.
 Authors:
Juan Pablo Canales[1,2], Viviana Castro[1,2], Gabriel Rada[2,3,4,5,6]
Authors:
Juan Pablo Canales[1,2], Viviana Castro[1,2], Gabriel Rada[2,3,4,5,6]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Centro Evidencia UC, Pontificia Universidad Católica de Chile, Santiago, Chile
[5] GRADE working group
[6] The Cochrane Collaboration
E-mail: radagabriel@gmail.com
Author address:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Centro de Innovación UC Anacleto Angelini Avda.Vicuña Mackenna 4860 Macul Santiago Chile

Citation: Canales J, Castro V, Rada G. Are vaginal estrogens effective for preventing urinary tract infection in postmenopausal women?. Medwave 2017 Nov-Dic;17(9):e7093 doi: 10.5867/medwave.2017.09.7093
Submission date: 12/9/2017
Acceptance date: 17/11/2017
Publication date: 21/11/2017
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Epistemonikos Evidence Synthesis Project.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev. 2008 Apr 16;(2):CD005131. | CrossRef | PubMed |
- Beerepoot MA, Geerlings SE, van Haarst EP, van Charante NM, ter Riet G. Nonantibiotic prophylaxis for recurrent urinary tract infections: a systematic review and meta-analysis of randomized controlled trials. J Urol. 2013 Dec;190(6):1981-9. | CrossRef | PubMed |
- Eells SJ, Bharadwa K, McKinnell JA, Miller LG. Recurrent urinary tract infections among women: comparative effectiveness of 5 prevention and management strategies using a Markov chain Monte Carlo model. Clin Infect Dis. 2014 Jan;58(2):147-60. | CrossRef | PubMed | PMC |
- Cardozo L, Lose G, McClish D, Versi E, de KoningGans H. A systematic review of estrogens for recurrent urinary tract infections: third report of the hormones and urogenital therapy (HUT) committee. IntUrogynecol J Pelvic Floor Dysfunct. 2001;12(1):15-20. | PubMed |
- Dueñas-Garcia OF, Sullivan G, Hall CD, Flynn MK, OʼDell K. Pharmacological Agents to Decrease New Episodes of Recurrent Lower Urinary Tract Infections in Postmenopausal Women. A Systematic Review. Female Pelvic Med Reconstr Surg. 2016 Mar-Apr;22(2):63-9. | CrossRef | PubMed |
- Leckie KJ. What is the evidence for the role of oestrogen in the prevention of recurrent urinary tract infections in postmenopausal women? An evidence-based review. Journal of Clinical Gerontology and Geriatrics 2010 December 2010;1(2):31-35.
- Benoit T, Leguevaque P, Roumiguié M, Beauval JB, Malavaud B, Soulié M, Rischmann P, Gourdy P, Arnal JF, Game X. [Use of local estrogenotherapy in urology and pelviperineology: A systematic review]. Prog Urol. 2015 Sep;25(11):628-35. French. | CrossRef | PubMed |
- Eriksen B. A randomized, open, parallel-group study on the preventive effect of an estradiol-releasing vaginal ring (Estring) on recurrent urinary tract infections in postmenopausal women. Am J Obstet Gynecol. 1999 May;180(5):1072-9. | PubMed |
- Kjaergaard B, Walter S, Knudsen A, Johansen B, Barlebo H. [Treatment with low-dose vaginal estradiol in post-menopausal women. A double-blind controlled trial]. UgeskrLaeger. 1990 Mar 5;152(10):658-9. Danish. | PubMed |
- Raz R, Stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med. 1993 Sep 9;329(11):753-6. | PubMed |
- Dessole S, Rubattu G, Ambrosini G, Gallo O, Capobianco G, Cherchi PL, Marci R, Cosmi E. Efficacy of low-dose intravaginal estriol on urogenital aging in postmenopausal women. Menopause. 2004 Jan-Feb;11(1):49-56. | PubMed |
- Orlander JD, Jick SS, Dean AD, Jick H. Urinary tract infections and estrogen use in older women. J Am Geriatr Soc. 1992 Aug;40(8):817-20. | PubMed |
- Parsons CL, Schmidt JD. Control of recurrent lower urinary tract infection in the postmenopausal woman. J Urol. 1982 Dec;128(6):1224-6. | PubMed |
- Pinggera GM, Feuchtner G, Frauscher F, Rehder P, Strasser H, Bartsch G, Herwig R. Effects of local estrogen therapy on recurrent urinary tract infections in young females under oral contraceptives. Eur Urol. 2005 Feb;47(2):243-9. | PubMed |
- National Collaborating Centre for Chronic Conditions (UK). Urinary tract infections in adults. 2015. | Link |
- G.Bonkat (Co-chair), R. Pickard (Co-chair), R. Bartoletti, F. Bruyère, S.E. Geerlings, F. Wagenlehner, B. Wullt Guidelines Associates: T. Cai, B. Köves, A. Pilatz, B. Pradere, R. Veeratterapillay. Guidelines on Urological Infections - European Association of Urology. 2016. | Link |
- Kimberly Ferrante. Vaginal Estrogen for the Prevention of Recurrent Urinary Tract Infection in Postmenopausal Women (VESPR), NCT01958073. 2017. | Link |
 Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev. 2008 Apr 16;(2):CD005131.
| CrossRef | PubMed |
Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev. 2008 Apr 16;(2):CD005131.
| CrossRef | PubMed | Beerepoot MA, Geerlings SE, van Haarst EP, van Charante NM, ter Riet G. Nonantibiotic prophylaxis for recurrent urinary tract infections: a systematic review and meta-analysis of randomized controlled trials. J Urol. 2013 Dec;190(6):1981-9. | CrossRef | PubMed |
Beerepoot MA, Geerlings SE, van Haarst EP, van Charante NM, ter Riet G. Nonantibiotic prophylaxis for recurrent urinary tract infections: a systematic review and meta-analysis of randomized controlled trials. J Urol. 2013 Dec;190(6):1981-9. | CrossRef | PubMed | Eells SJ, Bharadwa K, McKinnell JA, Miller LG. Recurrent urinary tract infections among women: comparative effectiveness of 5 prevention and management strategies using a Markov chain Monte Carlo model. Clin Infect Dis. 2014 Jan;58(2):147-60. | CrossRef | PubMed | PMC |
Eells SJ, Bharadwa K, McKinnell JA, Miller LG. Recurrent urinary tract infections among women: comparative effectiveness of 5 prevention and management strategies using a Markov chain Monte Carlo model. Clin Infect Dis. 2014 Jan;58(2):147-60. | CrossRef | PubMed | PMC | Cardozo L, Lose G, McClish D, Versi E, de KoningGans H. A systematic review of estrogens for recurrent urinary tract infections: third report of the hormones and urogenital therapy (HUT) committee. IntUrogynecol J Pelvic Floor Dysfunct. 2001;12(1):15-20. | PubMed |
Cardozo L, Lose G, McClish D, Versi E, de KoningGans H. A systematic review of estrogens for recurrent urinary tract infections: third report of the hormones and urogenital therapy (HUT) committee. IntUrogynecol J Pelvic Floor Dysfunct. 2001;12(1):15-20. | PubMed | Dueñas-Garcia OF, Sullivan G, Hall CD, Flynn MK, OʼDell K. Pharmacological Agents to Decrease New Episodes of Recurrent Lower Urinary Tract Infections in Postmenopausal Women. A Systematic Review. Female Pelvic Med Reconstr Surg. 2016 Mar-Apr;22(2):63-9. | CrossRef | PubMed |
Dueñas-Garcia OF, Sullivan G, Hall CD, Flynn MK, OʼDell K. Pharmacological Agents to Decrease New Episodes of Recurrent Lower Urinary Tract Infections in Postmenopausal Women. A Systematic Review. Female Pelvic Med Reconstr Surg. 2016 Mar-Apr;22(2):63-9. | CrossRef | PubMed | Leckie KJ. What is the evidence for the role of oestrogen in the prevention of recurrent urinary tract infections in postmenopausal women? An evidence-based review. Journal of Clinical Gerontology and Geriatrics 2010 December 2010;1(2):31-35.
Leckie KJ. What is the evidence for the role of oestrogen in the prevention of recurrent urinary tract infections in postmenopausal women? An evidence-based review. Journal of Clinical Gerontology and Geriatrics 2010 December 2010;1(2):31-35.  Benoit T, Leguevaque P, Roumiguié M, Beauval JB, Malavaud B, Soulié M, Rischmann P, Gourdy P, Arnal JF, Game X. [Use of local estrogenotherapy in urology and pelviperineology: A systematic review]. Prog Urol. 2015 Sep;25(11):628-35. French. | CrossRef | PubMed |
Benoit T, Leguevaque P, Roumiguié M, Beauval JB, Malavaud B, Soulié M, Rischmann P, Gourdy P, Arnal JF, Game X. [Use of local estrogenotherapy in urology and pelviperineology: A systematic review]. Prog Urol. 2015 Sep;25(11):628-35. French. | CrossRef | PubMed | Eriksen B. A randomized, open, parallel-group study on the preventive effect of an estradiol-releasing vaginal ring (Estring) on recurrent urinary tract infections in postmenopausal women. Am J Obstet Gynecol. 1999 May;180(5):1072-9. | PubMed |
Eriksen B. A randomized, open, parallel-group study on the preventive effect of an estradiol-releasing vaginal ring (Estring) on recurrent urinary tract infections in postmenopausal women. Am J Obstet Gynecol. 1999 May;180(5):1072-9. | PubMed | Kjaergaard B, Walter S, Knudsen A, Johansen B, Barlebo H. [Treatment with low-dose vaginal estradiol in post-menopausal women. A double-blind controlled trial]. UgeskrLaeger. 1990 Mar 5;152(10):658-9. Danish. | PubMed |
Kjaergaard B, Walter S, Knudsen A, Johansen B, Barlebo H. [Treatment with low-dose vaginal estradiol in post-menopausal women. A double-blind controlled trial]. UgeskrLaeger. 1990 Mar 5;152(10):658-9. Danish. | PubMed | Raz R, Stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med. 1993 Sep 9;329(11):753-6. | PubMed |
Raz R, Stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med. 1993 Sep 9;329(11):753-6. | PubMed | Dessole S, Rubattu G, Ambrosini G, Gallo O, Capobianco G, Cherchi PL, Marci R, Cosmi E. Efficacy of low-dose intravaginal estriol on urogenital aging in postmenopausal women. Menopause. 2004 Jan-Feb;11(1):49-56. | PubMed |
Dessole S, Rubattu G, Ambrosini G, Gallo O, Capobianco G, Cherchi PL, Marci R, Cosmi E. Efficacy of low-dose intravaginal estriol on urogenital aging in postmenopausal women. Menopause. 2004 Jan-Feb;11(1):49-56. | PubMed | Orlander JD, Jick SS, Dean AD, Jick H. Urinary tract infections and estrogen use in older women. J Am Geriatr Soc. 1992 Aug;40(8):817-20. | PubMed |
Orlander JD, Jick SS, Dean AD, Jick H. Urinary tract infections and estrogen use in older women. J Am Geriatr Soc. 1992 Aug;40(8):817-20. | PubMed | Parsons CL, Schmidt JD. Control of recurrent lower urinary tract infection in the postmenopausal woman. J Urol. 1982 Dec;128(6):1224-6. | PubMed |
Parsons CL, Schmidt JD. Control of recurrent lower urinary tract infection in the postmenopausal woman. J Urol. 1982 Dec;128(6):1224-6. | PubMed | Pinggera GM, Feuchtner G, Frauscher F, Rehder P, Strasser H, Bartsch G, Herwig R. Effects of local estrogen therapy on recurrent urinary tract infections in young females under oral contraceptives. Eur Urol. 2005 Feb;47(2):243-9. | PubMed |
Pinggera GM, Feuchtner G, Frauscher F, Rehder P, Strasser H, Bartsch G, Herwig R. Effects of local estrogen therapy on recurrent urinary tract infections in young females under oral contraceptives. Eur Urol. 2005 Feb;47(2):243-9. | PubMed | National Collaborating Centre for Chronic Conditions (UK). Urinary tract infections in adults. 2015. | Link |
National Collaborating Centre for Chronic Conditions (UK). Urinary tract infections in adults. 2015. | Link | G.Bonkat (Co-chair), R. Pickard (Co-chair), R. Bartoletti, F. Bruyère, S.E. Geerlings, F. Wagenlehner, B. Wullt Guidelines Associates: T. Cai, B. Köves, A. Pilatz, B. Pradere, R. Veeratterapillay. Guidelines on Urological Infections - European Association of Urology. 2016. | Link |
G.Bonkat (Co-chair), R. Pickard (Co-chair), R. Bartoletti, F. Bruyère, S.E. Geerlings, F. Wagenlehner, B. Wullt Guidelines Associates: T. Cai, B. Köves, A. Pilatz, B. Pradere, R. Veeratterapillay. Guidelines on Urological Infections - European Association of Urology. 2016. | Link | Kimberly Ferrante. Vaginal Estrogen for the Prevention of Recurrent Urinary Tract Infection in Postmenopausal Women (VESPR), NCT01958073. 2017. | Link |
Kimberly Ferrante. Vaginal Estrogen for the Prevention of Recurrent Urinary Tract Infection in Postmenopausal Women (VESPR), NCT01958073. 2017. | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








