Abstract
Acute bacterial tonsillopharyngitis in children has been classically treated with long courses of antibiotic, usually 10 days, with the intention to prevent the occurrence of complications. However, it has not been clarified whether a shortened treatment could be equally effective in fulfilling that purpose. To answer this question, we searched in Epistemonikos database, which is maintained by screening multiple databases. We identified five systematic reviews including 59 randomized trials overall. We extracted data, conducted a meta-analysis and generated a summary of findings table using the GRADE approach. We concluded that a shortened antibiotic regimen is probably similar, or with minimal differences, to a longer course, and might not make any difference regarding complications related to Streptococcus group A infection.
Problem
Traditionally, bacterial tonsillopharyngitis in children, mainly caused by Streptococcus, has been treated with long antibiotic courses (10 days) with the purpose of eradicating Streptococcus group A and consequently preventing its complications. However, it is unknown whether a shortened treatment can be equally effective to accomplish that same purpose, probably reducing costs, possible adverse effects and improving adherence to treatment.
Methods
We used Epistemonikos database, which is maintained by screening multiple databases, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found five systematic reviews [1],[2],[3],[4],[5] including 59 primary studies, reported in 54 references (some articles report more than one study) [6],[7],[8], [9],[10],[11],[12],[13],[14],[15],[16],[17],[18],[19],[20], [21],[22],[23],[24],[25],[26],[27],[28],[29],[30],[31], [32],[33],[34],[35],[36],[37],[38],[39],[40],[41],[42], [43],[44],[45],[46],[47],[48],[49],[50],[51],[52],[53], [54],[55],[56],[57],[58],[59]. All of the studies correspond to randomized controlled trials. We excluded from the analysis those trials whose long course of antibiotics lasted less than 10 days [33],[58], [59]. We included trials that involved only pediatric patients, whose age was 18 years or less [6],[7],[8],[9],[10],[12], [13],[14],[15],[19],[21],[23],[24],[25],[30],[31],[32], [37],[41],[43],[44],[45],[46],[48],[49],[50],[52],[53], [56],[57], and trials that enrolled adults too, if they were analyzed independently [34]. That is, 36 randomized trials, reported in 31 references. |
|
What types of patients were included |
Patients who participated in the trials included in this review correspond in their entirety to pediatric patients (between six months and 18 years). All trials included only patients with clinically compatible symptoms and microbiological diagnosis of Streptococcus group A (by culture or rapid test). One trial also included Anti-streptolysin O antibodies (ASO) as a possible test for the microbiological certification of Streptococcus group A [34]. |
|
What types of interventions were included |
All included trials compared the use of shortened antibiotic treatment (three to seven days) versus a standard 10-day antibiotic treatment. Only five trials [15],[24],[34],[37],[46] used the same antibiotic as standard and shortened treatment. One of these used cefaclor [15], one cefuroxime [24], one cefetamet [34], one cefpodoxime [37] and one penicillin V [46]. Nineteen trials used a macrolide as a shortened treatment; sixteen compared it to a beta-lactam [13],[14],[19],[23], [30],[31],[41],[43],[44],[48],[49],[50],[52] and three to a macrolide [32],[56],[57]. Sixteen trials used a beta-lactam as a shortened treatment; all were compared to a beta-lactam [6],[7], [8],[10],[12],[15],[21],[24],[25],[34],[37],[45],[46],[52], [53]. One trial compared the use of a macrolide or beta-lactam versus a standard penicillin treatment [9]. One trial allowed the use of analgesics as cointervention [15], two did not allow the use of concomitant analgesics [23],[34], and the rest did not report cointerventions. In all trials, except one [34], an early follow-up was conducted between days 0 to 15 once completed the antibiotic treatment. The majority [6],[7],[9],[10],[12], [13],[19],[21],[23],[25],[30],[31],[37],[41],[43],[44], [45],[52],[53],[56] also report having a late follow-up of variable duration with up to one year of follow-up after treatment. |
|
What types of outcomes |
The identified systematic reviews grouped the outcomes as follows:
|
Summary of findings
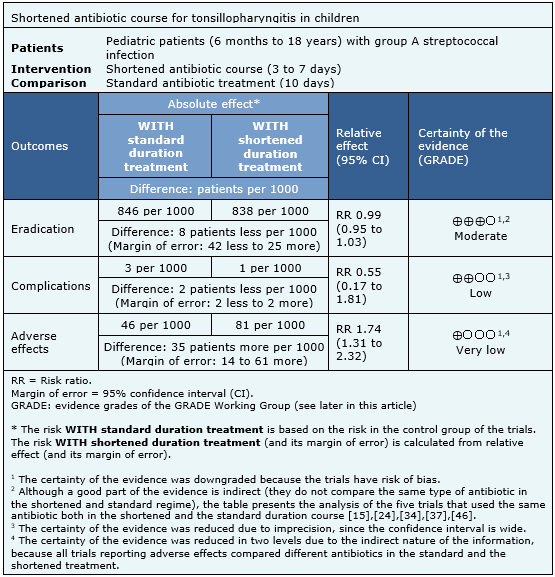
Information on the effects of shortened treatment of bacterial tonsillopharyngitis in children is based on 36 randomized trials. All of the trials (15,869 patients) reported microbiological eradication; three trials (8,135 patients) complications of group A Streptococcus [9],[44],[45] and 21 trials [6],[7],[10],[12],[13],[19],[21],[23],[29],[30],[31],[37],[41],[43],[44],[45],[52],[53] (7,997 patients) measured the adverse effects of therapy. The summary of findings is as follows:
- A shortened antibiotic course probably results in little or no difference in the Streptococcus group A eradication rate for bacterial tonsillopharyngitis in children, compared to a longer course. The certainty of the evidence is moderate.
- A shortened antibiotic course might not make any difference in the complications related to Streptococcus group A infection, compared to a longer course. The certainty of the evidence is low.
- It is unclear whether a shortened antibiotic course reduces adverse effects because the certainty of the evidence is very low.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
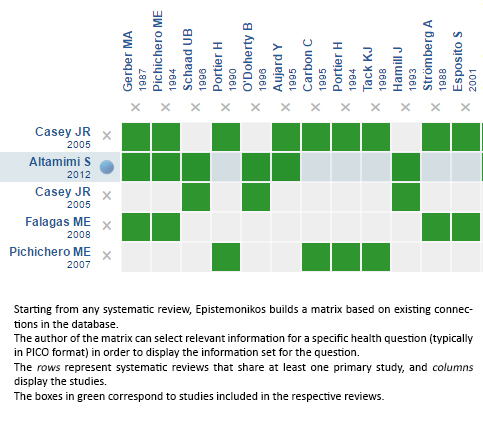
Follow the link to access the interactive version: Short-course antibiotic treatment for tonsillopharyngitis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

La faringoamigdalitis aguda bacteriana en niños ha sido clásicamente tratada con cursos largos de antibiótico, generalmente de 10 días, a modo de prevenir la aparición de complicaciones. Sin embargo, no ha sido esclarecido si un tratamiento acortado pudiese ser igualmente efectivo en cumplir dicho propósito. Utilizando la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en múltiples bases de datos, identificamos cinco revisiones sistemáticas que en conjunto incluyen 59 estudios controlados aleatorizados. Extrajimos los datos, realizamos un metanálisis y preparamos tablas de resumen de los resultados utilizando el método GRADE. Concluimos que un esquema antibiótico acortado es probablemente similar, o con diferencias mínimas, con un esquema más largo en cuanto a la erradicación, y podría no hacer diferencias en cuanto a las complicaciones del estreptococo grupo A.
 Authors:
Camila Rojas-Ramírez[1,2], Tomás Kramer-Urrutia[1,2], Lorena Cifuentes[2,3,4]
Authors:
Camila Rojas-Ramírez[1,2], Tomás Kramer-Urrutia[1,2], Lorena Cifuentes[2,3,4]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Departamento de Pediatría, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Programa de Salud Basada en Evidencia, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
E-mail: lorena.cifuentes@uc.cl
Author address:
[1] Facultad de Medicina Pontificia Universidad Católica de Chile Diagonal Paraguay 362 Santiago Centro Chile.

Citation: Rojas-Ramírez C, Kramer-Urrutia T, Cifuentes L. Is a short-course antibiotic treatment effective for streptococcal tonsillopharyngitis in children?. Medwave2017;17(Suppl1):e6873 doi: 10.5867/medwave.2017.6873
Submission date: 29/12/2016
Acceptance date: 29/12/2016
Publication date: 24/3/2017

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Altamimi S, Khalil A, Khalaiwi KA, Milner RA, Pusic MV, Al Othman MA. Short-term late-generation antibiotics versus longer term penicillin for acute streptococcal pharyngitis in children. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD004872 | CrossRef | PubMed |
- Casey JR, Pichichero ME. Metaanalysis of short course antibiotic treatment for group a streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 2005 Oct;24(10):909-17 | PubMed |
- Casey JR, Pichichero ME. Higher dosages of azithromycin are more effective in treatment of group A streptococcal tonsillopharyngitis. Clin Infect Dis. 2005 Jun 15;40(12):1748-55 | PubMed |
- Falagas ME, Vouloumanou EK, Matthaiou DK, Kapaskelis AM, Karageorgopoulos DE. Effectiveness and safety of short-course vs long-course antibiotic therapy for group a beta hemolytic streptococcal tonsillopharyngitis: a meta-analysis of randomized trials. Mayo Clin Proc. 2008 Aug;83(8):880-9 | PubMed |
- Pichichero ME, Casey JR. Bacterial eradication rates with shortened courses of 2nd- and 3rd-generation cephalosporins versus 10 days of penicillin for treatment of group A streptococcal tonsillopharyngitis in adults. Diagn Microbiol Infect Dis. 2007 Oct;59(2):127-30 | PubMed |
- Adam D, Hostalek U, Tröster K. 5-day cefixime therapy for bacterial pharyngitis and/or tonsillitis: comparison with 10-day penicillin V therapy. Cefixime Study Group. Infection. 1995;23 Suppl 2:S83-6 | PubMed |
- Adam D, Scholz H. Five days of erythromycin estolate versus ten days of penicillin V in the treatment of group A streptococcal tonsillopharyngitis in children. Pharyngitis Study Group. Eur J Clin Microbiol Infect Dis. 1996 Sep;15(9):712-7 | PubMed |
- Adam D, Scholz H, Helmerking M. Comparison of short-course (5 day) cefuroxime axetil with a standard 10 day oral penicillin V regimen in the treatment of tonsillopharyngitis. J Antimicrob Chemother. 2000 Feb;45 Suppl:23-30 | PubMed |
- Adam D, Scholz H, Helmerking M. Short-course antibiotic treatment of 4782 culture-proven cases of group A streptococcal tonsillopharyngitis and incidence of poststreptococcal sequelae. J Infect Dis. 2000 Aug;182(2):509-16 | PubMed |
- Aujard Y, Boucot I, Brahimi N, Chiche D, Bingen E. Comparative efficacy and safety of four-day cefuroxime axetil and ten-day penicillin treatment of group A beta-hemolytic streptococcal pharyngitis in children. Pediatr Infect Dis J. 1995 Apr;14(4):295-300 | PubMed |
- Carbon C, Chatelin A, Bingen E, Zuck P, Rio Y, Guetat F, et al. A double-blind randomized trial comparing the efficacy and safety of a 5-day course of cefotiam hexetil with that of a 10-day course of penicillin V in adult patients with pharyngitis caused by group A beta-haemolytic streptococci. J Antimicrob Chemother. 1995 Jun;35(6):843-54 | PubMed |
- Cohen R, Levy C, Doit C, De La Rocque F, Boucherat M, Fitoussi F, et al. Six-day amoxicillin vs. ten-day penicillin V therapy for group A streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 1996 Aug;15(8):678-82 | PubMed |
- Cohen R, Reinert P, De La Rocque F, Levy C, Boucherat M, Robert M, et al. Comparison of two dosages of azithromycin for three days versus penicillin V for ten days in acute group A streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 2002 Apr;21(4):297-303 | PubMed |
- Cremer J, Wallrauch C, Milatovic D, Braveny I. Azithromycin versus cefaclor in the treatment of pediatric patients with acute group A beta-hemolytic streptococcal tonsillopharyngitis. Eur J Clin Microbiol Infect Dis. 1998 Apr;17(4):235-9 | PubMed |
- Esposito S, Noviello S, Ianniello F, D'Errico G. Short-course therapy with cefaclor for treatment of streptococcal pharyngotonsillitis. Int J Antimicrob Agents. 2001 Oct;18(4):341-5 | PubMed |
- García Callejo FJ, Velert Vila MM, Orts Alborch MH, Pardo Mateu L, Esparcia Navarro M. [Comparison of azithromycin, amoxicillin/clavulanic acid and cefaclor in the treatment of acute ENT infections]. Acta Otorrinolaringol Esp. 1998 May;49(4):306-12 | PubMed |
- Gehanno P, Chiche D. Treatment of group a beta hemolytic streptococcal tonsillitis with cefuroxime axetil for 4 days : a comparative study with penicillin v for 10 days. Médecine et Maladies Infectieuses. 1991;21:66-70 | Link |
- Gerber MA, Randolph MF, Chanatry J, Wright LL, De Meo K, Kaplan EL. Five vs ten days of penicillin V therapy for streptococcal pharyngitis. Am J Dis Child. 1987 Feb;141(2):224-7 | PubMed |
- Hamill J. Multicentre evaluation of azithromycin and penicillin V in the treatment of acute streptococcal pharyngitis and tonsillitis in children. J Antimicrob Chemother. 1993 Jun;31 Suppl E:89-94 | PubMed |
- Hooton TM. A comparison of azithromycin and penicillin V for the treatment of streptococcal pharyngitis. Am J Med. 1991 Sep 12;91(3A):23S-26S | PubMed |
- Kafetzis DA, Liapi G, Tsolia M, Aoudi H, Mathioudakis J, Paraskakis I, et al. Failure to eradicate Group A beta-haemolytic streptococci (GABHS) from the upper respiratory tract after antibiotic treatment. Int J Antimicrob Agents. 2004 Jan;23(1):67-71 | PubMed |
- Kaplan EL, Gooch III WM, Notario GF, Craft JC. Macrolide therapy of group A streptococcal pharyngitis: 10 days of macrolide therapy (clarithromycin) is more effective in streptococcal eradication than 5 days (azithromycin). Clin Infect Dis. 2001 Jun 15;32(12):1798-802 | PubMed |
- McCarty J, Hedrick JA, Gooch WM. Clarithromycin suspension vs penicillin V suspension in children with streptococcal pharyngitis. Adv Ther. 2000 Jan-Feb;17(1):14-26 | PubMed |
- Mehra S, van Moerkerke M, Welck J, Sverrisson G, Sirotiakova J, Marr C, et al. Short course therapy with cefuroxime axetil for group A streptococcal tonsillopharyngitis in children. Pediatr Infect Dis J. 1998 Jun;17(6):452-7 | PubMed |
- Milatovic D. Evaluation of cefadroxil, penicillin and erythromycin in the treatment of streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 1991 Oct;10(10 Suppl):S61-3 | PubMed |
- Müller O. Comparison of azithromycin versus clarithromycin in the treatment of patients with upper respiratory tract infections. J Antimicrob Chemother. 1993 Jun;31 Suppl E:137-46 | PubMed |
- Müller O. An open comparative study of azithromycin and roxithromycin in the treatment of acute upper respiratory tract infections. J Antimicrob Chemother. 1996 Jun;37 Suppl C:83-92 | PubMed |
- Norrby SR, Rabie WJ, Bacart P, Mueller O, Leroy B, Rangaraju M, et al. Efficacy of short-course therapy with the ketolide telithromycin compared with 10 days of penicillin V for the treatment of pharyngitis/tonsillitis. Scand J Infect Dis. 2001;33(12):883-90 | PubMed |
- O'Doherty B. An open comparative study of azithromycin versus cefaclor in the treatment of patients with upper respiratory tract infections. J Antimicrob Chemother. 1996 Jun;37 Suppl C:71-81 | PubMed |
- O'Doherty B. Azithromycin versus penicillin V in the treatment of paediatric patients with acute streptococcal pharyngitis/tonsillitis. Paediatric azithromycin Study Group. Eur J Clin Microbiol Infect Dis. 1996 Sep;15(9):718-24 | PubMed |
- Pacifico L, Scopetti F, Ranucci A, Pataracchia M, Savignoni F, Chiesa C. Comparative efficacy and safety of 3-day azithromycin and 10-day penicillin V treatment of group A beta-hemolytic streptococcal pharyngitis in children. Antimicrob Agents Chemother. 1996 Apr;40(4):1005-8 | PubMed |
- Padilla-Raygoza N. Comparison of clarithromycin and azithromycin for treatment of streptococcal pharyngotonsillitis in children. Infections in Medicine. 1998;15:23-27. | Link |
- Pavesio D, Pecco P, Peisino MG. Short-term treatment of streptococcal tonsillitis with ceftriaxone. Chemotherapy. 1988;34 Suppl 1:34-8 | PubMed | Link |
- Peixoto E, Ramet J, Kissling M. Cefetamet pivoxil in pharyngotonsillitis due to group A beta-hemolytic streptococci. Current therapeutic research. 1993;53(6):694-706. | Link |
- Peyramond D, Tigaud S, Bremard-Oury C, Scheimberg A. Multicenter comparative trial of cefixime and phenoxymethylpenicillin for group a beta-hemolytic streptococcal tonsillitis. Current Therapeutic Research. 1994;55:14-21. | Link |
- Peyramond D, Portier H, Geslin P, Cohen R. 6-day amoxicillin versus 10-day penicillin V for group A beta-haemolytic streptococcal acute tonsillitis in adults: a French multicentre, open-label, randomized study. The French Study Group Clamorange. Scand J Infect Dis. 1996;28(5):497-501 | PubMed |
- Pichichero ME, Gooch WM, Rodriguez W, Blumer JL, Aronoff SC, Jacobs RF, et al. Effective short-course treatment of acute group A beta-hemolytic streptococcal tonsillopharyngitis. Ten days of penicillin V vs 5 days or 10 days of cefpodoxime therapy in children. Arch Pediatr Adolesc Med. 1994 Oct;148(10):1053-60 | PubMed |
- Portier H, Chavanet P, Gouyon JB, Guetat F. Five day treatment of pharyngotonsillitis with cefpodoxime proxetil. J Antimicrob Chemother. 1990 Dec;26 Suppl E:79-85 | PubMed |
- Portier H, Chavanet P, Waldner-Combernoux A, Kisterman JP, Grey PC, Ichou F, et al. Five versus ten days treatment of streptococcal pharyngotonsillitis: a randomized controlled trial comparing cefpodoxime proxetil and phenoxymethyl penicillin. Scand J Infect Dis. 1994;26(1):59-66 | PubMed |
- Portier H, Lucht F, Lescale O, Kazmierczak A, Ros A, Scheimberg A. Multicenter comparative trial and penicillin V as treatment of group a beta hemolytic streptococcus (GABHS) pharyngitis. Médecine et Maladies Infectieuses. 1995;25(10):1005-1010. | Link |
- Portier H, Bourrillon A, Lucht F, Choutet P, Géhanno P, Meziane L, et al. [Treatment of acute group A beta-hemolytic streptococcal tonsillitis in children with a 5-day course of josamycin]. Arch Pediatr. 2001 Jul;8(7):700-6 | PubMed |
- Portier H, Filipecki J, Weber P, Goldfarb G, Lethuaire D, Chauvin JP. Five day clarithromycin modified release versus 10 day penicillin V for group A streptococcal pharyngitis: a multi-centre, open-label, randomized study. J Antimicrob Chemother. 2002 Feb;49(2):337-44 | PubMed |
- Schaad UB, Heynen G. Evaluation of the efficacy, safety and toleration of azithromycin vs. penicillin V in the treatment of acute streptococcal pharyngitis in children: results of a multicenter, open comparative study. The Swiss Tonsillopharyngitis Study Group. Pediatr Infect Dis J. 1996 Sep;15(9):791-5 | PubMed |
- Schaad UB, Kellerhals P, Altwegg M; Swiss Pharyngitis Study Group. Azithromycin versus penicillin V for treatment of acute group A streptococcal pharyngitis. Pediatr Infect Dis J. 2002 Apr;21(4):304-8 | PubMed |
- Scholz H. Streptococcal-A tonsillopharyngitis: a 5-day course of cefuroxime axetil versus a 10-day course of penicillin V. results depending on the children's age. Chemotherapy. 2004 Apr;50(1):51-4 | PubMed |
- Schwartz RH, Wientzen RL Jr, Pedreira F, Feroli EJ, Mella GW, Guandolo VL. Penicillin V for group A streptococcal pharyngotonsillitis. A randomized trial of seven vs ten days' therapy. JAMA. 1981 Oct 16;246(16):1790-5 | PubMed |
- Sinanian R, Ruoff G, Panzer J, Atkinson W. Streptococcal pharyngitis: a comparison of the eradication of the organism by 5- and 10-day antibiotic therapy. Curr Ther Res Clin Exp. 1972 Nov;14(11):716-20 | PubMed |
- Still JG. Azithromycin suspension vs penicillin suspension in treatment of children with streptococcal pharyngitis. CLINICAL PHARMACOLOGY & THERAPEUTICS. 1993;53(2):195-195. | Link |
- Still JG. Treatment of streptococcal pharyngitis in children with five days of azithromycin suspension, abstr. M67. 34th Interscience Conference on Antimicrobial Agents and Chemotherapy. American Society for Microbiology, Washington, DC. 1994:246 | Link |
- Still JG. Management of pediatric patients with group A beta-hemolytic Streptococcus pharyngitis: treatment options. The Pediatric infectious disease journal. 1995;14(4):S57-61 | Link |
- Strömberg A, Schwan A, Cars O. Five versus ten days treatment of group A streptococcal pharyngotonsillitis: a randomized controlled clinical trial with phenoxymethylpenicillin and cefadroxil. Scand J Infect Dis. 1988;20(1):37-46 | PubMed |
- Syrogiannopoulos GA, Bozdogan B, Grivea IN, Ednie LM, Kritikou DI, Katopodis GD, et al. Two dosages of clarithromycin for five days, amoxicillin/clavulanate for five days or penicillin V for ten days in acute group A streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 2004 Sep;23(9):857-65 | PubMed |
- Tack KJ, Hedrick JA, Rothstein E, Nemeth MA, Keyserling C, Pichichero ME. A study of 5-day cefdinir treatment for streptococcal pharyngitis in children. Cefdinir Pediatric Pharyngitis Study Group. Arch Pediatr Adolesc Med. 1997 Jan;151(1):45-9 | PubMed |
- Tack KJ, Henry DC, Gooch WM, Brink DN, Keyserling CH. Five-day cefdinir treatment for streptococcal pharyngitis. Cefdinir Pharyngitis Study Group. Antimicrob Agents Chemother. 1998 May;42(5):1073-5 | PubMed |
- Takker U, Dzyublyk O, Busman T, Notario G. Comparison of 5 days of extended-release clarithromycin versus 10 days of penicillin V for the treatment of streptococcal pharyngitis/tonsillitis: results of a multicenter, double-blind, randomized study in adolescent and adult patients. Curr Med Res Opin. 2003;19(5):421-9 | PubMed |
- Venuta A, Laudizi L, Beverelli A, Bettelli F, Milioli S, Garetti E. Azithromycin compared with clarithromycin for the treatment of streptococcal pharyngitis in children. J Int Med Res. 1998 Jun-Jul;26(3):152-8 | PubMed |
- Weippl G. Multicentre comparison of azithromycin versus erythromycin in the treatment of paediatric pharyngitis or tonsillitis caused by group A streptococci. J Antimicrob Chemother. 1993 Jun;31 Suppl E:95-101 | PubMed |
- Zwart S, Sachs AP, Ruijs GJ, Gubbels JW, Hoes AW, de Melker RA. Penicillin for acute sore throat: randomised double blind trial of seven days versus three days treatment or placebo in adults. BMJ. 2000 Jan 15;320(7228):150-4 | PubMed |
- Zwart S, Rovers MM, de Melker RA, Hoes AW. Penicillin for acute sore throat in children: randomised, double blind trial. BMJ. 2003 Dec 6;327(7427):1324 | PubMed |
- Piñeiro Pérez R, Hijano Bandera F, Alvez González F, Fernández Landaluce A, Silva Rico JC, Pérez Cánovas C, et al. [Consensus document on the diagnosis and treatment of acute tonsillopharyngitis]. An Pediatr (Barc). 2011 Nov;75(5):342.e1-13 | CrossRef | PubMed |
- Randel A; Infectious Disease Society of America. IDSA Updates Guideline for Managing Group A Streptococcal Pharyngitis. Am Fam Physician. 2013 Sep 1;88(5):338-40 | PubMed |
- Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012 Nov 15;55(10):1279-82 | CrossRef | PubMed |
 Altamimi S, Khalil A, Khalaiwi KA, Milner RA, Pusic MV, Al Othman MA. Short-term late-generation antibiotics versus longer term penicillin for acute streptococcal pharyngitis in children. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD004872 | CrossRef | PubMed |
Altamimi S, Khalil A, Khalaiwi KA, Milner RA, Pusic MV, Al Othman MA. Short-term late-generation antibiotics versus longer term penicillin for acute streptococcal pharyngitis in children. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD004872 | CrossRef | PubMed | Casey JR, Pichichero ME. Metaanalysis of short course antibiotic treatment for group a streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 2005 Oct;24(10):909-17 | PubMed |
Casey JR, Pichichero ME. Metaanalysis of short course antibiotic treatment for group a streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 2005 Oct;24(10):909-17 | PubMed | Casey JR, Pichichero ME. Higher dosages of azithromycin are more effective in treatment of group A streptococcal tonsillopharyngitis. Clin Infect Dis. 2005 Jun 15;40(12):1748-55 | PubMed |
Casey JR, Pichichero ME. Higher dosages of azithromycin are more effective in treatment of group A streptococcal tonsillopharyngitis. Clin Infect Dis. 2005 Jun 15;40(12):1748-55 | PubMed | Falagas ME, Vouloumanou EK, Matthaiou DK, Kapaskelis AM, Karageorgopoulos DE. Effectiveness and safety of short-course vs long-course antibiotic therapy for group a beta hemolytic streptococcal tonsillopharyngitis: a meta-analysis of randomized trials. Mayo Clin Proc. 2008 Aug;83(8):880-9 | PubMed |
Falagas ME, Vouloumanou EK, Matthaiou DK, Kapaskelis AM, Karageorgopoulos DE. Effectiveness and safety of short-course vs long-course antibiotic therapy for group a beta hemolytic streptococcal tonsillopharyngitis: a meta-analysis of randomized trials. Mayo Clin Proc. 2008 Aug;83(8):880-9 | PubMed | Pichichero ME, Casey JR. Bacterial eradication rates with shortened courses of 2nd- and 3rd-generation cephalosporins versus 10 days of penicillin for treatment of group A streptococcal tonsillopharyngitis in adults. Diagn Microbiol Infect Dis. 2007 Oct;59(2):127-30 | PubMed |
Pichichero ME, Casey JR. Bacterial eradication rates with shortened courses of 2nd- and 3rd-generation cephalosporins versus 10 days of penicillin for treatment of group A streptococcal tonsillopharyngitis in adults. Diagn Microbiol Infect Dis. 2007 Oct;59(2):127-30 | PubMed | Adam D, Hostalek U, Tröster K. 5-day cefixime therapy for bacterial pharyngitis and/or tonsillitis: comparison with 10-day penicillin V therapy. Cefixime Study Group. Infection. 1995;23 Suppl 2:S83-6 | PubMed |
Adam D, Hostalek U, Tröster K. 5-day cefixime therapy for bacterial pharyngitis and/or tonsillitis: comparison with 10-day penicillin V therapy. Cefixime Study Group. Infection. 1995;23 Suppl 2:S83-6 | PubMed | Adam D, Scholz H. Five days of erythromycin estolate versus ten days of penicillin V in the treatment of group A streptococcal tonsillopharyngitis in children. Pharyngitis Study Group. Eur J Clin Microbiol Infect Dis. 1996 Sep;15(9):712-7 | PubMed |
Adam D, Scholz H. Five days of erythromycin estolate versus ten days of penicillin V in the treatment of group A streptococcal tonsillopharyngitis in children. Pharyngitis Study Group. Eur J Clin Microbiol Infect Dis. 1996 Sep;15(9):712-7 | PubMed | Adam D, Scholz H, Helmerking M. Comparison of short-course (5 day) cefuroxime axetil with a standard 10 day oral penicillin V regimen in the treatment of tonsillopharyngitis. J Antimicrob Chemother. 2000 Feb;45 Suppl:23-30 | PubMed |
Adam D, Scholz H, Helmerking M. Comparison of short-course (5 day) cefuroxime axetil with a standard 10 day oral penicillin V regimen in the treatment of tonsillopharyngitis. J Antimicrob Chemother. 2000 Feb;45 Suppl:23-30 | PubMed | Adam D, Scholz H, Helmerking M. Short-course antibiotic treatment of 4782 culture-proven cases of group A streptococcal tonsillopharyngitis and incidence of poststreptococcal sequelae. J Infect Dis. 2000 Aug;182(2):509-16 | PubMed |
Adam D, Scholz H, Helmerking M. Short-course antibiotic treatment of 4782 culture-proven cases of group A streptococcal tonsillopharyngitis and incidence of poststreptococcal sequelae. J Infect Dis. 2000 Aug;182(2):509-16 | PubMed | Aujard Y, Boucot I, Brahimi N, Chiche D, Bingen E. Comparative efficacy and safety of four-day cefuroxime axetil and ten-day penicillin treatment of group A beta-hemolytic streptococcal pharyngitis in children. Pediatr Infect Dis J. 1995 Apr;14(4):295-300 | PubMed |
Aujard Y, Boucot I, Brahimi N, Chiche D, Bingen E. Comparative efficacy and safety of four-day cefuroxime axetil and ten-day penicillin treatment of group A beta-hemolytic streptococcal pharyngitis in children. Pediatr Infect Dis J. 1995 Apr;14(4):295-300 | PubMed | Carbon C, Chatelin A, Bingen E, Zuck P, Rio Y, Guetat F, et al. A double-blind randomized trial comparing the efficacy and safety of a 5-day course of cefotiam hexetil with that of a 10-day course of penicillin V in adult patients with pharyngitis caused by group A beta-haemolytic streptococci. J Antimicrob Chemother. 1995 Jun;35(6):843-54 | PubMed |
Carbon C, Chatelin A, Bingen E, Zuck P, Rio Y, Guetat F, et al. A double-blind randomized trial comparing the efficacy and safety of a 5-day course of cefotiam hexetil with that of a 10-day course of penicillin V in adult patients with pharyngitis caused by group A beta-haemolytic streptococci. J Antimicrob Chemother. 1995 Jun;35(6):843-54 | PubMed | Cohen R, Levy C, Doit C, De La Rocque F, Boucherat M, Fitoussi F, et al. Six-day amoxicillin vs. ten-day penicillin V therapy for group A streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 1996 Aug;15(8):678-82 | PubMed |
Cohen R, Levy C, Doit C, De La Rocque F, Boucherat M, Fitoussi F, et al. Six-day amoxicillin vs. ten-day penicillin V therapy for group A streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 1996 Aug;15(8):678-82 | PubMed | Cohen R, Reinert P, De La Rocque F, Levy C, Boucherat M, Robert M, et al. Comparison of two dosages of azithromycin for three days versus penicillin V for ten days in acute group A streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 2002 Apr;21(4):297-303 | PubMed |
Cohen R, Reinert P, De La Rocque F, Levy C, Boucherat M, Robert M, et al. Comparison of two dosages of azithromycin for three days versus penicillin V for ten days in acute group A streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 2002 Apr;21(4):297-303 | PubMed | Cremer J, Wallrauch C, Milatovic D, Braveny I. Azithromycin versus cefaclor in the treatment of pediatric patients with acute group A beta-hemolytic streptococcal tonsillopharyngitis. Eur J Clin Microbiol Infect Dis. 1998 Apr;17(4):235-9 | PubMed |
Cremer J, Wallrauch C, Milatovic D, Braveny I. Azithromycin versus cefaclor in the treatment of pediatric patients with acute group A beta-hemolytic streptococcal tonsillopharyngitis. Eur J Clin Microbiol Infect Dis. 1998 Apr;17(4):235-9 | PubMed | Esposito S, Noviello S, Ianniello F, D'Errico G. Short-course therapy with cefaclor for treatment of streptococcal pharyngotonsillitis. Int J Antimicrob Agents. 2001 Oct;18(4):341-5 | PubMed |
Esposito S, Noviello S, Ianniello F, D'Errico G. Short-course therapy with cefaclor for treatment of streptococcal pharyngotonsillitis. Int J Antimicrob Agents. 2001 Oct;18(4):341-5 | PubMed | García Callejo FJ, Velert Vila MM, Orts Alborch MH, Pardo Mateu L, Esparcia Navarro M. [Comparison of azithromycin, amoxicillin/clavulanic acid and cefaclor in the treatment of acute ENT infections]. Acta Otorrinolaringol Esp. 1998 May;49(4):306-12 | PubMed |
García Callejo FJ, Velert Vila MM, Orts Alborch MH, Pardo Mateu L, Esparcia Navarro M. [Comparison of azithromycin, amoxicillin/clavulanic acid and cefaclor in the treatment of acute ENT infections]. Acta Otorrinolaringol Esp. 1998 May;49(4):306-12 | PubMed | Gehanno P, Chiche D. Treatment of group a beta hemolytic streptococcal tonsillitis with cefuroxime axetil for 4 days : a comparative study with penicillin v for 10 days. Médecine et Maladies Infectieuses. 1991;21:66-70 | Link |
Gehanno P, Chiche D. Treatment of group a beta hemolytic streptococcal tonsillitis with cefuroxime axetil for 4 days : a comparative study with penicillin v for 10 days. Médecine et Maladies Infectieuses. 1991;21:66-70 | Link | Gerber MA, Randolph MF, Chanatry J, Wright LL, De Meo K, Kaplan EL. Five vs ten days of penicillin V therapy for streptococcal pharyngitis. Am J Dis Child. 1987 Feb;141(2):224-7 | PubMed |
Gerber MA, Randolph MF, Chanatry J, Wright LL, De Meo K, Kaplan EL. Five vs ten days of penicillin V therapy for streptococcal pharyngitis. Am J Dis Child. 1987 Feb;141(2):224-7 | PubMed | Hamill J. Multicentre evaluation of azithromycin and penicillin V in the treatment of acute streptococcal pharyngitis and tonsillitis in children. J Antimicrob Chemother. 1993 Jun;31 Suppl E:89-94 | PubMed |
Hamill J. Multicentre evaluation of azithromycin and penicillin V in the treatment of acute streptococcal pharyngitis and tonsillitis in children. J Antimicrob Chemother. 1993 Jun;31 Suppl E:89-94 | PubMed | Hooton TM. A comparison of azithromycin and penicillin V for the treatment of streptococcal pharyngitis. Am J Med. 1991 Sep 12;91(3A):23S-26S | PubMed |
Hooton TM. A comparison of azithromycin and penicillin V for the treatment of streptococcal pharyngitis. Am J Med. 1991 Sep 12;91(3A):23S-26S | PubMed | Kafetzis DA, Liapi G, Tsolia M, Aoudi H, Mathioudakis J, Paraskakis I, et al. Failure to eradicate Group A beta-haemolytic streptococci (GABHS) from the upper respiratory tract after antibiotic treatment. Int J Antimicrob Agents. 2004 Jan;23(1):67-71 | PubMed |
Kafetzis DA, Liapi G, Tsolia M, Aoudi H, Mathioudakis J, Paraskakis I, et al. Failure to eradicate Group A beta-haemolytic streptococci (GABHS) from the upper respiratory tract after antibiotic treatment. Int J Antimicrob Agents. 2004 Jan;23(1):67-71 | PubMed | Kaplan EL, Gooch III WM, Notario GF, Craft JC. Macrolide therapy of group A streptococcal pharyngitis: 10 days of macrolide therapy (clarithromycin) is more effective in streptococcal eradication than 5 days (azithromycin). Clin Infect Dis. 2001 Jun 15;32(12):1798-802 | PubMed |
Kaplan EL, Gooch III WM, Notario GF, Craft JC. Macrolide therapy of group A streptococcal pharyngitis: 10 days of macrolide therapy (clarithromycin) is more effective in streptococcal eradication than 5 days (azithromycin). Clin Infect Dis. 2001 Jun 15;32(12):1798-802 | PubMed | McCarty J, Hedrick JA, Gooch WM. Clarithromycin suspension vs penicillin V suspension in children with streptococcal pharyngitis. Adv Ther. 2000 Jan-Feb;17(1):14-26 | PubMed |
McCarty J, Hedrick JA, Gooch WM. Clarithromycin suspension vs penicillin V suspension in children with streptococcal pharyngitis. Adv Ther. 2000 Jan-Feb;17(1):14-26 | PubMed | Mehra S, van Moerkerke M, Welck J, Sverrisson G, Sirotiakova J, Marr C, et al. Short course therapy with cefuroxime axetil for group A streptococcal tonsillopharyngitis in children. Pediatr Infect Dis J. 1998 Jun;17(6):452-7 | PubMed |
Mehra S, van Moerkerke M, Welck J, Sverrisson G, Sirotiakova J, Marr C, et al. Short course therapy with cefuroxime axetil for group A streptococcal tonsillopharyngitis in children. Pediatr Infect Dis J. 1998 Jun;17(6):452-7 | PubMed | Milatovic D. Evaluation of cefadroxil, penicillin and erythromycin in the treatment of streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 1991 Oct;10(10 Suppl):S61-3 | PubMed |
Milatovic D. Evaluation of cefadroxil, penicillin and erythromycin in the treatment of streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 1991 Oct;10(10 Suppl):S61-3 | PubMed | Müller O. Comparison of azithromycin versus clarithromycin in the treatment of patients with upper respiratory tract infections. J Antimicrob Chemother. 1993 Jun;31 Suppl E:137-46 | PubMed |
Müller O. Comparison of azithromycin versus clarithromycin in the treatment of patients with upper respiratory tract infections. J Antimicrob Chemother. 1993 Jun;31 Suppl E:137-46 | PubMed | Müller O. An open comparative study of azithromycin and roxithromycin in the treatment of acute upper respiratory tract infections. J Antimicrob Chemother. 1996 Jun;37 Suppl C:83-92 | PubMed |
Müller O. An open comparative study of azithromycin and roxithromycin in the treatment of acute upper respiratory tract infections. J Antimicrob Chemother. 1996 Jun;37 Suppl C:83-92 | PubMed | Norrby SR, Rabie WJ, Bacart P, Mueller O, Leroy B, Rangaraju M, et al. Efficacy of short-course therapy with the ketolide telithromycin compared with 10 days of penicillin V for the treatment of
pharyngitis/tonsillitis. Scand J Infect Dis. 2001;33(12):883-90
| PubMed |
Norrby SR, Rabie WJ, Bacart P, Mueller O, Leroy B, Rangaraju M, et al. Efficacy of short-course therapy with the ketolide telithromycin compared with 10 days of penicillin V for the treatment of
pharyngitis/tonsillitis. Scand J Infect Dis. 2001;33(12):883-90
| PubMed | O'Doherty B. An open comparative study of azithromycin versus cefaclor in the treatment of patients with upper respiratory tract infections. J Antimicrob Chemother. 1996 Jun;37 Suppl C:71-81 | PubMed |
O'Doherty B. An open comparative study of azithromycin versus cefaclor in the treatment of patients with upper respiratory tract infections. J Antimicrob Chemother. 1996 Jun;37 Suppl C:71-81 | PubMed | O'Doherty B. Azithromycin versus penicillin V in the treatment of paediatric patients with acute streptococcal pharyngitis/tonsillitis. Paediatric azithromycin Study Group. Eur J Clin Microbiol Infect Dis. 1996 Sep;15(9):718-24 | PubMed |
O'Doherty B. Azithromycin versus penicillin V in the treatment of paediatric patients with acute streptococcal pharyngitis/tonsillitis. Paediatric azithromycin Study Group. Eur J Clin Microbiol Infect Dis. 1996 Sep;15(9):718-24 | PubMed | Pacifico L, Scopetti F, Ranucci A, Pataracchia M, Savignoni F, Chiesa C. Comparative efficacy and safety of 3-day azithromycin and 10-day penicillin V treatment of group A beta-hemolytic streptococcal pharyngitis in children. Antimicrob Agents Chemother. 1996 Apr;40(4):1005-8 | PubMed |
Pacifico L, Scopetti F, Ranucci A, Pataracchia M, Savignoni F, Chiesa C. Comparative efficacy and safety of 3-day azithromycin and 10-day penicillin V treatment of group A beta-hemolytic streptococcal pharyngitis in children. Antimicrob Agents Chemother. 1996 Apr;40(4):1005-8 | PubMed | Padilla-Raygoza N. Comparison of clarithromycin and azithromycin for treatment of streptococcal pharyngotonsillitis in children. Infections in Medicine. 1998;15:23-27. | Link |
Padilla-Raygoza N. Comparison of clarithromycin and azithromycin for treatment of streptococcal pharyngotonsillitis in children. Infections in Medicine. 1998;15:23-27. | Link | Pavesio D, Pecco P, Peisino MG. Short-term treatment of streptococcal tonsillitis with ceftriaxone. Chemotherapy. 1988;34 Suppl 1:34-8 | PubMed | Link |
Pavesio D, Pecco P, Peisino MG. Short-term treatment of streptococcal tonsillitis with ceftriaxone. Chemotherapy. 1988;34 Suppl 1:34-8 | PubMed | Link | Peixoto E, Ramet J, Kissling M. Cefetamet pivoxil in pharyngotonsillitis due to group A beta-hemolytic streptococci. Current therapeutic research. 1993;53(6):694-706. | Link |
Peixoto E, Ramet J, Kissling M. Cefetamet pivoxil in pharyngotonsillitis due to group A beta-hemolytic streptococci. Current therapeutic research. 1993;53(6):694-706. | Link | Peyramond D, Tigaud S, Bremard-Oury C, Scheimberg A. Multicenter comparative trial of cefixime and phenoxymethylpenicillin for group a beta-hemolytic streptococcal tonsillitis. Current Therapeutic Research. 1994;55:14-21. | Link |
Peyramond D, Tigaud S, Bremard-Oury C, Scheimberg A. Multicenter comparative trial of cefixime and phenoxymethylpenicillin for group a beta-hemolytic streptococcal tonsillitis. Current Therapeutic Research. 1994;55:14-21. | Link | Peyramond D, Portier H, Geslin P, Cohen R. 6-day amoxicillin versus 10-day penicillin V for group A beta-haemolytic streptococcal acute tonsillitis in adults: a French multicentre, open-label, randomized study. The French Study Group Clamorange. Scand J Infect Dis. 1996;28(5):497-501 | PubMed |
Peyramond D, Portier H, Geslin P, Cohen R. 6-day amoxicillin versus 10-day penicillin V for group A beta-haemolytic streptococcal acute tonsillitis in adults: a French multicentre, open-label, randomized study. The French Study Group Clamorange. Scand J Infect Dis. 1996;28(5):497-501 | PubMed | Pichichero ME, Gooch WM, Rodriguez W, Blumer JL, Aronoff SC, Jacobs RF, et al. Effective short-course treatment of acute group A beta-hemolytic streptococcal tonsillopharyngitis. Ten days of penicillin V vs 5 days or 10 days of cefpodoxime therapy in children. Arch Pediatr Adolesc Med. 1994 Oct;148(10):1053-60 | PubMed |
Pichichero ME, Gooch WM, Rodriguez W, Blumer JL, Aronoff SC, Jacobs RF, et al. Effective short-course treatment of acute group A beta-hemolytic streptococcal tonsillopharyngitis. Ten days of penicillin V vs 5 days or 10 days of cefpodoxime therapy in children. Arch Pediatr Adolesc Med. 1994 Oct;148(10):1053-60 | PubMed | Portier H, Chavanet P, Gouyon JB, Guetat F. Five day treatment of pharyngotonsillitis with cefpodoxime proxetil. J Antimicrob Chemother. 1990 Dec;26 Suppl E:79-85 | PubMed |
Portier H, Chavanet P, Gouyon JB, Guetat F. Five day treatment of pharyngotonsillitis with cefpodoxime proxetil. J Antimicrob Chemother. 1990 Dec;26 Suppl E:79-85 | PubMed | Portier H, Chavanet P, Waldner-Combernoux A, Kisterman JP, Grey PC, Ichou F, et al. Five versus ten days treatment of streptococcal pharyngotonsillitis: a randomized controlled trial comparing cefpodoxime proxetil and phenoxymethyl penicillin. Scand J Infect Dis. 1994;26(1):59-66 | PubMed |
Portier H, Chavanet P, Waldner-Combernoux A, Kisterman JP, Grey PC, Ichou F, et al. Five versus ten days treatment of streptococcal pharyngotonsillitis: a randomized controlled trial comparing cefpodoxime proxetil and phenoxymethyl penicillin. Scand J Infect Dis. 1994;26(1):59-66 | PubMed | Portier H, Lucht F, Lescale O, Kazmierczak A, Ros A, Scheimberg A. Multicenter comparative trial and penicillin V as treatment of group a beta hemolytic streptococcus (GABHS) pharyngitis. Médecine et Maladies Infectieuses. 1995;25(10):1005-1010. | Link |
Portier H, Lucht F, Lescale O, Kazmierczak A, Ros A, Scheimberg A. Multicenter comparative trial and penicillin V as treatment of group a beta hemolytic streptococcus (GABHS) pharyngitis. Médecine et Maladies Infectieuses. 1995;25(10):1005-1010. | Link | Portier H, Bourrillon A, Lucht F, Choutet P, Géhanno P, Meziane L, et al. [Treatment of acute group A beta-hemolytic streptococcal tonsillitis in children with a 5-day course of josamycin]. Arch Pediatr. 2001 Jul;8(7):700-6 | PubMed |
Portier H, Bourrillon A, Lucht F, Choutet P, Géhanno P, Meziane L, et al. [Treatment of acute group A beta-hemolytic streptococcal tonsillitis in children with a 5-day course of josamycin]. Arch Pediatr. 2001 Jul;8(7):700-6 | PubMed | Portier H, Filipecki J, Weber P, Goldfarb G, Lethuaire D, Chauvin JP. Five day clarithromycin modified release versus 10 day penicillin V for group A streptococcal pharyngitis: a multi-centre, open-label, randomized study. J Antimicrob Chemother. 2002 Feb;49(2):337-44 | PubMed |
Portier H, Filipecki J, Weber P, Goldfarb G, Lethuaire D, Chauvin JP. Five day clarithromycin modified release versus 10 day penicillin V for group A streptococcal pharyngitis: a multi-centre, open-label, randomized study. J Antimicrob Chemother. 2002 Feb;49(2):337-44 | PubMed | Schaad UB, Heynen G. Evaluation of the efficacy, safety and toleration of azithromycin vs. penicillin V in the treatment of acute streptococcal pharyngitis in children: results of a multicenter, open comparative study. The Swiss Tonsillopharyngitis Study Group. Pediatr Infect Dis J. 1996 Sep;15(9):791-5 | PubMed |
Schaad UB, Heynen G. Evaluation of the efficacy, safety and toleration of azithromycin vs. penicillin V in the treatment of acute streptococcal pharyngitis in children: results of a multicenter, open comparative study. The Swiss Tonsillopharyngitis Study Group. Pediatr Infect Dis J. 1996 Sep;15(9):791-5 | PubMed | Schaad UB, Kellerhals P, Altwegg M; Swiss Pharyngitis Study Group. Azithromycin versus penicillin V for treatment of acute group A streptococcal pharyngitis. Pediatr Infect Dis J. 2002 Apr;21(4):304-8 | PubMed |
Schaad UB, Kellerhals P, Altwegg M; Swiss Pharyngitis Study Group. Azithromycin versus penicillin V for treatment of acute group A streptococcal pharyngitis. Pediatr Infect Dis J. 2002 Apr;21(4):304-8 | PubMed | Scholz H. Streptococcal-A tonsillopharyngitis: a 5-day course of cefuroxime axetil versus a 10-day course of penicillin V. results depending on the children's age. Chemotherapy. 2004 Apr;50(1):51-4 | PubMed |
Scholz H. Streptococcal-A tonsillopharyngitis: a 5-day course of cefuroxime axetil versus a 10-day course of penicillin V. results depending on the children's age. Chemotherapy. 2004 Apr;50(1):51-4 | PubMed | Schwartz RH, Wientzen RL Jr, Pedreira F, Feroli EJ, Mella GW, Guandolo VL. Penicillin V for group A streptococcal pharyngotonsillitis. A randomized trial of seven vs ten days' therapy. JAMA. 1981 Oct 16;246(16):1790-5 | PubMed |
Schwartz RH, Wientzen RL Jr, Pedreira F, Feroli EJ, Mella GW, Guandolo VL. Penicillin V for group A streptococcal pharyngotonsillitis. A randomized trial of seven vs ten days' therapy. JAMA. 1981 Oct 16;246(16):1790-5 | PubMed | Sinanian R, Ruoff G, Panzer J, Atkinson W. Streptococcal pharyngitis: a comparison of the eradication of the organism by 5- and 10-day antibiotic therapy. Curr Ther Res Clin Exp. 1972 Nov;14(11):716-20 | PubMed |
Sinanian R, Ruoff G, Panzer J, Atkinson W. Streptococcal pharyngitis: a comparison of the eradication of the organism by 5- and 10-day antibiotic therapy. Curr Ther Res Clin Exp. 1972 Nov;14(11):716-20 | PubMed | Still JG. Azithromycin suspension vs penicillin suspension in treatment of children with streptococcal pharyngitis. CLINICAL PHARMACOLOGY & THERAPEUTICS. 1993;53(2):195-195. | Link |
Still JG. Azithromycin suspension vs penicillin suspension in treatment of children with streptococcal pharyngitis. CLINICAL PHARMACOLOGY & THERAPEUTICS. 1993;53(2):195-195. | Link | Still JG. Treatment of streptococcal pharyngitis in children with five days of azithromycin suspension, abstr. M67. 34th Interscience Conference on Antimicrobial Agents and Chemotherapy. American Society for Microbiology, Washington, DC. 1994:246 | Link |
Still JG. Treatment of streptococcal pharyngitis in children with five days of azithromycin suspension, abstr. M67. 34th Interscience Conference on Antimicrobial Agents and Chemotherapy. American Society for Microbiology, Washington, DC. 1994:246 | Link | Still JG. Management of pediatric patients with group A beta-hemolytic Streptococcus pharyngitis: treatment options. The Pediatric infectious disease journal. 1995;14(4):S57-61 | Link |
Still JG. Management of pediatric patients with group A beta-hemolytic Streptococcus pharyngitis: treatment options. The Pediatric infectious disease journal. 1995;14(4):S57-61 | Link | Strömberg A, Schwan A, Cars O. Five versus ten days treatment of group A streptococcal pharyngotonsillitis: a randomized controlled clinical trial with phenoxymethylpenicillin and cefadroxil. Scand J Infect Dis. 1988;20(1):37-46 | PubMed |
Strömberg A, Schwan A, Cars O. Five versus ten days treatment of group A streptococcal pharyngotonsillitis: a randomized controlled clinical trial with phenoxymethylpenicillin and cefadroxil. Scand J Infect Dis. 1988;20(1):37-46 | PubMed | Syrogiannopoulos GA, Bozdogan B, Grivea IN, Ednie LM, Kritikou DI, Katopodis GD, et al. Two dosages of clarithromycin for five days, amoxicillin/clavulanate for five days or penicillin V for ten days in acute group A streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 2004 Sep;23(9):857-65 | PubMed |
Syrogiannopoulos GA, Bozdogan B, Grivea IN, Ednie LM, Kritikou DI, Katopodis GD, et al. Two dosages of clarithromycin for five days, amoxicillin/clavulanate for five days or penicillin V for ten days in acute group A streptococcal tonsillopharyngitis. Pediatr Infect Dis J. 2004 Sep;23(9):857-65 | PubMed | Tack KJ, Hedrick JA, Rothstein E, Nemeth MA, Keyserling C, Pichichero ME. A study of 5-day cefdinir treatment for streptococcal pharyngitis in children. Cefdinir Pediatric Pharyngitis Study Group. Arch Pediatr Adolesc Med. 1997 Jan;151(1):45-9 | PubMed |
Tack KJ, Hedrick JA, Rothstein E, Nemeth MA, Keyserling C, Pichichero ME. A study of 5-day cefdinir treatment for streptococcal pharyngitis in children. Cefdinir Pediatric Pharyngitis Study Group. Arch Pediatr Adolesc Med. 1997 Jan;151(1):45-9 | PubMed | Tack KJ, Henry DC, Gooch WM, Brink DN, Keyserling CH. Five-day cefdinir treatment for streptococcal pharyngitis. Cefdinir Pharyngitis Study Group. Antimicrob Agents Chemother. 1998 May;42(5):1073-5 | PubMed |
Tack KJ, Henry DC, Gooch WM, Brink DN, Keyserling CH. Five-day cefdinir treatment for streptococcal pharyngitis. Cefdinir Pharyngitis Study Group. Antimicrob Agents Chemother. 1998 May;42(5):1073-5 | PubMed | Takker U, Dzyublyk O, Busman T, Notario G. Comparison of 5 days of extended-release clarithromycin versus 10 days of penicillin V for the treatment of streptococcal pharyngitis/tonsillitis: results of a multicenter, double-blind, randomized study in adolescent and adult patients. Curr Med Res Opin. 2003;19(5):421-9 | PubMed |
Takker U, Dzyublyk O, Busman T, Notario G. Comparison of 5 days of extended-release clarithromycin versus 10 days of penicillin V for the treatment of streptococcal pharyngitis/tonsillitis: results of a multicenter, double-blind, randomized study in adolescent and adult patients. Curr Med Res Opin. 2003;19(5):421-9 | PubMed | Venuta A, Laudizi L, Beverelli A, Bettelli F, Milioli S, Garetti E. Azithromycin compared with clarithromycin for the treatment of streptococcal pharyngitis in children. J Int Med Res. 1998 Jun-Jul;26(3):152-8 | PubMed |
Venuta A, Laudizi L, Beverelli A, Bettelli F, Milioli S, Garetti E. Azithromycin compared with clarithromycin for the treatment of streptococcal pharyngitis in children. J Int Med Res. 1998 Jun-Jul;26(3):152-8 | PubMed | Weippl G. Multicentre comparison of azithromycin versus erythromycin in the treatment of paediatric pharyngitis or tonsillitis caused by group A streptococci. J Antimicrob Chemother. 1993 Jun;31 Suppl E:95-101 | PubMed |
Weippl G. Multicentre comparison of azithromycin versus erythromycin in the treatment of paediatric pharyngitis or tonsillitis caused by group A streptococci. J Antimicrob Chemother. 1993 Jun;31 Suppl E:95-101 | PubMed | Zwart S, Sachs AP, Ruijs GJ, Gubbels JW, Hoes AW, de Melker RA. Penicillin for acute sore throat: randomised double blind trial of seven days versus three days treatment or placebo in adults. BMJ. 2000 Jan 15;320(7228):150-4 | PubMed |
Zwart S, Sachs AP, Ruijs GJ, Gubbels JW, Hoes AW, de Melker RA. Penicillin for acute sore throat: randomised double blind trial of seven days versus three days treatment or placebo in adults. BMJ. 2000 Jan 15;320(7228):150-4 | PubMed | Zwart S, Rovers MM, de Melker RA, Hoes AW. Penicillin for acute sore throat in children: randomised, double blind trial. BMJ. 2003 Dec 6;327(7427):1324 | PubMed |
Zwart S, Rovers MM, de Melker RA, Hoes AW. Penicillin for acute sore throat in children: randomised, double blind trial. BMJ. 2003 Dec 6;327(7427):1324 | PubMed | Piñeiro Pérez R, Hijano Bandera F, Alvez González F, Fernández Landaluce A, Silva Rico JC, Pérez Cánovas C, et al. [Consensus document on the diagnosis and treatment of acute tonsillopharyngitis]. An Pediatr (Barc). 2011 Nov;75(5):342.e1-13 | CrossRef | PubMed |
Piñeiro Pérez R, Hijano Bandera F, Alvez González F, Fernández Landaluce A, Silva Rico JC, Pérez Cánovas C, et al. [Consensus document on the diagnosis and treatment of acute tonsillopharyngitis]. An Pediatr (Barc). 2011 Nov;75(5):342.e1-13 | CrossRef | PubMed | Randel A; Infectious Disease Society of America. IDSA Updates Guideline for Managing Group A Streptococcal Pharyngitis. Am Fam Physician. 2013 Sep 1;88(5):338-40 | PubMed |
Randel A; Infectious Disease Society of America. IDSA Updates Guideline for Managing Group A Streptococcal Pharyngitis. Am Fam Physician. 2013 Sep 1;88(5):338-40 | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








