Abstract
Several beneficial effects have been proposed for cannabinoids in different clinical conditions, including epilepsy. However, their clinical role is controversial. Searching in Epistemonikos database, which is maintained by screening multiple databases, we identified five systematic reviews including four randomized trials addressing the question of this article. We extracted data and generated a summary of findings following the GRADE approach. We concluded it is not clear whether cannabinoids reduce the frequency of seizures in epilepsy because the certainty of the evidence is very low, and they probably increase adverse effects.
Problem
Epilepsy is a condition that disturbs the normal functioning of the brain and it is characterized by stereotyped and recurrent seizures. Although antiepileptic drugs usually achieve disease control, about 30% of patients have persistent seizures. Both tetrahydrocannabinol and cannabidiol have anticonvulsant properties by activating the CB1 and/or CB2 receptors of endocannabidiol system. However, their actual clinical role is not clear.
Methods
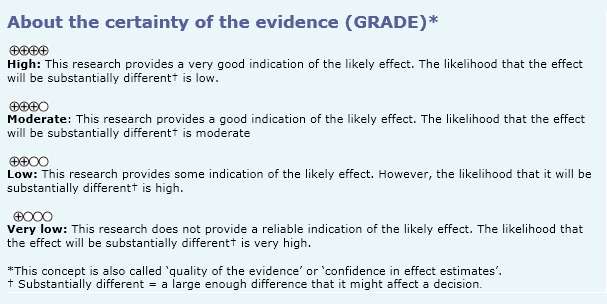
We used Epistemonikos database, which is maintained by screening multiple information sources, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found five systematic reviews [1],[2],[3],[4],[5] including six primary studies [6],[7],[8],[9],[10],[11], of which four [6],[7],[8],[9] correspond to randomized controlled trials.This table and the summary in general are based on the latter. |
|
What types of patients were included |
All trials [6],[7],[8],[9] included patients with epilepsy, however only one trial [9] specified the type of epilepsy (secondarily generalized). |
|
What types of interventions were included |
All trials [6],[7],[8],[9] compared oral cannabidiol in different doses and different periods against placebo. |
|
What types of outcomes |
The systematic reviews identified [1],[2],[3],[4],[5] grouped outcomes in the following way: |
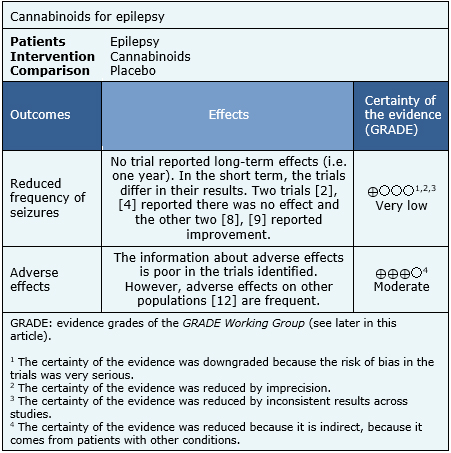
Summary of findings
The information about the effects of cannabinoids for control of epilepsy is based on four randomized trials including 48 patients [6],[7],[8],[9]. All of the trials reported both the frequency of seizures and adverse effects associated with its use, but none of the systematic reviews was able to conduct a meta-analysis with their data. The information on adverse effects was supplemented with a systematic review evaluating the adverse effects of cannabinoids in different populations, and includes 29 studies reporting this outcome [12]. The summary of findings is as follows:
- It is not clear whether cannabinoids reduce the frequency of seizures because the certainty of the evidence is very low.
- Cannabinoids are probably associated with transient but frequent adverse effects. The certainty of the evidence is moderate.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
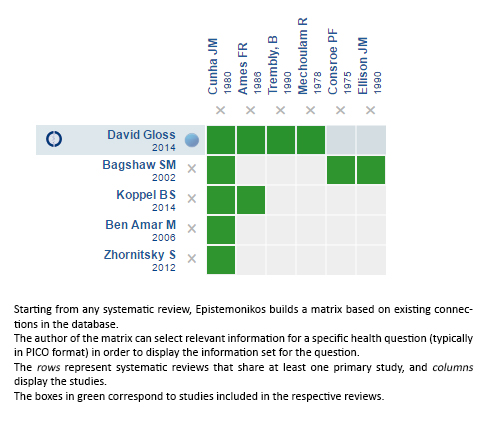
Siga el enlace para acceder a la versión interactiva: Cannabinoids for epilepsy
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

En el último tiempo se han descrito diversos beneficios con el uso de canabinoides en diferentes situaciones clínicas. Dentro de ellas se ha planteado un posible efecto en el control de la epilepsia, pero la real utilidad clínica es tema de debate. Utilizando la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en múltiples bases de datos, identificamos cinco revisiones sistemáticas que en conjunto incluyen cuatro estudios aleatorizados. Extrajimos los datos y realizamos una síntesis mediante tablas de resumen de los resultados utilizando el método GRADE. Concluimos que no está claro si los cannabinoides disminuyen la frecuencia de las convulsiones porque la certeza de la evidencia es muy baja, pero probablemente se asocian a efectos adversos frecuentes.
 Authors:
Javier Peña[1,2], Gabriel Rada[2,3,4,5,6]
Authors:
Javier Peña[1,2], Gabriel Rada[2,3,4,5,6]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Programa de Salud Basada en Evidencia, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[5] GRADE working group
[6] The Cochrane Collaboration
E-mail: radagabriel@epistemonikos.org
Author address:
[1] Facultad de Medicina Pontificia Universidad Católica de Chile Lira 63 Santiago Centro Chile

Citation: Peña J, Rada G. Are cannabinoids effective for epilepsy?. Medwave 2017; 17(Suppl1):e6821 doi: 10.5867/medwave.2017.6821
Publication date: 13/1/2017

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Gloss D, Vickrey B. Cannabinoids for epilepsy. Cochrane Database Syst Rev. 2014 Mar 5;(3):CD009270 | CrossRef | PubMed |
- Koppel BS, Brust JC, Fife T, Bronstein J, Youssof S, Gronseth G, et al. Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014 Apr 29;82(17):1556-63 | CrossRef | PubMed |
- Ben Amar M. Cannabinoids in medicine: A review of their therapeutic potential. J Ethnopharmacol. 2006 Apr 21;105(1-2):1-25 | PubMed |
- Bagshaw SM, Hagen NA. Medical efficacy of cannabinoids and marijuana: a comprehensive review of the literature. J Palliat Care. 2002 Summer;18(2):111-22 | PubMed |
- Zhornitsky S, Potvin S. Cannabidiol in humans-the quest for therapeutic targets. Pharmaceuticals (Basel). 2012 May 21;5(5):529-52 | CrossRef | PubMed |
- Trembly, B, Sherman, M. Double-blind clinical study of cannabidiol as a secondary anticonvulsant. Marijuana '90 International Conference on Cannabis and Cannabinoids. Kolympari, Crete. International Association for Cannabinoid Medicines. 1990;:Section 2, Pág. 5 | Link |
- Ames FR, Cridland S. Anticonvulsant effect of cannabidiol. S Afr Med J. 1986 Jan 4;69(1):14 | PubMed |
- Mechoulam R, Carlini EA. Toward drugs derived from cannabis. Naturwissenschaften. 1978 Apr;65(4):174-9 | PubMed |
- Cunha JM, Carlini EA, Pereira AE, Ramos OL, Pimentel C, Gagliardi R, et al. Chronic administration of cannabidiol to healthy volunteers and epileptic patients. Pharmacology. 1980;21(3):175-85 | PubMed |
- Consroe PF, Wood GC, Buchsbaum H. Anticonvulsant nature of marihuana smoking. JAMA. 1975 Oct 20;234(3):306-7 | PubMed |
- Ellison JM, Gelwan E, Ogletree J. Complex partial seizure symptoms affected by marijuana abuse. J Clin Psychiatry. 1990 Oct;51(10):439-40 | PubMed |
- Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, Keurentjes JC, Lang S, et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA. 2015 Jun 23-30;313(24):2456-73 | CrossRef | PubMed |
- AES Position on medical marijuana (Updated March 21, 2016.). Accedido el 15 de octubre 2016 | Link |
 Gloss D, Vickrey B. Cannabinoids for epilepsy. Cochrane Database Syst Rev. 2014 Mar 5;(3):CD009270 | CrossRef | PubMed |
Gloss D, Vickrey B. Cannabinoids for epilepsy. Cochrane Database Syst Rev. 2014 Mar 5;(3):CD009270 | CrossRef | PubMed | Koppel BS, Brust JC, Fife T, Bronstein J, Youssof S, Gronseth G, et al. Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014 Apr 29;82(17):1556-63 | CrossRef | PubMed |
Koppel BS, Brust JC, Fife T, Bronstein J, Youssof S, Gronseth G, et al. Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014 Apr 29;82(17):1556-63 | CrossRef | PubMed | Ben Amar M. Cannabinoids in medicine: A review of their therapeutic potential. J Ethnopharmacol. 2006 Apr 21;105(1-2):1-25 | PubMed |
Ben Amar M. Cannabinoids in medicine: A review of their therapeutic potential. J Ethnopharmacol. 2006 Apr 21;105(1-2):1-25 | PubMed | Bagshaw SM, Hagen NA. Medical efficacy of cannabinoids and marijuana: a comprehensive review of the literature. J Palliat Care. 2002 Summer;18(2):111-22 | PubMed |
Bagshaw SM, Hagen NA. Medical efficacy of cannabinoids and marijuana: a comprehensive review of the literature. J Palliat Care. 2002 Summer;18(2):111-22 | PubMed | Zhornitsky S, Potvin S. Cannabidiol in humans-the quest for therapeutic targets. Pharmaceuticals (Basel). 2012 May 21;5(5):529-52 | CrossRef | PubMed |
Zhornitsky S, Potvin S. Cannabidiol in humans-the quest for therapeutic targets. Pharmaceuticals (Basel). 2012 May 21;5(5):529-52 | CrossRef | PubMed | Trembly, B, Sherman, M. Double-blind clinical study of cannabidiol as a secondary anticonvulsant. Marijuana '90 International Conference on Cannabis and Cannabinoids. Kolympari, Crete. International Association for Cannabinoid Medicines. 1990;:Section 2, Pág. 5 | Link |
Trembly, B, Sherman, M. Double-blind clinical study of cannabidiol as a secondary anticonvulsant. Marijuana '90 International Conference on Cannabis and Cannabinoids. Kolympari, Crete. International Association for Cannabinoid Medicines. 1990;:Section 2, Pág. 5 | Link | Ames FR, Cridland S. Anticonvulsant effect of cannabidiol. S Afr Med J. 1986 Jan 4;69(1):14 | PubMed |
Ames FR, Cridland S. Anticonvulsant effect of cannabidiol. S Afr Med J. 1986 Jan 4;69(1):14 | PubMed | Mechoulam R, Carlini EA. Toward drugs derived from cannabis. Naturwissenschaften. 1978 Apr;65(4):174-9 | PubMed |
Mechoulam R, Carlini EA. Toward drugs derived from cannabis. Naturwissenschaften. 1978 Apr;65(4):174-9 | PubMed | Cunha JM, Carlini EA, Pereira AE, Ramos OL, Pimentel C, Gagliardi R, et al. Chronic administration of cannabidiol to healthy volunteers and epileptic patients. Pharmacology. 1980;21(3):175-85 | PubMed |
Cunha JM, Carlini EA, Pereira AE, Ramos OL, Pimentel C, Gagliardi R, et al. Chronic administration of cannabidiol to healthy volunteers and epileptic patients. Pharmacology. 1980;21(3):175-85 | PubMed | Consroe PF, Wood GC, Buchsbaum H. Anticonvulsant nature of marihuana smoking. JAMA. 1975 Oct 20;234(3):306-7 | PubMed |
Consroe PF, Wood GC, Buchsbaum H. Anticonvulsant nature of marihuana smoking. JAMA. 1975 Oct 20;234(3):306-7 | PubMed | Ellison JM, Gelwan E, Ogletree J. Complex partial seizure symptoms affected by marijuana abuse. J Clin Psychiatry. 1990 Oct;51(10):439-40 | PubMed |
Ellison JM, Gelwan E, Ogletree J. Complex partial seizure symptoms affected by marijuana abuse. J Clin Psychiatry. 1990 Oct;51(10):439-40 | PubMed | Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, Keurentjes JC, Lang S, et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA. 2015 Jun 23-30;313(24):2456-73 | CrossRef | PubMed |
Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, Keurentjes JC, Lang S, et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA. 2015 Jun 23-30;313(24):2456-73 | CrossRef | PubMed | AES Position on medical marijuana (Updated March 21, 2016.). Accedido el 15 de octubre 2016 | Link |
AES Position on medical marijuana (Updated March 21, 2016.). Accedido el 15 de octubre 2016 | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








