Resumen
El betabloqueo en pacientes sometidos a cirugía no cardíaca ha sido ampliamente recomendado como una forma de disminuir los eventos adversos cardiovasculares durante el periodo perioperatorio. Sin embargo, los estudios han mostrado resultados discordantes. Utilizando la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en múltiples bases de datos, identificamos 22 revisiones sistemáticas que en conjunto incluyen 131 estudios, entre ellos 112 estudios aleatorizados. Extrajimos los datos, realizamos un metanálisis y preparamos tablas de resumen de los resultados utilizando el método GRADE. Concluimos que el uso perioperatorio de betabloqueadores en pacientes sometidos a cirugía no cardíaca, si bien probablemente disminuye el riesgo de infarto miocárdico, aumenta el riesgo de accidente cerebrovascular y la mortalidad total.
Problema
El aumento de catecolaminas que ocurre durante una cirugía no cardiaca [1] produce una elevación de la presión arterial y de la frecuencia cardíaca [2],[3],[4] que contribuye a la ocurrencia de eventos adversos cardiovasculares. Los betabloqueadores suprimen el efecto de la elevación de catecolaminas, por lo que se piensa que su administración en el periodo perioperatorio podría prevenir estos eventos. Los estudios iniciales mostraron resultados muy prometedores, lo cual llevó a que esta intervención fuera ampliamente recomendada para un gran espectro de pacientes sometidos a cirugía no cardíaca. No obstante, estudios posteriores no sólo matizaron el posible beneficio de administrar betabloqueadores en el periodo perioperatorio, sino que alertaron sobre posibles efectos adversos como accidente cerebrovascular, hipotensión y bradicardia, entre otros. A lo anterior se suma el cuestionamiento sobre la confiabilidad de ciertos estudios en que se fundamentaron las recomendaciones previas, ya que algunos autores han sido acusados de mala conducta científica. Por todas estas razones la decisión sobre si utilizar o no esta intervención es motivo de debate hasta el día de hoy.
Métodos
Utilizamos la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en múltiples bases de datos, para identificar revisiones sistemáticas y sus estudios primarios incluidos. Con esta información generamos un resumen estructurado, siguiendo un formato preestablecido, que incluye mensajes clave, un resumen del conjunto de evidencia (presentado como matriz de evidencia en Epistemonikos), metanálisis del total de los estudios, tablas de resumen de resultados con el método GRADE, y tabla de otras consideraciones para la toma de decisión.
|
Mensajes clave
|
Acerca del conjunto de evidencia para esta pregunta
|
Cuál es la evidencia. |
Encontramos 22 revisiones sistemáticas[5],[6],[7],[8],[9], |
|
Qué tipo de pacientes incluyeron los estudios |
Los 55 estudios incluyeron pacientes adultos sometidos a cualquier tipo de cirugía no cardíaca: cirugía digestiva (22%), cirugía vascular (22%), ginecológica (14,6%), torácica (12,2%), traumatológica (7,3%), neurológica (7,3%), otorrinolaringológica (4,9%), maxilofacial (4,9%), oral (2,4%) y cirugía de emergencia (2,4%). |
|
Qué tipo de intervenciones incluyeron los estudios |
El tipo de betabloqueador más utilizado fue metoprolol (35,1%), luego esmolol (24,1%), atenolol (16,9%), labetalol (7,4%), bisoprolol (7,4%), propanolol (3,7%) y otros (landiolol, nadolol y timolol; 5,4%). |
|
Qué tipo de desenlaces midieron |
Las revisiones sistemáticas identificadas agruparon los desenlaces de la siguiente forma:
El seguimiento postoperatorio de los pacientes en los distintos estudios varió desde el día del alta hospitalaria, hasta 30 días posteriores a la cirugía. |
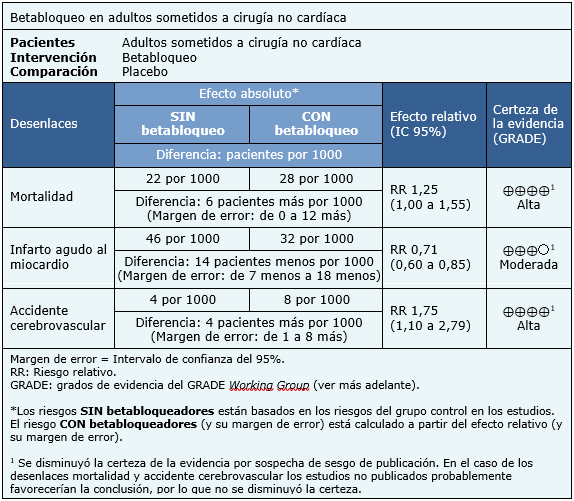
Resumen de los resultados
La información sobre el efecto de los betabloqueadores está basada en 29 estudios aleatorizados que incluyen 12 644 pacientes, cuyos datos pudieron ser incorporados a un metanálisis. Todos los estudios midieron el desenlace mortalidad por cualquier causa [27],[28],[29],[31],[32],[33],[34],[36],[37],[38],[39], [40],[41],[42],[45],[46],[47],[52],[54],[56],[58],[59],[60],[62],[72],[74],[75],[77],[78], 26 estudios midieron el desenlace infarto miocárdico perioperatorio [27],[28],[29],[31],[33],[34],[39],[40],[41],[42],[45],[46],[47],[52],[54],[56],[58],[59],[60],[62],[63],[72],[74],[75],[77],[78] y 16 midieron accidentes cerebrovasculares [27],[28],[29],[40],[41],[42],[47],[56],[58],[59],[62],[72],[74],[75],[77],[78]. El resumen de los resultados es el siguiente.
- El uso perioperatorio de betabloqueadores en pacientes sometidos a cirugía no cardíaca aumenta la mortalidad. La certeza de la evidencia es alta.
- El uso perioperatorio de betabloqueadores en pacientes sometidos a cirugía no cardíaca probablemente disminuye el riesgo de infarto miocárdico. La certeza de la evidencia es moderada.
- El uso perioperatorio de betabloqueadores en pacientes sometidos a cirugía no cardíaca aumenta el riesgo de accidente cerebrovascular. La certeza de la evidencia es alta.
Otras consideraciones para la toma de decisión
|
A quién se aplica y a quién no se aplica esta evidencia |
|
| Sobre los desenlaces incluidos en este resumen |
|
| Balance riesgo/beneficio y certeza de la evidencia |
|
| Qué piensan los pacientes y sus tratantes |
|
| Consideraciones de recursos |
|
| Diferencias entre este resumen y otras fuentes |
|
| ¿Puede que cambie esta información en el futuro? |
|
Cómo realizamos este resumen
Mediante métodos automatizados y colaborativos recopilamos toda la evidencia relevante para la pregunta de interés y la presentamos en una matriz de evidencia.
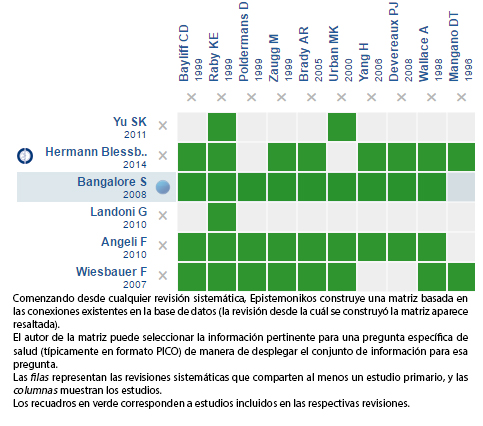
Siga el enlace para acceder a la versión interactiva: Betabloqueo perioperatorio en cirugía no cardíaca
Notas
Si con posterioridad a la publicación de este resumen se publican nuevas revisiones sistemáticas sobre este tema, en la parte superior de la matriz se mostrará un aviso de “nueva evidencia”. Si bien el proyecto contempla la actualización periódica de estos resúmenes, los usuarios están invitados a comentar en Medwave o contactar a los autores mediante correo electrónico si creen que hay evidencia que motive una actualización más rápida.
Luego de crear una cuenta en Epistemonikos, al guardar las matrices recibirá notificaciones automáticas cada vez que exista nueva evidencia que potencialmente responda a esta pregunta. El detalle de los métodos para elaborar este resumen están descritos aquí: http://dx.doi.org/10.5867/medwave.2014.06.5997.
La Fundación Epistemonikos es una organización que busca acercar la información a quienes toman decisiones en salud, mediante el uso de tecnologías. Su principal desarrollo es la base de datos Epistemonikos (www.epistemonikos.org).
Los resúmenes de evidencia siguen un riguroso proceso de revisión por pares interno.
Declaración de conflictos de intereses
Los autores declaran no tener conflictos de intereses con la materia de este artículo.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

El betabloqueo en pacientes sometidos a cirugía no cardíaca ha sido ampliamente recomendado como una forma de disminuir los eventos adversos cardiovasculares durante el periodo perioperatorio. Sin embargo, los estudios han mostrado resultados discordantes. Utilizando la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en múltiples bases de datos, identificamos 22 revisiones sistemáticas que en conjunto incluyen 131 estudios, entre ellos 112 estudios aleatorizados. Extrajimos los datos, realizamos un metanálisis y preparamos tablas de resumen de los resultados utilizando el método GRADE. Concluimos que el uso perioperatorio de betabloqueadores en pacientes sometidos a cirugía no cardíaca, si bien probablemente disminuye el riesgo de infarto miocárdico, aumenta el riesgo de accidente cerebrovascular y la mortalidad total.
 Authors:
Andrés Armstrong[1,2], Gabriel Rada[2,3,4,5,6], Fernando Altermatt[2,7]
Authors:
Andrés Armstrong[1,2], Gabriel Rada[2,3,4,5,6], Fernando Altermatt[2,7]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Programa de Salud Basada en Evidencia, Facultad de Medicina, Pontificia Universidad Católica de Chile
[4] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[5] GRADE working group
[6] The Cochrane Collaboration
[7] Departamento de Anestesiología, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
E-mail: fernando.altermatt@gmail.com
Author address:
[1] Facultad de Medicina Pontificia Universidad Católica de Chile Lira 63 Santiago Centro Chile

Citation: Armstrong A, Rada G, Altermatt F. Is perioperative beta-blockade effective and safe in patients undergoing non-cardiac surgery?. Medwave 2016; 16(Suppl5):e6819 doi: 10.5867/medwave.2016.6819
Publication date: 27/12/2016

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Sametz W, Metzler H, Gries M, Porta S, Sadjak A, Supanz S, et al. Perioperative catecholamine changes in cardiac risk patients. Eur J Clin Invest. 1999 Jul;29(7):582-7 | PubMed |
- Parker SD, Breslow MJ, Frank SM, Rosenfeld BA, Norris EJ, Christopherson R, et al. Catecholamine and cortisol responses to lower extremity revascularization: correlation with outcome variables. Perioperative Ischemia Randomized Anesthesia Trial Study Group. Crit Care Med. 1995 Dec;23(12):1954-61 | PubMed |
- Priebe HJ. Triggers of perioperative myocardial ischaemia and infarction. Br J Anaesth. 2004 Jul;93(1):9-20 | PubMed |
- Weissman C. The metabolic response to stress: an overview and update. Anesthesiology. 1990 Aug;73(2):308-27 | PubMed |
- Angeli F, Verdecchia P, Karthikeyan G, Mazzotta G, Gentile G, Reboldi G. ß-Blockers reduce mortality in patients undergoing high-risk non-cardiac surgery. Am J Cardiovasc Drugs. 2010;10(4):247-59 | CrossRef | PubMed |
- Angeli F, Verdecchia P, Karthikeyan G, Mazzotta G, Repaci S, del Pinto M, et al. Beta-blockers and risk of all-cause mortality in non-cardiac surgery. Ther Adv Cardiovasc Dis. 2010 Apr;4(2):109-18 | CrossRef | PubMed |
- Auerbach AD, Goldman L. beta-Blockers and reduction of cardiac events in noncardiac surgery: scientific review. JAMA. 2002 Mar 20;287(11):1435-44 | PubMed |
- Bangalore S, Wetterslev J, Pranesh S, Sawhney S, Gluud C, Messerli FH. Perioperative beta blockers in patients having non-cardiac surgery: a meta-analysis. Lancet. 2008 Dec 6;372(9654):1962-76 | CrossRef | PubMed |
- Bouri S, Shun-Shin MJ, Cole GD, Mayet J, Francis DP. Meta-analysis of secure randomised controlled trials of ß-blockade to prevent perioperative death in non-cardiac surgery. Heart. 2014 Mar;100(6):456-64 | CrossRef | PubMed |
- Dai N, Xu D, Zhang J, Wei Y, Li W, Fan B, et al. Different ß-blockers and initiation time in patients undergoing noncardiac surgery: a meta-analysis. Am J Med Sci. 2014 Mar;347(3):235-44 | CrossRef | PubMed |
- Devereaux PJ, Beattie WS, Choi PT, Badner NH, Guyatt GH, Villar JC, et al. How strong is the evidence for the use of perioperative beta blockers in non-cardiac surgery? Systematic review and meta-analysis of randomised controlled trials. BMJ. 2005 Aug 6;331(7512):313-21 | PubMed |
- Schouten O, Shaw LJ, Boersma E, Bax JJ, Kertai MD, Feringa HH, et al. A meta-analysis of safety and effectiveness of perioperative beta-blocker use for the prevention of cardiac events in different types of noncardiac surgery. Coron Artery Dis. 2006 Mar;17(2):173-9 | PubMed |
- Giles JW, Sear JW, Foëx P. Effect of chronic beta-blockade on peri-operative outcome in patients undergoing non-cardiac surgery: an analysis of observational and case control studies. Anaesthesia. 2004 Jun;59(6):574-83 | PubMed |
- Guay J, Ochroch EA. ß-blocking agents for surgery: influence on mortality and major outcomes. A meta-analysis. J Cardiothorac Vasc Anesth. 2013 Oct;27(5):834-44 | CrossRef | PubMed |
- Blessberger H, Kammler J, Domanovits H, Schlager O, Wildner B, Azar D, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity. Cochrane Database Syst Rev. 2014 Sep 18;(9):CD004476 | CrossRef | PubMed |
- Landoni G, Turi S, Biondi-Zoccai G, Bignami E, Testa V, Belloni I, et al. Esmolol reduces perioperative ischemia in noncardiac surgery: a meta-analysis of randomized controlled studies. J Cardiothorac Vasc Anesth. 2010 Apr;24(2):219-29 | CrossRef | PubMed |
- McGory ML, Maggard MA, Ko CY. A meta-analysis of perioperative beta blockade: what is the actual risk reduction? Surgery. 2005 Aug;138(2):171-9 | PubMed |
- Mostafaie K, Bedenis R, Harrington D. Beta-adrenergic blockers for perioperative cardiac risk reduction in people undergoing vascular surgery. Cochrane Database Syst Rev. 2015 Jan 14;1:CD006342 | CrossRef | PubMed |
- Riber LP, Larsen TB, Christensen TD. Postoperative atrial fibrillation prophylaxis after lung surgery: systematic review and meta-analysis. Ann Thorac Surg. 2014 Dec;98(6):1989-97 | CrossRef | PubMed |
- Sedrakyan A, Treasure T, Browne J, Krumholz H, Sharpin C, van der Meulen J. Pharmacologic prophylaxis for postoperative atrial tachyarrhythmia in general thoracic surgery: evidence from randomized clinical trials. J Thorac Cardiovasc Surg. 2005 May;129(5):997-1005 | PubMed |
- Stevens RD, Burri H, Tramèr MR. Pharmacologic myocardial protection in patients undergoing noncardiac surgery: a quantitative systematic review. Anesth Analg. 2003 Sep;97(3):623-33 | PubMed |
- Talati R, Reinhart KM, White CM, Phung OJ, Sedrakyan A, Kluger J, et al. Outcomes of perioperative beta-blockade in patients undergoing noncardiac surgery: a meta-analysis. Ann Pharmacother. 2009 Jul;43(7):1181-8 | CrossRef | PubMed |
- Wan YD, Zhang SG, Sun TW, Kan QC, Wang LX. The effects of perioperative ß-blockers on mortality in patients undergoing non-cardiac surgery in real world: a meta-analysis of cohort studies. Int J Cardiol. 2014 Oct 20;176(3):605-10 | CrossRef | PubMed |
- Wiesbauer F, Schlager O, Domanovits H, Wildner B, Maurer G, Muellner M, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity: a systematic review and meta-analysis. Anesth Analg. 2007 Jan;104(1):27-41 | PubMed |
- Wijeysundera DN, Duncan D, Nkonde-Price C, Virani SS, Washam JB, Fleischmann KE, et al. Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014 Dec 9;64(22):2406-25 | CrossRef | PubMed |
- Yu SK, Tait G, Karkouti K, Wijeysundera D, McCluskey S, Beattie WS. The safety of perioperative esmolol: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2011 Feb;112(2):267-81 | CrossRef | PubMed |
- Miller DR, Martineau RJ, Wynands JE, Hill J. Bolus administration of esmolol for controlling the haemodynamic response to tracheal intubation: the Canadian Multicentre Trial. Can J Anaesth. 1991 Oct;38(7):849-58 | PubMed |
- Lai RC, Xu MX, Huang WQ, Wang XD, Zeng WA, Lin WQ. [Beneficial effects of metoprolol on perioperative cardiac function of elderly esophageal cancer patients]. Ai Zheng. 2006 May;25(5):609-13 | PubMed |
- Wallace A, Layug B, Tateo I, Li J, Hollenberg M, Browner W, Miller D, Mangano DT. Prophylactic atenolol reduces postoperative myocardial ischemia. McSPI Research Group. Anesthesiology. 1998 Jan;88(1):7-17 | PubMed |
- Apipan B, Rummasak D. Efficacy and safety of oral propranolol premedication to reduce reflex tachycardia during hypotensive anesthesia with sodium nitroprusside in orthognathic surgery: a double-blind randomized clinical trial. J Oral Maxillofac Surg. 2010 Jan;68(1):120-4 | CrossRef | PubMed |
- Urban MK, Markowitz SM, Gordon MA, Urquhart BL, Kligfield P. Postoperative prophylactic administration of beta-adrenergic blockers in patients at risk for myocardial ischemia. Anesth Analg. 2000 Jun;90(6):1257-61 | PubMed |
- Magnusson J, Thulin T, Werner O, Järhult J, Thomson D. Haemodynamic effects of pretreatment with metoprolol in hypertensive patients undergoing surgery. Br J Anaesth. 1986 Mar;58(3):251-60 | PubMed |
- Magnusson H, Pontén J, Sonander HG. Methohexitone anaesthesia for microlaryngoscopy: circulatory modulation with metoprolol and dihydralazine. Br J Anaesth. 1986 Sep;58(9):976-82 | PubMed |
- Neary WD, McCrirrick A, Foy C, Heather BP, Earnshaw JJ. Lessons learned from a randomised controlled study of perioperative beta blockade in high risk patients undergoing emergency surgery. Surgeon. 2006 Jun;4(3):139-43 | PubMed |
- Jakobsen CJ, Bille S, Ahlburg P, Rybro L, Hjortholm K, Andresen EB. Perioperative metoprolol reduces the frequency of atrial fibrillation after thoracotomy for lung resection. J Cardiothorac Vasc Anesth. 1997 Oct;11(6):746-51 | PubMed |
- Kawaguchi M, Utada K, Yoshitani K, Uchino H, Takeda Y, Masui K, et al; Intraoperative Landiolol for Intracranial Aneurysm Surgery Trial (ILAST) Investigators. Effects of a short-acting [beta]1 receptor antagonist landiolol on hemodynamics and tissue injury markers in patients with subarachnoid hemorrhage undergoing intracranial aneurysm surgery. J Neurosurg Anesthesiol. 2010 Jul;22(3):230-9 | CrossRef | PubMed |
- Suttner S, Boldt J, Mengistu A, Lang K, Mayer J. Influence of continuous perioperative beta-blockade in combination with phosphodiesterase inhibition on haemodynamics and myocardial ischaemia in high-risk vascular surgery patients. Br J Anaesth. 2009 May;102(5):597-607 | CrossRef | PubMed |
- Burns JM, Hart DM, Hughes RL, Kelman AW, Hillis WS. Effects of nadolol on arrhythmias during laparoscopy performed under general anaesthesia. Br J Anaesth. 1988 Sep;61(3):345-6 | PubMed |
- Miller D, Martineau R, Hull K, Hill J. Bolus administration of esmolol for controlling the hemodynamic response to laryngoscopy and intubation: efficacy and effects on myocardial performance. J Cardiothorac Anesth 1990; 4: 31–36 | Link |
- Mangano DT, Layug EL, Wallace A, Tateo I. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. Multicenter Study of Perioperative Ischemia Research Group. N Engl J Med. 1996 Dec 5;335(23):1713-20. | PubMed |
- Cucchiara RF, Benefiel DJ, Matteo RS, DeWood M, Albin MS. Evaluation of esmolol in controlling increases in heart rate and blood pressure during endotracheal intubation in patients undergoing carotid endarterectomy. Anesthesiology. 1986 Nov;65(5):528-31 | PubMed |
- Jakobsen CJ, Grabe N, Christensen B. Metoprolol decreases the amount of halothane required to induce hypotension during general anaesthesia. Br J Anaesth. 1986 Mar;58(3):261-6 | PubMed |
- Jakobsen CJ, Blom L. Effect of pre-operative metoprolol on cardiovascular and catecholamine response and bleeding during hysterectomy. Eur J Anaesthesiol. 1992 May;9(3):209-15 | PubMed |
- Poldermans D, Boersma E, Bax JJ, Thomson IR, van de Ven LL, Blankensteijn JD, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. N Engl J Med. 1999 Dec 9;341(24):1789-94 | PubMed |
- Zaugg M, Tagliente T, Lucchinetti E, Jacobs E, Krol M, Bodian C, et al. Beneficial effects from beta-adrenergic blockade in elderly patients undergoing noncardiac surgery. Anesthesiology. 1999 Dec;91(6):1674-86. | PubMed |
- Davies MJ, Dysart RH, Silbert BS, Scott DA, Cook RJ. Prevention of tachycardia with atenolol pretreatment for carotid endarterectomy under cervical plexus blockade. Anaesth Intensive Care. 1992 May;20(2):161-4 | PubMed |
- Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC, et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008 May 31;371(9627):1839-47 | CrossRef | PubMed |
- Stone JG, Foëx P, Sear JW, Johnson LL, Khambatta HJ, Triner L. Risk of myocardial ischaemia during anaesthesia in treated and untreated hypertensive patients. Br J Anaesth. 1988 Dec;61(6):675-9 | PubMed |
- Leslie JB, Kalayjian RW, McLoughlin TM, Plachetka JR. Attenuation of the hemodynamic responses to endotracheal intubation with preinduction intravenous labetalol. J Clin Anesth. 1989;1(3):194-200 | PubMed |
- Inada E, Cullen DJ, Nemeskal AR, Teplick R. Effect of labetalol or lidocaine on the hemodynamic response to intubation: a controlled randomized double-blind study. J Clin Anesth. 1989;1(3):207-13 | PubMed |
- London MJ, Zaugg M, Schaub MC, Spahn DR. Perioperative beta-adrenergic receptor blockade: physiologic foundations and clinical controversies. Anesthesiology. 2004 Jan;100(1):170-5 | PubMed |
- Raby KE, Brull SJ, Timimi F, Akhtar S, Rosenbaum S, Naimi C, Whittemore AD. The effect of heart rate control on myocardial ischemia among high-risk patients after vascular surgery. Anesth Analg. 1999 Mar;88(3):477-82 | PubMed |
- Dunkelgrun M, Boersma E, Schouten O, Koopman-van Gemert AW, van Poorten F, Bax JJ, et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate-risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE-IV). Ann Surg. 2009 Jun;249(6):921-6 | CrossRef | PubMed |
- Stone JG, Foëx P, Sear JW, Johnson LL, Khambatta HJ, Triner L. Myocardial ischemia in untreated hypertensive patients: effect of a single small oral dose of a beta-adrenergic blocking agent. Anesthesiology. 1988 Apr;68(4):495-500 | PubMed |
- Yang H, Raymer K, Butler R, et al. Metoprolol after vascular surgery (MAVS). Can J Anaesth 2004;51: A7 | Link |
- Bayliff CD, Massel DR, Inculet RI, Malthaner RA, Quinton SD, Powell FS, et al. Propranolol for the prevention of postoperative arrhythmias in general thoracic surgery. Ann Thorac Surg. 1999 Jan;67(1):182-6 | PubMed |
- Oxorn D, Knox JW, Hill J. Bolus doses of esmolol for the prevention of perioperative hypertension and tachycardia. Can J Anaesth. 1990 Mar;37(2):206-9. | PubMed |
- Yang H, Raymer K, Butler R, Parlow J, Roberts R. The effects of perioperative beta-blockade: results of the Metoprolol after Vascular Surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006 Nov;152(5):983-90 | PubMed |
- Marwick TH, Branagan H, Venkatesh B, Stewart S; STRATIFY investigators. Use of a nurse-led intervention to optimize beta-blockade for reducing cardiac events after major noncardiac surgery. Am Heart J. 2009 Apr;157(4):784-90 | CrossRef | PubMed |
- Jakobsen CJ, Bille S, Ahlburg P, Rybro L, Pedersen KD, Rasmussen B. Preoperative metoprolol improves cardiovascular stability and reduces oxygen consumption after thoracotomy. Acta Anaesthesiol Scand. 1997 Nov;41(10):1324-30. | PubMed |
- Miller DR, Martineau RJ. Bolus administration of esmolol for the treatment of intraoperative myocardial ischaemia. Can J Anaesth. 1989 Sep;36(5):593-7 | PubMed |
- Brady AR, Gibbs JS, Greenhalgh RM, Powell JT, Sydes MR; POBBLE trial investigators.. Perioperative beta-blockade (POBBLE) for patients undergoing infrarenal vascular surgery: results of a randomized double-blind controlled trial. J Vasc Surg. 2005 Apr;41(4):602-9 | PubMed |
- Liu Y, Huang CL, He M, Zhang LN, Cai HW, Guo QL. [Influences of perioperative metoprolol on hemodynamics and myocardial ischaemia in elderly patients undergoing noncardiac surgery]. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2006 Apr;31(2):249-53 | PubMed |
- Mackenzie JW, Bird J. Timolol: a non-sedative anxiolytic premedicant for day cases. BMJ. 1989 Feb 11;298(6670):363-4 | PubMed |
- Whitehead MH, Whitmarsh VB, Horton JN. Metoprolol in anaesthesia for oral surgery. The effect of pretreatment on the incidence of cardiac dysrhythmias. Anaesthesia. 1980 Aug;35(8):779-82 | PubMed |
- Moon YE, Hwang WJ, Koh HJ, Min JY, Lee J. The sparing effect of low-dose esmolol on sevoflurane during laparoscopic gynaecological surgery. J Int Med Res. 2011;39(5):1861-9 | PubMed |
- Böhm M, Maack C, Wehrlen-Grandjean M, Erdmann E. Effect of bisoprolol on perioperative complications in chronic heart failure after surgery (Cardiac Insufficiency Bisoprolol Study II (CIBIS II)). Z Kardiol. 2003 Aug;92(8):668-76. | PubMed |
- Gibson BE, Black S, Maass L, Cucchiara RF. Esmolol for the control of hypertension after neurologic surgery. Clin Pharmacol Ther. 1988 Dec;44(6):650-3. | PubMed |
- Coleman AJ, Jordan C. Cardiovascular responses to anaesthesia. Influence of beta-adrenoreceptor blockade with metoprolol. Anaesthesia. 1980 Oct;35(10):972-8. | PubMed |
- Sandler AN, Leitch LF, Badner NH, et al. Esmolol compared with placebo in preventing increases in heart rate and blood pressure during rigid bronchoscopy. J Cardiothorac Anesth 1990; 4:44 –50 | Link |
- Lee SJ, Lee JN. The effect of perioperative esmolol infusion on the postoperative nausea, vomiting and pain after laparoscopic appendectomy. Korean J Anesthesiol. 2010 Sep;59(3):179-84 | CrossRef | PubMed |
- Yang XY, Wu XM, Wang S, Wang Q. [Effects of metoprolol on perioperative cardiovascular events in patients with risk or at high risk for coronary artery disease undergoing non-cardiac surgery]. Zhonghua Yi Xue Za Zhi. 2008 Jun 3;88(21):1476-80 | PubMed |
- Liu PL, Gatt S, Gugino LD, Mallampati SR, Covino BG. Esmolol for control of increases in heart rate and blood pressure during tracheal intubation after thiopentone and succinylcholine. Can Anaesth Soc J. 1986 Sep;33(5):556-62 | PubMed |
- Jakobsen CJ, Blom L, Brondbjerg M, Lenler-Petersen P. Effect of metoprolol and diazepam on pre-operative anxiety. Anaesthesia. 1990 Jan;45(1):40-3 | PubMed |
- Zaugg M, Bestmann L, Wacker J, Lucchinetti E, Boltres A, Schulz C, et al. Adrenergic receptor genotype but not perioperative bisoprolol therapy may determine cardiovascular outcome in at-risk patients undergoing surgery with spinal block: the Swiss Beta Blocker in Spinal Anesthesia (BBSA) study: a double-blinded, placebo-controlled, multicenter trial with 1-year follow-up. Anesthesiology. 2007 Jul;107(1):33-44 | PubMed |
- Gupta D, Srivastava S, Dubey RK, Prakash PS, Singh PK, Singh U. Comparative evaluation of atenolol and clonidine premedication on cardiovascular response to nasal speculum insertion during trans-sphenoid surgery for resection of pituitary adenoma: A prospective, randomised, double-blind, controlled study. Indian J Anaesth. 2011 Mar;55(2):135-40 | CrossRef | PubMed |
- Juul AB, Wetterslev J, Gluud C, Kofoed-Enevoldsen A, Jensen G, Callesen T, et al. Effect of perioperative beta blockade in patients with diabetes undergoing major non-cardiac surgery: randomised placebo controlled, blinded multicentre trial. BMJ. 2006 Jun 24;332(7556):1482 | PubMed |
- Rosenberg J, Overgaard H, Andersen M, Rasmussen V, Schulze S. Double blind randomised controlled trial of effect of metoprolol on myocardial ischaemia during endoscopic cholangiopancreatography. BMJ. 1996 Aug 3;313(7052):258-61 | PubMed |
- Juul AB, Wetterslev J, Kofoed-Enevoldsen A, Callesen T, Jensen G, Gluud C; Diabetic Postoperative Mortality and Morbidity group. The Diabetic Postoperative Mortality and Morbidity (DIPOM) trial: rationale and design of a multicenter, randomized, placebo-controlled, clinical trial of metoprolol for patients with diabetes mellitus who are undergoing major noncardiac surgery. Am Heart J. 2004 Apr;147(4):677-83 | PubMed |
- Shukla S, Gupta K, Gurha P, Sharma M, Sanjay RR, Shukla R, et al. Role of beta blockade in anaesthesia and postoperative pain management after major lower abdominal surgery. The Internet Journal of Anesthesiology 2010;25(1) | Link |
- Juul AB, Wetterslev J, Enevoldsen AK, et al. Randomized, blinded trial on perioperative metoprolol versus placebo for diabetic patients undergoing non-cardiac surgery. Circulation 2005; 111:1725 | Link |
- Erasmus MC Follow-up Investigation Committee. Investigation into Possible Violation of Scientific Integrity: Report Summary. November 16, 2011.
- Erasmus MC Follow-up Investigation Committee. Report on the 2012 Follow-Up Investigation of Possible Breaches of Academic Integrity. September 30, 2012.
 Sametz W, Metzler H, Gries M, Porta S, Sadjak A, Supanz S, et al. Perioperative catecholamine changes in cardiac risk patients. Eur J Clin Invest. 1999 Jul;29(7):582-7 | PubMed |
Sametz W, Metzler H, Gries M, Porta S, Sadjak A, Supanz S, et al. Perioperative catecholamine changes in cardiac risk patients. Eur J Clin Invest. 1999 Jul;29(7):582-7 | PubMed | Parker SD, Breslow MJ, Frank SM, Rosenfeld BA, Norris EJ, Christopherson R, et al. Catecholamine and cortisol responses to lower extremity revascularization: correlation with outcome variables. Perioperative Ischemia Randomized Anesthesia Trial Study Group. Crit Care Med. 1995 Dec;23(12):1954-61 | PubMed |
Parker SD, Breslow MJ, Frank SM, Rosenfeld BA, Norris EJ, Christopherson R, et al. Catecholamine and cortisol responses to lower extremity revascularization: correlation with outcome variables. Perioperative Ischemia Randomized Anesthesia Trial Study Group. Crit Care Med. 1995 Dec;23(12):1954-61 | PubMed | Priebe HJ. Triggers of perioperative myocardial ischaemia and infarction. Br J Anaesth. 2004 Jul;93(1):9-20 | PubMed |
Priebe HJ. Triggers of perioperative myocardial ischaemia and infarction. Br J Anaesth. 2004 Jul;93(1):9-20 | PubMed | Weissman C. The metabolic response to stress: an overview and update. Anesthesiology. 1990 Aug;73(2):308-27 | PubMed |
Weissman C. The metabolic response to stress: an overview and update. Anesthesiology. 1990 Aug;73(2):308-27 | PubMed | Angeli F, Verdecchia P, Karthikeyan G, Mazzotta G, Gentile G, Reboldi G. ß-Blockers reduce mortality in patients undergoing high-risk non-cardiac surgery. Am J Cardiovasc Drugs. 2010;10(4):247-59 | CrossRef | PubMed |
Angeli F, Verdecchia P, Karthikeyan G, Mazzotta G, Gentile G, Reboldi G. ß-Blockers reduce mortality in patients undergoing high-risk non-cardiac surgery. Am J Cardiovasc Drugs. 2010;10(4):247-59 | CrossRef | PubMed | Angeli F, Verdecchia P, Karthikeyan G, Mazzotta G, Repaci S, del Pinto M, et al. Beta-blockers and risk of all-cause mortality in non-cardiac surgery. Ther Adv Cardiovasc Dis. 2010 Apr;4(2):109-18 | CrossRef | PubMed |
Angeli F, Verdecchia P, Karthikeyan G, Mazzotta G, Repaci S, del Pinto M, et al. Beta-blockers and risk of all-cause mortality in non-cardiac surgery. Ther Adv Cardiovasc Dis. 2010 Apr;4(2):109-18 | CrossRef | PubMed | Auerbach AD, Goldman L. beta-Blockers and reduction of cardiac events in noncardiac surgery: scientific review. JAMA. 2002 Mar 20;287(11):1435-44 | PubMed |
Auerbach AD, Goldman L. beta-Blockers and reduction of cardiac events in noncardiac surgery: scientific review. JAMA. 2002 Mar 20;287(11):1435-44 | PubMed | Bangalore S, Wetterslev J, Pranesh S, Sawhney S, Gluud C, Messerli FH. Perioperative beta blockers in patients having non-cardiac surgery: a meta-analysis. Lancet. 2008 Dec 6;372(9654):1962-76 | CrossRef | PubMed |
Bangalore S, Wetterslev J, Pranesh S, Sawhney S, Gluud C, Messerli FH. Perioperative beta blockers in patients having non-cardiac surgery: a meta-analysis. Lancet. 2008 Dec 6;372(9654):1962-76 | CrossRef | PubMed | Bouri S, Shun-Shin MJ, Cole GD, Mayet J, Francis DP. Meta-analysis of secure randomised controlled trials of ß-blockade to prevent perioperative death in non-cardiac surgery. Heart. 2014 Mar;100(6):456-64 | CrossRef | PubMed |
Bouri S, Shun-Shin MJ, Cole GD, Mayet J, Francis DP. Meta-analysis of secure randomised controlled trials of ß-blockade to prevent perioperative death in non-cardiac surgery. Heart. 2014 Mar;100(6):456-64 | CrossRef | PubMed | Dai N, Xu D, Zhang J, Wei Y, Li W, Fan B, et al. Different ß-blockers and initiation time in patients undergoing noncardiac surgery: a meta-analysis. Am J Med Sci. 2014 Mar;347(3):235-44 | CrossRef | PubMed |
Dai N, Xu D, Zhang J, Wei Y, Li W, Fan B, et al. Different ß-blockers and initiation time in patients undergoing noncardiac surgery: a meta-analysis. Am J Med Sci. 2014 Mar;347(3):235-44 | CrossRef | PubMed | Devereaux PJ, Beattie WS, Choi PT, Badner NH, Guyatt GH, Villar JC, et al. How strong is the evidence for the use of perioperative beta blockers in non-cardiac surgery? Systematic review and meta-analysis of randomised controlled trials. BMJ. 2005 Aug 6;331(7512):313-21 | PubMed |
Devereaux PJ, Beattie WS, Choi PT, Badner NH, Guyatt GH, Villar JC, et al. How strong is the evidence for the use of perioperative beta blockers in non-cardiac surgery? Systematic review and meta-analysis of randomised controlled trials. BMJ. 2005 Aug 6;331(7512):313-21 | PubMed | Schouten O, Shaw LJ, Boersma E, Bax JJ, Kertai MD, Feringa HH, et al. A meta-analysis of safety and effectiveness of perioperative beta-blocker use for the prevention of cardiac events in different types of noncardiac surgery. Coron Artery Dis. 2006 Mar;17(2):173-9 | PubMed |
Schouten O, Shaw LJ, Boersma E, Bax JJ, Kertai MD, Feringa HH, et al. A meta-analysis of safety and effectiveness of perioperative beta-blocker use for the prevention of cardiac events in different types of noncardiac surgery. Coron Artery Dis. 2006 Mar;17(2):173-9 | PubMed | Giles JW, Sear JW, Foëx P. Effect of chronic beta-blockade on peri-operative outcome in patients undergoing non-cardiac surgery: an analysis of observational and case control studies. Anaesthesia. 2004 Jun;59(6):574-83 | PubMed |
Giles JW, Sear JW, Foëx P. Effect of chronic beta-blockade on peri-operative outcome in patients undergoing non-cardiac surgery: an analysis of observational and case control studies. Anaesthesia. 2004 Jun;59(6):574-83 | PubMed | Guay J, Ochroch EA. ß-blocking agents for surgery: influence on mortality and major outcomes. A meta-analysis. J Cardiothorac Vasc Anesth. 2013 Oct;27(5):834-44 | CrossRef | PubMed |
Guay J, Ochroch EA. ß-blocking agents for surgery: influence on mortality and major outcomes. A meta-analysis. J Cardiothorac Vasc Anesth. 2013 Oct;27(5):834-44 | CrossRef | PubMed | Blessberger H, Kammler J, Domanovits H, Schlager O, Wildner B, Azar D, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity. Cochrane Database Syst Rev. 2014 Sep 18;(9):CD004476 | CrossRef | PubMed |
Blessberger H, Kammler J, Domanovits H, Schlager O, Wildner B, Azar D, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity. Cochrane Database Syst Rev. 2014 Sep 18;(9):CD004476 | CrossRef | PubMed | Landoni G, Turi S, Biondi-Zoccai G, Bignami E, Testa V, Belloni I, et al. Esmolol reduces perioperative ischemia in noncardiac surgery: a meta-analysis of randomized controlled studies. J Cardiothorac Vasc Anesth. 2010 Apr;24(2):219-29 | CrossRef | PubMed |
Landoni G, Turi S, Biondi-Zoccai G, Bignami E, Testa V, Belloni I, et al. Esmolol reduces perioperative ischemia in noncardiac surgery: a meta-analysis of randomized controlled studies. J Cardiothorac Vasc Anesth. 2010 Apr;24(2):219-29 | CrossRef | PubMed | McGory ML, Maggard MA, Ko CY. A meta-analysis of perioperative beta blockade: what is the actual risk reduction? Surgery. 2005 Aug;138(2):171-9 | PubMed |
McGory ML, Maggard MA, Ko CY. A meta-analysis of perioperative beta blockade: what is the actual risk reduction? Surgery. 2005 Aug;138(2):171-9 | PubMed | Mostafaie K, Bedenis R, Harrington D. Beta-adrenergic blockers for perioperative cardiac risk reduction in people undergoing vascular surgery. Cochrane Database Syst Rev. 2015 Jan 14;1:CD006342 | CrossRef | PubMed |
Mostafaie K, Bedenis R, Harrington D. Beta-adrenergic blockers for perioperative cardiac risk reduction in people undergoing vascular surgery. Cochrane Database Syst Rev. 2015 Jan 14;1:CD006342 | CrossRef | PubMed | Riber LP, Larsen TB, Christensen TD. Postoperative atrial fibrillation prophylaxis after lung surgery: systematic review and meta-analysis. Ann Thorac Surg. 2014 Dec;98(6):1989-97 | CrossRef | PubMed |
Riber LP, Larsen TB, Christensen TD. Postoperative atrial fibrillation prophylaxis after lung surgery: systematic review and meta-analysis. Ann Thorac Surg. 2014 Dec;98(6):1989-97 | CrossRef | PubMed | Sedrakyan A, Treasure T, Browne J, Krumholz H, Sharpin C, van der Meulen J. Pharmacologic prophylaxis for postoperative atrial tachyarrhythmia in general thoracic surgery: evidence from randomized clinical trials. J Thorac Cardiovasc Surg. 2005 May;129(5):997-1005 | PubMed |
Sedrakyan A, Treasure T, Browne J, Krumholz H, Sharpin C, van der Meulen J. Pharmacologic prophylaxis for postoperative atrial tachyarrhythmia in general thoracic surgery: evidence from randomized clinical trials. J Thorac Cardiovasc Surg. 2005 May;129(5):997-1005 | PubMed | Stevens RD, Burri H, Tramèr MR. Pharmacologic myocardial protection in patients undergoing noncardiac surgery: a quantitative systematic review. Anesth Analg. 2003 Sep;97(3):623-33 | PubMed |
Stevens RD, Burri H, Tramèr MR. Pharmacologic myocardial protection in patients undergoing noncardiac surgery: a quantitative systematic review. Anesth Analg. 2003 Sep;97(3):623-33 | PubMed | Talati R, Reinhart KM, White CM, Phung OJ, Sedrakyan A, Kluger J, et al. Outcomes of perioperative beta-blockade in patients undergoing noncardiac surgery: a meta-analysis. Ann Pharmacother. 2009 Jul;43(7):1181-8 | CrossRef | PubMed |
Talati R, Reinhart KM, White CM, Phung OJ, Sedrakyan A, Kluger J, et al. Outcomes of perioperative beta-blockade in patients undergoing noncardiac surgery: a meta-analysis. Ann Pharmacother. 2009 Jul;43(7):1181-8 | CrossRef | PubMed | Wan YD, Zhang SG, Sun TW, Kan QC, Wang LX. The effects of perioperative ß-blockers on mortality in patients undergoing non-cardiac surgery in real world: a meta-analysis of cohort studies. Int J Cardiol. 2014 Oct 20;176(3):605-10 | CrossRef | PubMed |
Wan YD, Zhang SG, Sun TW, Kan QC, Wang LX. The effects of perioperative ß-blockers on mortality in patients undergoing non-cardiac surgery in real world: a meta-analysis of cohort studies. Int J Cardiol. 2014 Oct 20;176(3):605-10 | CrossRef | PubMed | Wiesbauer F, Schlager O, Domanovits H, Wildner B, Maurer G, Muellner M, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity: a systematic review and meta-analysis. Anesth Analg. 2007 Jan;104(1):27-41 | PubMed |
Wiesbauer F, Schlager O, Domanovits H, Wildner B, Maurer G, Muellner M, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity: a systematic review and meta-analysis. Anesth Analg. 2007 Jan;104(1):27-41 | PubMed | Wijeysundera DN, Duncan D, Nkonde-Price C, Virani SS, Washam JB, Fleischmann KE, et al. Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014 Dec 9;64(22):2406-25 | CrossRef | PubMed |
Wijeysundera DN, Duncan D, Nkonde-Price C, Virani SS, Washam JB, Fleischmann KE, et al. Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014 Dec 9;64(22):2406-25 | CrossRef | PubMed | Yu SK, Tait G, Karkouti K, Wijeysundera D, McCluskey S, Beattie WS. The safety of perioperative esmolol: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2011 Feb;112(2):267-81 | CrossRef | PubMed |
Yu SK, Tait G, Karkouti K, Wijeysundera D, McCluskey S, Beattie WS. The safety of perioperative esmolol: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2011 Feb;112(2):267-81 | CrossRef | PubMed | Miller DR, Martineau RJ, Wynands JE, Hill J. Bolus administration of esmolol for controlling the haemodynamic response to tracheal intubation: the Canadian Multicentre Trial. Can J Anaesth. 1991 Oct;38(7):849-58 | PubMed |
Miller DR, Martineau RJ, Wynands JE, Hill J. Bolus administration of esmolol for controlling the haemodynamic response to tracheal intubation: the Canadian Multicentre Trial. Can J Anaesth. 1991 Oct;38(7):849-58 | PubMed | Lai RC, Xu MX, Huang WQ, Wang XD, Zeng WA, Lin WQ. [Beneficial effects of metoprolol on perioperative cardiac function of elderly esophageal cancer patients]. Ai Zheng. 2006 May;25(5):609-13 | PubMed |
Lai RC, Xu MX, Huang WQ, Wang XD, Zeng WA, Lin WQ. [Beneficial effects of metoprolol on perioperative cardiac function of elderly esophageal cancer patients]. Ai Zheng. 2006 May;25(5):609-13 | PubMed | Wallace A, Layug B, Tateo I, Li J, Hollenberg M, Browner W, Miller D, Mangano DT. Prophylactic atenolol reduces postoperative myocardial ischemia. McSPI Research Group. Anesthesiology. 1998 Jan;88(1):7-17 | PubMed |
Wallace A, Layug B, Tateo I, Li J, Hollenberg M, Browner W, Miller D, Mangano DT. Prophylactic atenolol reduces postoperative myocardial ischemia. McSPI Research Group. Anesthesiology. 1998 Jan;88(1):7-17 | PubMed | Apipan B, Rummasak D. Efficacy and safety of oral propranolol premedication to reduce reflex tachycardia during hypotensive anesthesia with sodium nitroprusside in orthognathic surgery: a double-blind randomized clinical trial. J Oral Maxillofac Surg. 2010 Jan;68(1):120-4 | CrossRef | PubMed |
Apipan B, Rummasak D. Efficacy and safety of oral propranolol premedication to reduce reflex tachycardia during hypotensive anesthesia with sodium nitroprusside in orthognathic surgery: a double-blind randomized clinical trial. J Oral Maxillofac Surg. 2010 Jan;68(1):120-4 | CrossRef | PubMed | Urban MK, Markowitz SM, Gordon MA, Urquhart BL, Kligfield P. Postoperative prophylactic administration of beta-adrenergic blockers in patients at risk for myocardial ischemia. Anesth Analg. 2000 Jun;90(6):1257-61 | PubMed |
Urban MK, Markowitz SM, Gordon MA, Urquhart BL, Kligfield P. Postoperative prophylactic administration of beta-adrenergic blockers in patients at risk for myocardial ischemia. Anesth Analg. 2000 Jun;90(6):1257-61 | PubMed | Magnusson J, Thulin T, Werner O, Järhult J, Thomson D. Haemodynamic effects of pretreatment with metoprolol in hypertensive patients undergoing surgery. Br J Anaesth. 1986 Mar;58(3):251-60 | PubMed |
Magnusson J, Thulin T, Werner O, Järhult J, Thomson D. Haemodynamic effects of pretreatment with metoprolol in hypertensive patients undergoing surgery. Br J Anaesth. 1986 Mar;58(3):251-60 | PubMed | Magnusson H, Pontén J, Sonander HG. Methohexitone anaesthesia for microlaryngoscopy: circulatory modulation with metoprolol and dihydralazine. Br J Anaesth. 1986 Sep;58(9):976-82 | PubMed |
Magnusson H, Pontén J, Sonander HG. Methohexitone anaesthesia for microlaryngoscopy: circulatory modulation with metoprolol and dihydralazine. Br J Anaesth. 1986 Sep;58(9):976-82 | PubMed | Neary WD, McCrirrick A, Foy C, Heather BP, Earnshaw JJ. Lessons learned from a randomised controlled study of perioperative beta blockade in high risk patients undergoing emergency surgery. Surgeon. 2006 Jun;4(3):139-43 | PubMed |
Neary WD, McCrirrick A, Foy C, Heather BP, Earnshaw JJ. Lessons learned from a randomised controlled study of perioperative beta blockade in high risk patients undergoing emergency surgery. Surgeon. 2006 Jun;4(3):139-43 | PubMed | Jakobsen CJ, Bille S, Ahlburg P, Rybro L, Hjortholm K, Andresen EB. Perioperative metoprolol reduces the frequency of atrial fibrillation after thoracotomy for lung resection. J Cardiothorac Vasc Anesth. 1997 Oct;11(6):746-51 | PubMed |
Jakobsen CJ, Bille S, Ahlburg P, Rybro L, Hjortholm K, Andresen EB. Perioperative metoprolol reduces the frequency of atrial fibrillation after thoracotomy for lung resection. J Cardiothorac Vasc Anesth. 1997 Oct;11(6):746-51 | PubMed | Kawaguchi M, Utada K, Yoshitani K, Uchino H, Takeda Y, Masui K, et al; Intraoperative Landiolol for Intracranial Aneurysm Surgery Trial (ILAST) Investigators. Effects of a short-acting [beta]1 receptor antagonist landiolol on hemodynamics and tissue injury markers in patients with subarachnoid hemorrhage undergoing intracranial aneurysm surgery. J Neurosurg Anesthesiol. 2010 Jul;22(3):230-9 | CrossRef | PubMed |
Kawaguchi M, Utada K, Yoshitani K, Uchino H, Takeda Y, Masui K, et al; Intraoperative Landiolol for Intracranial Aneurysm Surgery Trial (ILAST) Investigators. Effects of a short-acting [beta]1 receptor antagonist landiolol on hemodynamics and tissue injury markers in patients with subarachnoid hemorrhage undergoing intracranial aneurysm surgery. J Neurosurg Anesthesiol. 2010 Jul;22(3):230-9 | CrossRef | PubMed | Suttner S, Boldt J, Mengistu A, Lang K, Mayer J. Influence of continuous perioperative beta-blockade in combination with phosphodiesterase inhibition on haemodynamics and myocardial ischaemia in high-risk vascular surgery patients. Br J Anaesth. 2009 May;102(5):597-607 | CrossRef | PubMed |
Suttner S, Boldt J, Mengistu A, Lang K, Mayer J. Influence of continuous perioperative beta-blockade in combination with phosphodiesterase inhibition on haemodynamics and myocardial ischaemia in high-risk vascular surgery patients. Br J Anaesth. 2009 May;102(5):597-607 | CrossRef | PubMed | Burns JM, Hart DM, Hughes RL, Kelman AW, Hillis WS. Effects of nadolol on arrhythmias during laparoscopy performed under general anaesthesia. Br J Anaesth. 1988 Sep;61(3):345-6 | PubMed |
Burns JM, Hart DM, Hughes RL, Kelman AW, Hillis WS. Effects of nadolol on arrhythmias during laparoscopy performed under general anaesthesia. Br J Anaesth. 1988 Sep;61(3):345-6 | PubMed | Miller D, Martineau R, Hull K, Hill J. Bolus administration of esmolol for controlling the hemodynamic response to laryngoscopy and intubation: efficacy and effects on myocardial performance. J Cardiothorac Anesth 1990; 4: 31–36 | Link |
Miller D, Martineau R, Hull K, Hill J. Bolus administration of esmolol for controlling the hemodynamic response to laryngoscopy and intubation: efficacy and effects on myocardial performance. J Cardiothorac Anesth 1990; 4: 31–36 | Link | Mangano DT, Layug EL, Wallace A, Tateo I. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. Multicenter Study of Perioperative Ischemia Research Group. N Engl J Med. 1996 Dec 5;335(23):1713-20. | PubMed |
Mangano DT, Layug EL, Wallace A, Tateo I. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. Multicenter Study of Perioperative Ischemia Research Group. N Engl J Med. 1996 Dec 5;335(23):1713-20. | PubMed | Cucchiara RF, Benefiel DJ, Matteo RS, DeWood M, Albin MS. Evaluation of esmolol in controlling increases in heart rate and blood pressure during endotracheal intubation in patients undergoing carotid endarterectomy. Anesthesiology. 1986 Nov;65(5):528-31 | PubMed |
Cucchiara RF, Benefiel DJ, Matteo RS, DeWood M, Albin MS. Evaluation of esmolol in controlling increases in heart rate and blood pressure during endotracheal intubation in patients undergoing carotid endarterectomy. Anesthesiology. 1986 Nov;65(5):528-31 | PubMed | Jakobsen CJ, Grabe N, Christensen B. Metoprolol decreases the amount of halothane required to induce hypotension during general anaesthesia. Br J Anaesth. 1986 Mar;58(3):261-6 | PubMed |
Jakobsen CJ, Grabe N, Christensen B. Metoprolol decreases the amount of halothane required to induce hypotension during general anaesthesia. Br J Anaesth. 1986 Mar;58(3):261-6 | PubMed | Jakobsen CJ, Blom L. Effect of pre-operative metoprolol on cardiovascular and catecholamine response and bleeding during hysterectomy. Eur J Anaesthesiol. 1992 May;9(3):209-15 | PubMed |
Jakobsen CJ, Blom L. Effect of pre-operative metoprolol on cardiovascular and catecholamine response and bleeding during hysterectomy. Eur J Anaesthesiol. 1992 May;9(3):209-15 | PubMed | Poldermans D, Boersma E, Bax JJ, Thomson IR, van de Ven LL, Blankensteijn JD, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. N Engl J Med. 1999 Dec 9;341(24):1789-94 | PubMed |
Poldermans D, Boersma E, Bax JJ, Thomson IR, van de Ven LL, Blankensteijn JD, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. N Engl J Med. 1999 Dec 9;341(24):1789-94 | PubMed | Zaugg M, Tagliente T, Lucchinetti E, Jacobs E, Krol M, Bodian C, et al. Beneficial effects from beta-adrenergic blockade in elderly patients undergoing noncardiac surgery. Anesthesiology. 1999 Dec;91(6):1674-86. | PubMed |
Zaugg M, Tagliente T, Lucchinetti E, Jacobs E, Krol M, Bodian C, et al. Beneficial effects from beta-adrenergic blockade in elderly patients undergoing noncardiac surgery. Anesthesiology. 1999 Dec;91(6):1674-86. | PubMed | Davies MJ, Dysart RH, Silbert BS, Scott DA, Cook RJ. Prevention of tachycardia with atenolol pretreatment for carotid endarterectomy under cervical plexus blockade. Anaesth Intensive Care. 1992 May;20(2):161-4 | PubMed |
Davies MJ, Dysart RH, Silbert BS, Scott DA, Cook RJ. Prevention of tachycardia with atenolol pretreatment for carotid endarterectomy under cervical plexus blockade. Anaesth Intensive Care. 1992 May;20(2):161-4 | PubMed | Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC, et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008 May 31;371(9627):1839-47 | CrossRef | PubMed |
Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC, et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008 May 31;371(9627):1839-47 | CrossRef | PubMed | Stone JG, Foëx P, Sear JW, Johnson LL, Khambatta HJ, Triner L. Risk of myocardial ischaemia during anaesthesia in treated and untreated hypertensive patients. Br J Anaesth. 1988 Dec;61(6):675-9 | PubMed |
Stone JG, Foëx P, Sear JW, Johnson LL, Khambatta HJ, Triner L. Risk of myocardial ischaemia during anaesthesia in treated and untreated hypertensive patients. Br J Anaesth. 1988 Dec;61(6):675-9 | PubMed | Leslie JB, Kalayjian RW, McLoughlin TM, Plachetka JR. Attenuation of the hemodynamic responses to endotracheal intubation with preinduction intravenous labetalol. J Clin Anesth. 1989;1(3):194-200 | PubMed |
Leslie JB, Kalayjian RW, McLoughlin TM, Plachetka JR. Attenuation of the hemodynamic responses to endotracheal intubation with preinduction intravenous labetalol. J Clin Anesth. 1989;1(3):194-200 | PubMed | Inada E, Cullen DJ, Nemeskal AR, Teplick R. Effect of labetalol or lidocaine on the hemodynamic response to intubation: a controlled randomized double-blind study. J Clin Anesth. 1989;1(3):207-13 | PubMed |
Inada E, Cullen DJ, Nemeskal AR, Teplick R. Effect of labetalol or lidocaine on the hemodynamic response to intubation: a controlled randomized double-blind study. J Clin Anesth. 1989;1(3):207-13 | PubMed | London MJ, Zaugg M, Schaub MC, Spahn DR. Perioperative beta-adrenergic receptor blockade: physiologic foundations and clinical controversies. Anesthesiology. 2004 Jan;100(1):170-5 | PubMed |
London MJ, Zaugg M, Schaub MC, Spahn DR. Perioperative beta-adrenergic receptor blockade: physiologic foundations and clinical controversies. Anesthesiology. 2004 Jan;100(1):170-5 | PubMed | Raby KE, Brull SJ, Timimi F, Akhtar S, Rosenbaum S, Naimi C, Whittemore AD. The effect of heart rate control on myocardial ischemia among high-risk patients after vascular surgery. Anesth Analg. 1999 Mar;88(3):477-82 | PubMed |
Raby KE, Brull SJ, Timimi F, Akhtar S, Rosenbaum S, Naimi C, Whittemore AD. The effect of heart rate control on myocardial ischemia among high-risk patients after vascular surgery. Anesth Analg. 1999 Mar;88(3):477-82 | PubMed | Dunkelgrun M, Boersma E, Schouten O, Koopman-van Gemert AW, van Poorten F, Bax JJ, et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate-risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE-IV). Ann Surg. 2009 Jun;249(6):921-6 | CrossRef | PubMed |
Dunkelgrun M, Boersma E, Schouten O, Koopman-van Gemert AW, van Poorten F, Bax JJ, et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate-risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE-IV). Ann Surg. 2009 Jun;249(6):921-6 | CrossRef | PubMed | Stone JG, Foëx P, Sear JW, Johnson LL, Khambatta HJ, Triner L. Myocardial ischemia in untreated hypertensive patients: effect of a single small oral dose of a beta-adrenergic blocking agent. Anesthesiology. 1988 Apr;68(4):495-500 | PubMed |
Stone JG, Foëx P, Sear JW, Johnson LL, Khambatta HJ, Triner L. Myocardial ischemia in untreated hypertensive patients: effect of a single small oral dose of a beta-adrenergic blocking agent. Anesthesiology. 1988 Apr;68(4):495-500 | PubMed | Yang H, Raymer K, Butler R, et al. Metoprolol after vascular surgery (MAVS). Can J Anaesth 2004;51: A7 | Link |
Yang H, Raymer K, Butler R, et al. Metoprolol after vascular surgery (MAVS). Can J Anaesth 2004;51: A7 | Link | Bayliff CD, Massel DR, Inculet RI, Malthaner RA, Quinton SD, Powell FS, et al. Propranolol for the prevention of postoperative arrhythmias in general thoracic surgery. Ann Thorac Surg. 1999 Jan;67(1):182-6 | PubMed |
Bayliff CD, Massel DR, Inculet RI, Malthaner RA, Quinton SD, Powell FS, et al. Propranolol for the prevention of postoperative arrhythmias in general thoracic surgery. Ann Thorac Surg. 1999 Jan;67(1):182-6 | PubMed | Oxorn D, Knox JW, Hill J. Bolus doses of esmolol for the prevention of perioperative hypertension and tachycardia. Can J Anaesth. 1990 Mar;37(2):206-9. | PubMed |
Oxorn D, Knox JW, Hill J. Bolus doses of esmolol for the prevention of perioperative hypertension and tachycardia. Can J Anaesth. 1990 Mar;37(2):206-9. | PubMed | Yang H, Raymer K, Butler R, Parlow J, Roberts R. The effects of perioperative beta-blockade: results of the Metoprolol after Vascular Surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006 Nov;152(5):983-90 | PubMed |
Yang H, Raymer K, Butler R, Parlow J, Roberts R. The effects of perioperative beta-blockade: results of the Metoprolol after Vascular Surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006 Nov;152(5):983-90 | PubMed | Marwick TH, Branagan H, Venkatesh B, Stewart S; STRATIFY investigators. Use of a nurse-led intervention to optimize beta-blockade for reducing cardiac events after major noncardiac surgery. Am Heart J. 2009 Apr;157(4):784-90 | CrossRef | PubMed |
Marwick TH, Branagan H, Venkatesh B, Stewart S; STRATIFY investigators. Use of a nurse-led intervention to optimize beta-blockade for reducing cardiac events after major noncardiac surgery. Am Heart J. 2009 Apr;157(4):784-90 | CrossRef | PubMed | Jakobsen CJ, Bille S, Ahlburg P, Rybro L, Pedersen KD, Rasmussen B. Preoperative metoprolol improves cardiovascular stability and reduces oxygen consumption after thoracotomy. Acta Anaesthesiol Scand. 1997 Nov;41(10):1324-30. | PubMed |
Jakobsen CJ, Bille S, Ahlburg P, Rybro L, Pedersen KD, Rasmussen B. Preoperative metoprolol improves cardiovascular stability and reduces oxygen consumption after thoracotomy. Acta Anaesthesiol Scand. 1997 Nov;41(10):1324-30. | PubMed | Miller DR, Martineau RJ. Bolus administration of esmolol for the treatment of intraoperative myocardial ischaemia. Can J Anaesth. 1989 Sep;36(5):593-7 | PubMed |
Miller DR, Martineau RJ. Bolus administration of esmolol for the treatment of intraoperative myocardial ischaemia. Can J Anaesth. 1989 Sep;36(5):593-7 | PubMed | Brady AR, Gibbs JS, Greenhalgh RM, Powell JT, Sydes MR; POBBLE trial investigators.. Perioperative beta-blockade (POBBLE) for patients undergoing infrarenal vascular surgery: results of a randomized double-blind controlled trial. J Vasc Surg. 2005 Apr;41(4):602-9 | PubMed |
Brady AR, Gibbs JS, Greenhalgh RM, Powell JT, Sydes MR; POBBLE trial investigators.. Perioperative beta-blockade (POBBLE) for patients undergoing infrarenal vascular surgery: results of a randomized double-blind controlled trial. J Vasc Surg. 2005 Apr;41(4):602-9 | PubMed | Liu Y, Huang CL, He M, Zhang LN, Cai HW, Guo QL. [Influences of perioperative metoprolol on hemodynamics and myocardial ischaemia in elderly patients undergoing noncardiac surgery]. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2006 Apr;31(2):249-53 | PubMed |
Liu Y, Huang CL, He M, Zhang LN, Cai HW, Guo QL. [Influences of perioperative metoprolol on hemodynamics and myocardial ischaemia in elderly patients undergoing noncardiac surgery]. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2006 Apr;31(2):249-53 | PubMed | Mackenzie JW, Bird J. Timolol: a non-sedative anxiolytic premedicant for day cases. BMJ. 1989 Feb 11;298(6670):363-4 | PubMed |
Mackenzie JW, Bird J. Timolol: a non-sedative anxiolytic premedicant for day cases. BMJ. 1989 Feb 11;298(6670):363-4 | PubMed | Whitehead MH, Whitmarsh VB, Horton JN. Metoprolol in anaesthesia for oral surgery. The effect of pretreatment on the incidence of cardiac dysrhythmias. Anaesthesia. 1980 Aug;35(8):779-82 | PubMed |
Whitehead MH, Whitmarsh VB, Horton JN. Metoprolol in anaesthesia for oral surgery. The effect of pretreatment on the incidence of cardiac dysrhythmias. Anaesthesia. 1980 Aug;35(8):779-82 | PubMed | Moon YE, Hwang WJ, Koh HJ, Min JY, Lee J. The sparing effect of low-dose esmolol on sevoflurane during laparoscopic gynaecological surgery. J Int Med Res. 2011;39(5):1861-9 | PubMed |
Moon YE, Hwang WJ, Koh HJ, Min JY, Lee J. The sparing effect of low-dose esmolol on sevoflurane during laparoscopic gynaecological surgery. J Int Med Res. 2011;39(5):1861-9 | PubMed | Böhm M, Maack C, Wehrlen-Grandjean M, Erdmann E. Effect of bisoprolol on perioperative complications in chronic heart failure after surgery (Cardiac Insufficiency Bisoprolol Study II (CIBIS II)). Z Kardiol. 2003 Aug;92(8):668-76. | PubMed |
Böhm M, Maack C, Wehrlen-Grandjean M, Erdmann E. Effect of bisoprolol on perioperative complications in chronic heart failure after surgery (Cardiac Insufficiency Bisoprolol Study II (CIBIS II)). Z Kardiol. 2003 Aug;92(8):668-76. | PubMed | Gibson BE, Black S, Maass L, Cucchiara RF. Esmolol for the control of hypertension after neurologic surgery. Clin Pharmacol Ther. 1988 Dec;44(6):650-3. | PubMed |
Gibson BE, Black S, Maass L, Cucchiara RF. Esmolol for the control of hypertension after neurologic surgery. Clin Pharmacol Ther. 1988 Dec;44(6):650-3. | PubMed | Coleman AJ, Jordan C. Cardiovascular responses to anaesthesia. Influence of beta-adrenoreceptor blockade with metoprolol. Anaesthesia. 1980 Oct;35(10):972-8. | PubMed |
Coleman AJ, Jordan C. Cardiovascular responses to anaesthesia. Influence of beta-adrenoreceptor blockade with metoprolol. Anaesthesia. 1980 Oct;35(10):972-8. | PubMed | Sandler AN, Leitch LF, Badner NH, et al. Esmolol compared with placebo in preventing increases in heart rate and blood pressure during rigid bronchoscopy. J Cardiothorac Anesth 1990; 4:44 –50 | Link |
Sandler AN, Leitch LF, Badner NH, et al. Esmolol compared with placebo in preventing increases in heart rate and blood pressure during rigid bronchoscopy. J Cardiothorac Anesth 1990; 4:44 –50 | Link | Lee SJ, Lee JN. The effect of perioperative esmolol infusion on the postoperative nausea, vomiting and pain after laparoscopic appendectomy. Korean J Anesthesiol. 2010 Sep;59(3):179-84 | CrossRef | PubMed |
Lee SJ, Lee JN. The effect of perioperative esmolol infusion on the postoperative nausea, vomiting and pain after laparoscopic appendectomy. Korean J Anesthesiol. 2010 Sep;59(3):179-84 | CrossRef | PubMed | Yang XY, Wu XM, Wang S, Wang Q. [Effects of metoprolol on perioperative cardiovascular events in patients with risk or at high risk for coronary artery disease undergoing non-cardiac surgery]. Zhonghua Yi Xue Za Zhi. 2008 Jun 3;88(21):1476-80 | PubMed |
Yang XY, Wu XM, Wang S, Wang Q. [Effects of metoprolol on perioperative cardiovascular events in patients with risk or at high risk for coronary artery disease undergoing non-cardiac surgery]. Zhonghua Yi Xue Za Zhi. 2008 Jun 3;88(21):1476-80 | PubMed | Liu PL, Gatt S, Gugino LD, Mallampati SR, Covino BG. Esmolol for control of increases in heart rate and blood pressure during tracheal intubation after thiopentone and succinylcholine. Can Anaesth Soc J. 1986 Sep;33(5):556-62 | PubMed |
Liu PL, Gatt S, Gugino LD, Mallampati SR, Covino BG. Esmolol for control of increases in heart rate and blood pressure during tracheal intubation after thiopentone and succinylcholine. Can Anaesth Soc J. 1986 Sep;33(5):556-62 | PubMed | Jakobsen CJ, Blom L, Brondbjerg M, Lenler-Petersen P. Effect of metoprolol and diazepam on pre-operative anxiety. Anaesthesia. 1990 Jan;45(1):40-3 | PubMed |
Jakobsen CJ, Blom L, Brondbjerg M, Lenler-Petersen P. Effect of metoprolol and diazepam on pre-operative anxiety. Anaesthesia. 1990 Jan;45(1):40-3 | PubMed | Zaugg M, Bestmann L, Wacker J, Lucchinetti E, Boltres A, Schulz C, et al. Adrenergic receptor genotype but not perioperative bisoprolol therapy may determine cardiovascular outcome in at-risk patients undergoing surgery with spinal block: the Swiss Beta Blocker in Spinal Anesthesia (BBSA) study: a double-blinded, placebo-controlled, multicenter trial with 1-year follow-up. Anesthesiology. 2007 Jul;107(1):33-44 | PubMed |
Zaugg M, Bestmann L, Wacker J, Lucchinetti E, Boltres A, Schulz C, et al. Adrenergic receptor genotype but not perioperative bisoprolol therapy may determine cardiovascular outcome in at-risk patients undergoing surgery with spinal block: the Swiss Beta Blocker in Spinal Anesthesia (BBSA) study: a double-blinded, placebo-controlled, multicenter trial with 1-year follow-up. Anesthesiology. 2007 Jul;107(1):33-44 | PubMed | Gupta D, Srivastava S, Dubey RK, Prakash PS, Singh PK, Singh U. Comparative evaluation of atenolol and clonidine premedication on cardiovascular response to nasal speculum insertion during trans-sphenoid surgery for resection of pituitary adenoma: A prospective, randomised, double-blind, controlled study. Indian J Anaesth. 2011 Mar;55(2):135-40 | CrossRef | PubMed |
Gupta D, Srivastava S, Dubey RK, Prakash PS, Singh PK, Singh U. Comparative evaluation of atenolol and clonidine premedication on cardiovascular response to nasal speculum insertion during trans-sphenoid surgery for resection of pituitary adenoma: A prospective, randomised, double-blind, controlled study. Indian J Anaesth. 2011 Mar;55(2):135-40 | CrossRef | PubMed | Juul AB, Wetterslev J, Gluud C, Kofoed-Enevoldsen A, Jensen G, Callesen T, et al. Effect of perioperative beta blockade in patients with diabetes undergoing major non-cardiac surgery: randomised placebo controlled, blinded multicentre trial. BMJ. 2006 Jun 24;332(7556):1482 | PubMed |
Juul AB, Wetterslev J, Gluud C, Kofoed-Enevoldsen A, Jensen G, Callesen T, et al. Effect of perioperative beta blockade in patients with diabetes undergoing major non-cardiac surgery: randomised placebo controlled, blinded multicentre trial. BMJ. 2006 Jun 24;332(7556):1482 | PubMed | Rosenberg J, Overgaard H, Andersen M, Rasmussen V, Schulze S. Double blind randomised controlled trial of effect of metoprolol on myocardial ischaemia during endoscopic cholangiopancreatography. BMJ. 1996 Aug 3;313(7052):258-61 | PubMed |
Rosenberg J, Overgaard H, Andersen M, Rasmussen V, Schulze S. Double blind randomised controlled trial of effect of metoprolol on myocardial ischaemia during endoscopic cholangiopancreatography. BMJ. 1996 Aug 3;313(7052):258-61 | PubMed | Juul AB, Wetterslev J, Kofoed-Enevoldsen A, Callesen T, Jensen G, Gluud C; Diabetic Postoperative Mortality and Morbidity group. The Diabetic Postoperative Mortality and Morbidity (DIPOM) trial: rationale and design of a multicenter, randomized, placebo-controlled, clinical trial of metoprolol for patients with diabetes mellitus who are undergoing major noncardiac surgery. Am Heart J. 2004 Apr;147(4):677-83 | PubMed |
Juul AB, Wetterslev J, Kofoed-Enevoldsen A, Callesen T, Jensen G, Gluud C; Diabetic Postoperative Mortality and Morbidity group. The Diabetic Postoperative Mortality and Morbidity (DIPOM) trial: rationale and design of a multicenter, randomized, placebo-controlled, clinical trial of metoprolol for patients with diabetes mellitus who are undergoing major noncardiac surgery. Am Heart J. 2004 Apr;147(4):677-83 | PubMed | Shukla S, Gupta K, Gurha P, Sharma M, Sanjay RR, Shukla R, et al. Role of beta blockade in anaesthesia and postoperative pain management after major lower abdominal surgery. The Internet Journal of Anesthesiology 2010;25(1) | Link |
Shukla S, Gupta K, Gurha P, Sharma M, Sanjay RR, Shukla R, et al. Role of beta blockade in anaesthesia and postoperative pain management after major lower abdominal surgery. The Internet Journal of Anesthesiology 2010;25(1) | Link | Juul AB, Wetterslev J, Enevoldsen AK, et al. Randomized, blinded trial on perioperative metoprolol versus placebo for diabetic patients undergoing non-cardiac surgery. Circulation 2005; 111:1725 | Link |
Juul AB, Wetterslev J, Enevoldsen AK, et al. Randomized, blinded trial on perioperative metoprolol versus placebo for diabetic patients undergoing non-cardiac surgery. Circulation 2005; 111:1725 | Link | Erasmus MC Follow-up Investigation Committee. Investigation into Possible Violation of Scientific Integrity: Report Summary. November 16, 2011.
Erasmus MC Follow-up Investigation Committee. Investigation into Possible Violation of Scientific Integrity: Report Summary. November 16, 2011.  Erasmus MC Follow-up Investigation Committee. Report on the 2012 Follow-Up Investigation of Possible Breaches of Academic Integrity. September 30, 2012.
Erasmus MC Follow-up Investigation Committee. Report on the 2012 Follow-Up Investigation of Possible Breaches of Academic Integrity. September 30, 2012. Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








