Abstract
Fluid restriction is usually recommended in chronic heart failure. However, the evidence base to support this is not that clear. Searching in Epistemonikos database, which is maintained by screening multiple databases, we identified five systematic reviews evaluating 11 studies addressing the question of this article, including seven randomized trials. We extracted data, combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded fluid restriction probably decreases hospital readmission in chronic heart failure and might decrease mortality, but the certainty of the evidence for the latter is low.
Problem
Chronic heart failure is a morbidity that impairs quality of life, requires frequent hospitalization and increases mortality. Many symptoms of heart failure are a consequence of sodium and fluid overload, so it is usually recommended to restrict fluid intake as a way to compensate volume overload. However, this measure might also have negative consequences, such as thirst, orthostatic hypotension and renal failure. It is not clear whether this recommendation is supported by scientific evidence.
Methods
We used Epistemonikos database, which is maintained by screening multiple databases, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found five systematic reviews [1],[2],[3],[4],[5] including 11 primary studies relevant to the question of this article, reported in 12 references [6],[7],[8],[9],[10],[11],[12],[13],[14],[15], [16],[17], among them seven randomized trials reported in eight references [6],[7],[8],[9],[10],[11],[12],[13]. Two trials evaluated patients with acute heart failure, so they were not considered relevant to the question addressed in this summary [8],[10].This table and the summary in general are based on the five randomized trials evaluating patients with chronic heart failure [6],[7],[9],[11],[12]. |
|
What types of patients were included |
Four trials evaluated patients with compensated heart failure [6],[7],[9],[12] and one included decompensated patients [11]. |
|
What types of interventions were included |
In two trials, fluid restriction was 1 litre per day [9],[11] and in three was 1.5 litres per day [6],[7],[12]. |
|
What types of outcomes |
The different reviews grouped outcomes as follows:
|
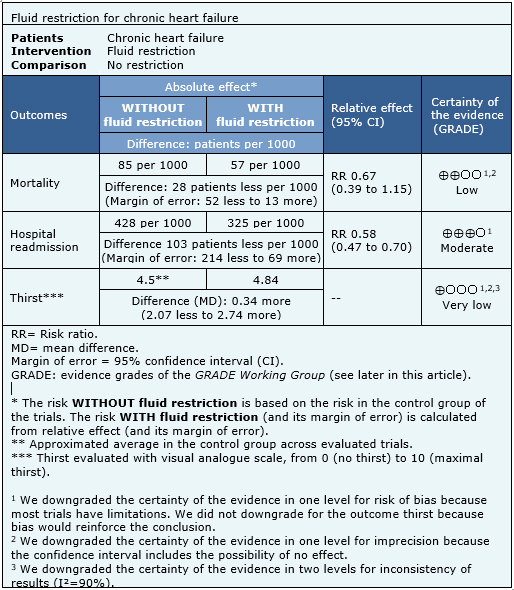
Summary of findings
The information on the effects of fluid restriction for chronic heart failure is based on four randomized trials including 678 participants, because one trial did not report any outcome of interest, or did not present it in a way it could be incorporated in a meta-analysis [12]. Four trials reported the outcomes mortality and hospital readmission [6],[7],[9],[11] and three reported thirst [6],[7],[9].
The summary of findings is the following:
- Fluid restriction might decrease mortality in chronic heart failure, but the certainty of the evidence is low.
- Fluid restriction probably decreases hospital readmission in chronic heart failure. The certainty of the evidence is moderate.
- It is not clear whether fluid restriction increases thirst because the certainty of the evidence is very low.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
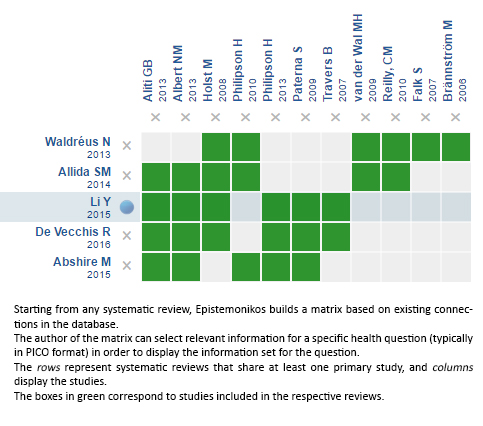
Follow the link to access the interactive version: Fluid restriction for chronic heart failure
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Habitualmente se recomienda la restricción de volumen en la insuficiencia cardíaca. Sin embargo, esto no necesariamente está sustentado por evidencia científica. Utilizando la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en múltiples bases de datos, identificamos cinco revisiones sistemáticas que en conjunto incluyen once estudios pertinentes a la pregunta, de los cuales siete corresponden a estudios controlados aleatorizados. Realizamos un metanálisis y tablas de resumen de los resultados utilizando el método GRADE. Concluimos que la restricción de volumen en la insuficiencia cardíaca probablemente disminuye la readmisión hospitalaria y podría disminuir la mortalidad, aunque la certeza de la evidencia para esto último es baja.
 Authors:
Victoria Castro-Gutiérrez[1,2], Gabriel Rada[2,3,4,5,6]
Authors:
Victoria Castro-Gutiérrez[1,2], Gabriel Rada[2,3,4,5,6]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Programa de Salud Basada en Evidencia, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[5] GRADE working group
[6] The Cochrane Collaboration
E-mail: radagabriel@epistemonikos.org
Author address:
[1] Facultad de Medicina Pontificia Universidad Católica de Chile Lira 63 Santiago Centro Chile

Citation: Castro-Gutiérrez V, Rada G. Is fluid restriction beneficial in chronic heart failure?. Medwave 2017;17(Suppl1):e6817 doi: 10.5867/medwave.2017.6817
Publication date: 9/1/2017

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Li Y, Fu B, Qian X. Liberal versus restricted fluid administration in heart failure patients. A systematic review and meta-analysis of randomized trials. Int Heart J. 2015;56(2):192-5 | CrossRef | PubMed |
- Abshire M, Xu J, Baptiste D, Almansa JR, Xu J, Cummings A, et al. Nutritional Interventions in Heart Failure: A Systematic Review of the Literature. J Card Fail. 2015 Dec;21(12):989-99 | CrossRef | PubMed |
- De Vecchis R, Baldi C, Cioppa C, Giasi A, Fusco A. Effects of limiting fluid intake on clinical and laboratory outcomes in patients with heart failure. Results of a meta-analysis of randomized controlled trials. Herz. 2016 Feb;41(1):63-75 | CrossRef | PubMed |
- Waldréus N, Hahn RG, Jaarsma T. Thirst in heart failure: a systematic literature review. Eur J Heart Fail. 2013 Feb;15(2):141-9 | CrossRef | PubMed |
- Allida SM, Inglis SC, Davidson PM, Lal S, Hayward CS, Newton PJ. Thirst in chronic heart failure: a review. J Clin Nurs. 2015 Apr;24(7-8):916-26 | CrossRef | PubMed |
- Philipson H, Ekman I, Forslund HB, Swedberg K, Schaufelberger M. Salt and fluid restriction is effective in patients with chronic heart failure. Eur J Heart Fail. 2013 Nov;15(11):1304-10 | CrossRef | PubMed |
- Holst M, Strömberg A, Lindholm M, Willenheimer R. Liberal versus restricted fluid prescription in stabilised patients with chronic heart failure: result of a randomised cross-over study of the effects on health-related quality of life, physical capacity, thirst and morbidity. Scand Cardiovasc J. 2008 Oct;42(5):316-22 | CrossRef | PubMed |
- Aliti GB, Rabelo ER, Clausell N, Rohde LE, Biolo A, Beck-da-Silva L. Aggressive fluid and sodium restriction in acute decompensated heart failure: a randomized clinical trial. JAMA Intern Med. 2013 Jun 24;173(12):1058-64 | CrossRef | PubMed |
- Albert NM, Nutter B, Forney J, Slifcak E, Tang WH. A randomized controlled pilot study of outcomes of strict allowance of fluid therapy in hyponatremic heart failure (SALT-HF). J Card Fail. 2013 Jan;19(1):1-9 | CrossRef | PubMed |
- Travers B, O'Loughlin C, Murphy NF, Ryder M, Conlon C, Ledwidge M, et al. Fluid restriction in the management of decompensated heart failure: no impact on time to clinical stability. J Card Fail. 2007 Mar;13(2):128-32 | PubMed |
- Paterna S, Parrinello G, Cannizzaro S, Fasullo S, Torres D, Sarullo FM, et al. Medium term effects of different dosage of diuretic, sodium, and fluid administration on neurohormonal and clinical outcome in patients with recently compensated heart failure. Am J Cardiol. 2009 Jan 1;103(1):93-102 | CrossRef | PubMed |
- Philipson H, Ekman I, Swedberg K, Schaufelberger M. A pilot study of salt and water restriction in patients with chronic heart failure. Scand Cardiovasc J. 2010 Aug;44(4):209-14 | CrossRef | PubMed |
- Holst M, Strömberg A, Lindholm M, Willenheimer R. Description of self-reported fluid intake and its effects on body weight, symptoms, quality of life and physical capacity in patients with stable chronic heart failure. J Clin Nurs. 2008 Sep;17(17):2318-26 | CrossRef | PubMed |
- Falk S, Wahn AK, Lidell E. Keeping the maintenance of daily life in spite of chronic heart failure. A qualitative study. Eur J Cardiovasc Nurs. 2007 Sep;6(3):192-9 | PubMed |
- Brännström M, Ekman I, Norberg A, Boman K, Strandberg G. Living with severe chronic heart failure in palliative advanced home care. Eur J Cardiovasc Nurs. 2006 Dec;5(4):295-302 | PubMed |
- van der Wal MH, Jaarsma T, Moser DK, van Gilst WH, van Veldhuisen DJ. Qualitative examination of compliance in heart failure patients in The Netherlands. Heart Lung. 2010 Mar-Apr;39(2):121-30 | CrossRef | PubMed |
- Reilly CM, Meadows K, Dunbar S, Culler S, Smith A. Thirst and QOL in persons with heart failure. Heart & Lung: The Journal of Acute and Critical Care. 2010;39(4):353 | CrossRef |
- McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al; ESC Committee for Practice Guidelines. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847 | CrossRef | PubMed |
- Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194 | CrossRef | PubMed |
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327 | CrossRef | PubMed |
- Finn Gustafsson. The Effect of Fluid Restriction in Congestive Heart Failure Complicated With Hyponatremia. NCT01748331 | Link |
- Simon Stewart. The which heart failure intervention is most cost-effective in reducing hospital stay trial. ACTRN12613000921785 | Link |
- Abshire M, Xu J, Baptiste D, Almansa JR, Xu J, Cummings A, et al. Nutritional Interventions in Heart Failure: A Systematic Review of the Literature. J Card Fail. 2015 Dec;21(12):989-99 | CrossRef | PubMed |
 Li Y, Fu B, Qian X. Liberal versus restricted fluid administration in heart failure patients. A systematic review and meta-analysis of randomized trials. Int Heart J. 2015;56(2):192-5 | CrossRef | PubMed |
Li Y, Fu B, Qian X. Liberal versus restricted fluid administration in heart failure patients. A systematic review and meta-analysis of randomized trials. Int Heart J. 2015;56(2):192-5 | CrossRef | PubMed | Abshire M, Xu J, Baptiste D, Almansa JR, Xu J, Cummings A, et al. Nutritional Interventions in Heart Failure: A Systematic Review of the Literature. J Card Fail. 2015 Dec;21(12):989-99 | CrossRef | PubMed |
Abshire M, Xu J, Baptiste D, Almansa JR, Xu J, Cummings A, et al. Nutritional Interventions in Heart Failure: A Systematic Review of the Literature. J Card Fail. 2015 Dec;21(12):989-99 | CrossRef | PubMed | De Vecchis R, Baldi C, Cioppa C, Giasi A, Fusco A. Effects of limiting fluid intake on clinical and laboratory outcomes in patients with heart failure. Results of a meta-analysis of randomized controlled trials. Herz. 2016 Feb;41(1):63-75 | CrossRef | PubMed |
De Vecchis R, Baldi C, Cioppa C, Giasi A, Fusco A. Effects of limiting fluid intake on clinical and laboratory outcomes in patients with heart failure. Results of a meta-analysis of randomized controlled trials. Herz. 2016 Feb;41(1):63-75 | CrossRef | PubMed | Waldréus N, Hahn RG, Jaarsma T. Thirst in heart failure: a systematic literature review. Eur J Heart Fail. 2013 Feb;15(2):141-9 | CrossRef | PubMed |
Waldréus N, Hahn RG, Jaarsma T. Thirst in heart failure: a systematic literature review. Eur J Heart Fail. 2013 Feb;15(2):141-9 | CrossRef | PubMed | Allida SM, Inglis SC, Davidson PM, Lal S, Hayward CS, Newton PJ. Thirst in chronic heart failure: a review. J Clin Nurs. 2015 Apr;24(7-8):916-26 | CrossRef | PubMed |
Allida SM, Inglis SC, Davidson PM, Lal S, Hayward CS, Newton PJ. Thirst in chronic heart failure: a review. J Clin Nurs. 2015 Apr;24(7-8):916-26 | CrossRef | PubMed | Philipson H, Ekman I, Forslund HB, Swedberg K, Schaufelberger M. Salt and fluid restriction is effective in patients with chronic heart failure. Eur J Heart Fail. 2013 Nov;15(11):1304-10 | CrossRef | PubMed |
Philipson H, Ekman I, Forslund HB, Swedberg K, Schaufelberger M. Salt and fluid restriction is effective in patients with chronic heart failure. Eur J Heart Fail. 2013 Nov;15(11):1304-10 | CrossRef | PubMed | Holst M, Strömberg A, Lindholm M, Willenheimer R. Liberal versus restricted fluid prescription in stabilised patients with chronic heart failure: result of a randomised cross-over study of the effects on health-related quality of life, physical capacity, thirst and morbidity. Scand Cardiovasc J. 2008 Oct;42(5):316-22 | CrossRef | PubMed |
Holst M, Strömberg A, Lindholm M, Willenheimer R. Liberal versus restricted fluid prescription in stabilised patients with chronic heart failure: result of a randomised cross-over study of the effects on health-related quality of life, physical capacity, thirst and morbidity. Scand Cardiovasc J. 2008 Oct;42(5):316-22 | CrossRef | PubMed | Aliti GB, Rabelo ER, Clausell N, Rohde LE, Biolo A, Beck-da-Silva L. Aggressive fluid and sodium restriction in acute decompensated heart failure: a randomized clinical trial. JAMA Intern Med. 2013 Jun 24;173(12):1058-64 | CrossRef | PubMed |
Aliti GB, Rabelo ER, Clausell N, Rohde LE, Biolo A, Beck-da-Silva L. Aggressive fluid and sodium restriction in acute decompensated heart failure: a randomized clinical trial. JAMA Intern Med. 2013 Jun 24;173(12):1058-64 | CrossRef | PubMed | Albert NM, Nutter B, Forney J, Slifcak E, Tang WH. A randomized controlled pilot study of outcomes of strict allowance of fluid therapy in hyponatremic heart failure (SALT-HF). J Card Fail. 2013 Jan;19(1):1-9 | CrossRef | PubMed |
Albert NM, Nutter B, Forney J, Slifcak E, Tang WH. A randomized controlled pilot study of outcomes of strict allowance of fluid therapy in hyponatremic heart failure (SALT-HF). J Card Fail. 2013 Jan;19(1):1-9 | CrossRef | PubMed | Travers B, O'Loughlin C, Murphy NF, Ryder M, Conlon C, Ledwidge M, et al. Fluid restriction in the management of decompensated heart failure: no impact on time to clinical stability. J Card Fail. 2007 Mar;13(2):128-32 | PubMed |
Travers B, O'Loughlin C, Murphy NF, Ryder M, Conlon C, Ledwidge M, et al. Fluid restriction in the management of decompensated heart failure: no impact on time to clinical stability. J Card Fail. 2007 Mar;13(2):128-32 | PubMed | Paterna S, Parrinello G, Cannizzaro S, Fasullo S, Torres D, Sarullo FM, et al. Medium term effects of different dosage of diuretic, sodium, and fluid administration on neurohormonal and clinical outcome in patients with recently compensated heart failure. Am J Cardiol. 2009 Jan 1;103(1):93-102 | CrossRef | PubMed |
Paterna S, Parrinello G, Cannizzaro S, Fasullo S, Torres D, Sarullo FM, et al. Medium term effects of different dosage of diuretic, sodium, and fluid administration on neurohormonal and clinical outcome in patients with recently compensated heart failure. Am J Cardiol. 2009 Jan 1;103(1):93-102 | CrossRef | PubMed | Philipson H, Ekman I, Swedberg K, Schaufelberger M. A pilot study of salt and water restriction in patients with chronic heart failure. Scand Cardiovasc J. 2010 Aug;44(4):209-14 | CrossRef | PubMed |
Philipson H, Ekman I, Swedberg K, Schaufelberger M. A pilot study of salt and water restriction in patients with chronic heart failure. Scand Cardiovasc J. 2010 Aug;44(4):209-14 | CrossRef | PubMed | Holst M, Strömberg A, Lindholm M, Willenheimer R. Description of self-reported fluid intake and its effects on body weight, symptoms, quality of life and physical capacity in patients with stable chronic heart failure. J Clin Nurs. 2008 Sep;17(17):2318-26 | CrossRef | PubMed |
Holst M, Strömberg A, Lindholm M, Willenheimer R. Description of self-reported fluid intake and its effects on body weight, symptoms, quality of life and physical capacity in patients with stable chronic heart failure. J Clin Nurs. 2008 Sep;17(17):2318-26 | CrossRef | PubMed | Falk S, Wahn AK, Lidell E. Keeping the maintenance of daily life in spite of chronic heart failure. A qualitative study. Eur J Cardiovasc Nurs. 2007 Sep;6(3):192-9 | PubMed |
Falk S, Wahn AK, Lidell E. Keeping the maintenance of daily life in spite of chronic heart failure. A qualitative study. Eur J Cardiovasc Nurs. 2007 Sep;6(3):192-9 | PubMed | Brännström M, Ekman I, Norberg A, Boman K, Strandberg G. Living with severe chronic heart failure in palliative advanced home care. Eur J Cardiovasc Nurs. 2006 Dec;5(4):295-302 | PubMed |
Brännström M, Ekman I, Norberg A, Boman K, Strandberg G. Living with severe chronic heart failure in palliative advanced home care. Eur J Cardiovasc Nurs. 2006 Dec;5(4):295-302 | PubMed | van der Wal MH, Jaarsma T, Moser DK, van Gilst WH, van Veldhuisen DJ. Qualitative examination of compliance in heart failure patients in The Netherlands. Heart Lung. 2010 Mar-Apr;39(2):121-30 | CrossRef | PubMed |
van der Wal MH, Jaarsma T, Moser DK, van Gilst WH, van Veldhuisen DJ. Qualitative examination of compliance in heart failure patients in The Netherlands. Heart Lung. 2010 Mar-Apr;39(2):121-30 | CrossRef | PubMed | Reilly CM, Meadows K, Dunbar S, Culler S, Smith A. Thirst and QOL in persons with heart failure. Heart & Lung: The Journal of Acute and Critical Care. 2010;39(4):353 | CrossRef |
Reilly CM, Meadows K, Dunbar S, Culler S, Smith A. Thirst and QOL in persons with heart failure. Heart & Lung: The Journal of Acute and Critical Care. 2010;39(4):353 | CrossRef | McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al; ESC Committee for Practice Guidelines. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847 | CrossRef | PubMed |
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al; ESC Committee for Practice Guidelines. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847 | CrossRef | PubMed | Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194 | CrossRef | PubMed |
Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194 | CrossRef | PubMed | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327 | CrossRef | PubMed |
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327 | CrossRef | PubMed | Finn Gustafsson. The Effect of Fluid Restriction in Congestive Heart Failure Complicated With Hyponatremia. NCT01748331 | Link |
Finn Gustafsson. The Effect of Fluid Restriction in Congestive Heart Failure Complicated With Hyponatremia. NCT01748331 | Link | Simon Stewart. The which heart failure intervention is most cost-effective in reducing hospital stay trial. ACTRN12613000921785 | Link |
Simon Stewart. The which heart failure intervention is most cost-effective in reducing hospital stay trial. ACTRN12613000921785 | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








