Abstract
Beta-blockers constitute standard therapy for heart failure with reduced ejection. However, their role in patients with preserved ejection fraction is not clear. Searching in Epistemonikos database, which is maintained by screening multiple databases, we identified four systematic reviews covering 19 primary studies, including seven randomized trials answering the question of this summary. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded the use of beta-blockers probably leads to little or no difference in the risk of death or hospitalization in patients with heart failure with preserved ejection fraction.
Problem
Around 50% of patients with heart failure have preserved ejection fraction, with or without diastolic dysfunction, and there is no treatment that is clearly effective.
Beta-blockers constitute standard therapy for heart failure with reduced ejection fraction. As they reduce heart rate it has been postulated they can also improve diastolic function, so constituting an alternative for patients with preserved ejection fraction. However, their clinical role is not clear.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found four systematic reviews [1],[2],[3],[4] including 19 primary studies, reported in 20 references [5],[6],[7], [8],[9],[10],[11],[12],[13],[14],[15],[16],[17],[18],[19],[20], |
|
What types of patients were included |
Ejection fraction was defined as >35% in one trial [9], > 40% in one trial [8] and > 45% in one trial [10]. Mean ejection fraction in the trials ranged from 49% to 63%. Even though trials did not restrict inclusion by functional class, most patients were NYHA II or III. All of the trials included adults. SENIORS trial restricted inclusion to patients over 70 years [9]. Mean age ranged from 66 to 76 years across studies. Between 66 and 86% of patients were hypertensive in the different trials, 3 to 24% had diabetes and 37 to 41% had atrial fibrillation. The latter were excluded in SWEDIC trial [10]. Etiology was ischemic in 77% of patients in SENIORS [9], 15% in J-DHF [8] and it was not reported in SWEDIC [10]. |
|
What types of interventions were included |
Two trials used carvedilol [8],[10] and one nebivolol [9]. In one trial carvedilol was initiated at 2.5 mg per day, then increasing up to 20 mg per day [8]; in the other trial initial dose was not reported, but the target dose was 25 or 50 mg depending on body weight [10]. Nebivolol starting dose was 1.25 mg per day, increasing up to 10 mg per day [9]. All of the trials compared against placebo. |
|
What types of outcomes |
The different systematic reviews identified groups outcomes as follows:
|
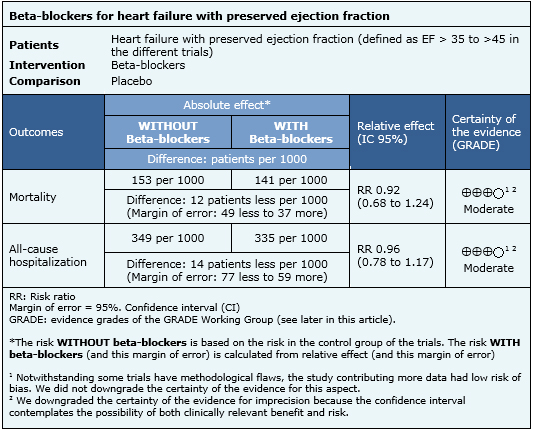
Summary of findings
The information on the effects of beta-blockers for heart failure with preserved ejection fraction is based on three randomized trials including 1094 participants. All of the trials reported mortality, but one did not have any event [10]. Only one trial reported all-cause hospitalization [9]. The summary of findings is the following:
- Use of beta-blockers probably leads to little or no difference in the risk of death in patients with heart failure with preserved ejection fraction. The certainty of the evidence is moderate.
- Use of beta-blockers probably leads to little or no difference in the risk of hospitalization in patients with heart failure with preserved ejection fraction. The certainty of the evidence is moderate.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
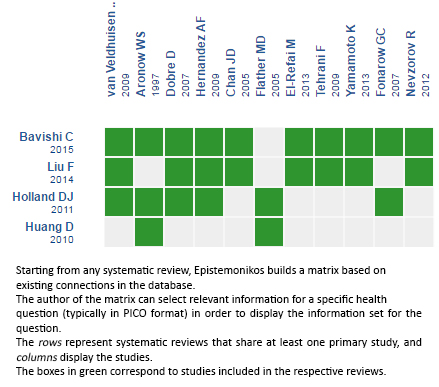
Follow the link to access the interactive version: Beta-blockers for heart failure with preserved ejection fraction.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Los betabloqueadores tienen un beneficio demostrado en el tratamiento de la insuficiencia cardíaca con fracción de eyección disminuida. Sin embargo, su rol en pacientes con fracción de eyección preservada no está tan claro. Utilizando la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en múltiples bases de datos, identificamos cuatro revisiones sistemáticas que en conjunto incluyen 19 estudios primarios, entre ellos siete estudios aleatorizados que responden la pregunta de este resumen. Realizamos un metanálisis y tablas de resumen de los resultados utilizando el método GRADE. Concluimos que el uso de betabloqueadores en pacientes con insuficiencia cardiaca con fracción de eyección preservada probablemente resulta en poca o nula diferencia en el riesgo de muerte u hospitalización por cualquier causa.
 Authors:
Javier Alegría [1,2 ], Gabriel Rada [1,2,3,4,5 ]
Authors:
Javier Alegría [1,2 ], Gabriel Rada [1,2,3,4,5 ]
Affiliation:
[1] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Programa de Salud Basada en Evidencia, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] GRADE working group
[5] The Cochrane Collaboration
E-mail: radagabriel@epistemonikos.org
Author address:
[1] Facultad de Medicina
Pontificia Universidad Católica de Chile
Lira 63
Santiago Centro
Chile

Citation: Alegría J , Rada G . Are beta-blockers effective in heart failure with preserved ejection fraction?. Medwave 2016;16(Suppl 5):e6593 doi: 10.5867/medwave.2016.6593
Publication date: 2/11/2016

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Bavishi C, Chatterjee S, Ather S, Patel D, Messerli FH. Beta-blockers in heart failure with preserved ejection fraction: a meta-analysis. Heart Fail Rev. 2015 Mar;20(2):193-201. | CrossRef |
- Holland DJ, Kumbhani DJ, Ahmed SH, Marwick TH. Effects of treatment on exercise tolerance, cardiac function, and mortality in heart failure with preserved ejection fraction. A meta-analysis. J Am Coll Cardiol. 2011 Apr 19;57(16):1676-86. | CrossRef | PubMed |
- Liu F, Chen Y, Feng X, Teng Z, Yuan Y, Bin J. Effects of beta-blockers on heart failure with preserved ejection fraction: a meta-analysis. PLoS One. 2014 Mar 5;9(3):e90555. | CrossRef | PubMed |
- Huang D, Cheng JW. Pharmacologic management of heart failure with preserved ejection fraction. Ann Pharmacother. 2010 Dec;44(12):1933-45. | CrossRef | PubMed |
- Nevzorov R, Porath A, Henkin Y, Kobal SL, Jotkowitz A, Novack V. Effect of beta blocker therapy on survival of patients with heart failure and preserved systolic function following hospitalization with acute decompensated heart failure. Eur J Intern Med. 2012 Jun;23(4):374-8. | CrossRef | PubMed |
- Smith DT, Farzaneh-Far R, Ali S, Na B, Whooley MA, Schiller NB. Relation of beta-blocker use with frequency of hospitalization for heart failure in patients with left ventricular diastolic dysfunction (from the Heart and Soul Study). Am J Cardiol. 2010 Jan 15;105(2):223-8. | CrossRef | PubMed |
- Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007 Aug 21;50(8):768-77. | PubMed |
- Yamamoto K, Origasa H, Hori M; J-DHF Investigators. Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013 Jan;15(1):110-8. | CrossRef | PubMed |
- van Veldhuisen DJ, Cohen-Solal A, Böhm M, Anker SD, Babalis D, Roughton M, et al. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). J Am Coll Cardiol. 2009 Jun 9;53(23):2150-8. | CrossRef | PubMed |
- Bergström A, Andersson B, Edner M, Nylander E, Persson H, Dahlström U. Effect of carvedilol on diastolic function in patients with diastolic heart failure and preserved systolic function. Results of the Swedish Doppler-echocardiographic study (SWEDIC). Eur J Heart Fail. 2004 Jun;6(4):453-61. | PubMed |
- Ghio S, Magrini G, Serio A, Klersy C, Fucili A, Ronaszèki A, et al. Effects of nebivolol in elderly heart failure patients with or without systolic left ventricular dysfunction: results of the SENIORS echocardiographic substudy. Eur Heart J. 2006 Mar;27(5):562-8. Epub 2006 Jan 27. Erratum in: Eur Heart J. 2006 Jul;27(14):1760. | PubMed |
- Gomez-Soto FM, Romero SP, Bernal JA, Escobar MA, Puerto JL, Andrey JL, et al. Mortality and morbidity of newly diagnosed heart failure with preserved systolic function treated with β-blockers: a propensity-adjusted case-control populational study. Int J Cardiol. 2011 Jan 7;146(1):51-5. | CrossRef | PubMed |
- Aronow WS, Ahn C, Kronzon I. Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction > or = 40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol. 1997 Jul 15;80(2):207-9. | PubMed |
- Farasat SM, Bolger DT, Shetty V, Menachery EP, Gerstenblith G, Kasper EK, et al. Effect of Beta-blocker therapy on rehospitalization rates in women versus men with heart failure and preserved ejection fraction. Am J Cardiol. 2010 Jan 15;105(2):229-34. | CrossRef | PubMed |
- Dobre D, van Veldhuisen DJ, DeJongste MJ, Lucas C, Cleuren G, Sanderman R, et al. Prescription of beta-blockers in patients with advanced heart failure and preserved left ventricular ejection fraction. Clinical implications and survival. Eur J Heart Fail. 2007 Mar;9(3):280-6. | PubMed |
- Nodari S, Metra M, Dei Cas L. Beta-blocker treatment of patients with diastolic heart failure and arterial hypertension. A prospective, randomized, comparison of the long-term effects of atenolol vs. nebivolol. Eur J Heart Fail. 2003 Oct;5(5):621-7. | PubMed |
- Flather MD, Shibata MC, Coats AJ, Van Veldhuisen DJ, Parkhomenko A, Borbola J, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005 Feb;26(3):215-25. | PubMed |
- Yanagihara K, Kinugasa Y, Sugihara S, Hirai M, Yamada K, Ishida K, et al. Discharge use of carvedilol is associated with higher survival in Japanese elderly patients with heart failure regardless of left ventricular ejection fraction. J Cardiovasc Pharmacol. 2013 Nov;62(5):485-90. | CrossRef | PubMed |
- Hernandez AF, Fonarow GC, Hammill BG, Al-Khatib SM, Yancy CW, O'Connor CM, et al. Clinical effectiveness of implantable cardioverter-defibrillators among medicare beneficiaries with heart failure. Circ Heart Fail. 2010 Jan;3(1):7-13. | CrossRef | PubMed |
- han JD, Rea TD, Smith NL, Siscovick D, Heckbert SR, Lumley T, et al. Association of beta-blocker use with mortality among patients with congestive heart failure in the Cardiovascular Health Study (CHS). Am Heart J. 2005 Sep;150(3):464-70. | PubMed |
- El-Refai M, Peterson EL, Wells K, Swadia T, Sabbah HN, Spertus JA, Williams LK, Lanfear DE. Comparison of β-blocker effectiveness in heart failure patients with preserved ejection fraction versus those with reduced ejection fraction. J Card Fail. 2013 Feb;19(2):73-9. | CrossRef | PubMed |
- Patel K, Fonarow GC, Ekundayo OJ, Aban IB, Kilgore ML, Love TE, et al. Beta-blockers in older patients with heart failure and preserved ejection fraction: class, dosage, and outcomes. Int J Cardiol. 2014 May 15;173(3):393-401. | CrossRef | PubMed |
- Tehrani F, Phan A, Chien CV, Morrissey RP, Rafique AM, Schwarz ER. Value of medical therapy in patients >80 years of age with heart failure and preserved ejection fraction. Am J Cardiol. 2009 Mar 15;103(6):829-33. | CrossRef | PubMed |
- Takeda Y, Fukutomi T, Suzuki S, Yamamoto K, Ogata M, Kondo H, et al. Effects of carvedilol on plasma B-type natriuretic peptide concentration and symptoms in patients with heart failure and preserved ejection fraction. Am J Cardiol. 2004 Aug 15;94(4):448-53. | PubMed |
- McMurray JJ V, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart. Eur Heart J. 2012 Jul;33(14):1787-847. | CrossRef | PubMed |
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327. | CrossRef | PubMed |
 Bavishi C, Chatterjee S, Ather S, Patel D, Messerli FH. Beta-blockers in heart failure with preserved ejection fraction: a meta-analysis. Heart Fail Rev. 2015 Mar;20(2):193-201. | CrossRef |
Bavishi C, Chatterjee S, Ather S, Patel D, Messerli FH. Beta-blockers in heart failure with preserved ejection fraction: a meta-analysis. Heart Fail Rev. 2015 Mar;20(2):193-201. | CrossRef | Holland DJ, Kumbhani DJ, Ahmed SH, Marwick TH. Effects of treatment on exercise tolerance, cardiac function, and mortality in heart failure with preserved ejection fraction. A meta-analysis. J Am Coll Cardiol. 2011 Apr 19;57(16):1676-86. | CrossRef | PubMed |
Holland DJ, Kumbhani DJ, Ahmed SH, Marwick TH. Effects of treatment on exercise tolerance, cardiac function, and mortality in heart failure with preserved ejection fraction. A meta-analysis. J Am Coll Cardiol. 2011 Apr 19;57(16):1676-86. | CrossRef | PubMed | Liu F, Chen Y, Feng X, Teng Z, Yuan Y, Bin J. Effects of beta-blockers on heart failure with preserved ejection fraction: a meta-analysis. PLoS One. 2014 Mar 5;9(3):e90555. | CrossRef | PubMed |
Liu F, Chen Y, Feng X, Teng Z, Yuan Y, Bin J. Effects of beta-blockers on heart failure with preserved ejection fraction: a meta-analysis. PLoS One. 2014 Mar 5;9(3):e90555. | CrossRef | PubMed | Huang D, Cheng JW. Pharmacologic management of heart failure with preserved ejection fraction. Ann Pharmacother. 2010 Dec;44(12):1933-45. | CrossRef | PubMed |
Huang D, Cheng JW. Pharmacologic management of heart failure with preserved ejection fraction. Ann Pharmacother. 2010 Dec;44(12):1933-45. | CrossRef | PubMed | Nevzorov R, Porath A, Henkin Y, Kobal SL, Jotkowitz A, Novack V. Effect of beta blocker therapy on survival of patients with heart failure and preserved systolic function following hospitalization with acute decompensated heart failure. Eur J Intern Med. 2012 Jun;23(4):374-8. | CrossRef | PubMed |
Nevzorov R, Porath A, Henkin Y, Kobal SL, Jotkowitz A, Novack V. Effect of beta blocker therapy on survival of patients with heart failure and preserved systolic function following hospitalization with acute decompensated heart failure. Eur J Intern Med. 2012 Jun;23(4):374-8. | CrossRef | PubMed | Smith DT, Farzaneh-Far R, Ali S, Na B, Whooley MA, Schiller NB. Relation of beta-blocker use with frequency of hospitalization for heart failure in patients with left ventricular diastolic dysfunction (from the Heart and Soul Study). Am J Cardiol. 2010 Jan 15;105(2):223-8. | CrossRef | PubMed |
Smith DT, Farzaneh-Far R, Ali S, Na B, Whooley MA, Schiller NB. Relation of beta-blocker use with frequency of hospitalization for heart failure in patients with left ventricular diastolic dysfunction (from the Heart and Soul Study). Am J Cardiol. 2010 Jan 15;105(2):223-8. | CrossRef | PubMed | Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007 Aug 21;50(8):768-77. | PubMed |
Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007 Aug 21;50(8):768-77. | PubMed | Yamamoto K, Origasa H, Hori M; J-DHF Investigators. Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013 Jan;15(1):110-8. | CrossRef | PubMed |
Yamamoto K, Origasa H, Hori M; J-DHF Investigators. Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013 Jan;15(1):110-8. | CrossRef | PubMed | van Veldhuisen DJ, Cohen-Solal A, Böhm M, Anker SD, Babalis D, Roughton M, et al. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). J Am Coll Cardiol. 2009 Jun 9;53(23):2150-8. | CrossRef | PubMed |
van Veldhuisen DJ, Cohen-Solal A, Böhm M, Anker SD, Babalis D, Roughton M, et al. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). J Am Coll Cardiol. 2009 Jun 9;53(23):2150-8. | CrossRef | PubMed | Bergström A, Andersson B, Edner M, Nylander E, Persson H, Dahlström U. Effect of carvedilol on diastolic function in patients with diastolic heart failure and preserved systolic function. Results of the Swedish Doppler-echocardiographic study (SWEDIC). Eur J Heart Fail. 2004 Jun;6(4):453-61. | PubMed |
Bergström A, Andersson B, Edner M, Nylander E, Persson H, Dahlström U. Effect of carvedilol on diastolic function in patients with diastolic heart failure and preserved systolic function. Results of the Swedish Doppler-echocardiographic study (SWEDIC). Eur J Heart Fail. 2004 Jun;6(4):453-61. | PubMed | Ghio S, Magrini G, Serio A, Klersy C, Fucili A, Ronaszèki A, et al. Effects of nebivolol in elderly heart failure patients with or without systolic left ventricular dysfunction: results of the SENIORS echocardiographic substudy. Eur Heart J. 2006 Mar;27(5):562-8. Epub 2006 Jan 27. Erratum in: Eur Heart J. 2006 Jul;27(14):1760. | PubMed |
Ghio S, Magrini G, Serio A, Klersy C, Fucili A, Ronaszèki A, et al. Effects of nebivolol in elderly heart failure patients with or without systolic left ventricular dysfunction: results of the SENIORS echocardiographic substudy. Eur Heart J. 2006 Mar;27(5):562-8. Epub 2006 Jan 27. Erratum in: Eur Heart J. 2006 Jul;27(14):1760. | PubMed | Gomez-Soto FM, Romero SP, Bernal JA, Escobar MA, Puerto JL, Andrey JL, et al. Mortality and morbidity of newly diagnosed heart failure with preserved systolic function treated with β-blockers: a propensity-adjusted case-control populational study. Int J Cardiol. 2011 Jan 7;146(1):51-5. | CrossRef | PubMed |
Gomez-Soto FM, Romero SP, Bernal JA, Escobar MA, Puerto JL, Andrey JL, et al. Mortality and morbidity of newly diagnosed heart failure with preserved systolic function treated with β-blockers: a propensity-adjusted case-control populational study. Int J Cardiol. 2011 Jan 7;146(1):51-5. | CrossRef | PubMed | Aronow WS, Ahn C, Kronzon I. Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction > or = 40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol. 1997 Jul 15;80(2):207-9. | PubMed |
Aronow WS, Ahn C, Kronzon I. Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction > or = 40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol. 1997 Jul 15;80(2):207-9. | PubMed | Farasat SM, Bolger DT, Shetty V, Menachery EP, Gerstenblith G, Kasper EK, et al. Effect of Beta-blocker therapy on rehospitalization rates in women versus men with heart failure and preserved ejection fraction. Am J Cardiol. 2010 Jan 15;105(2):229-34. | CrossRef | PubMed |
Farasat SM, Bolger DT, Shetty V, Menachery EP, Gerstenblith G, Kasper EK, et al. Effect of Beta-blocker therapy on rehospitalization rates in women versus men with heart failure and preserved ejection fraction. Am J Cardiol. 2010 Jan 15;105(2):229-34. | CrossRef | PubMed | Dobre D, van Veldhuisen DJ, DeJongste MJ, Lucas C, Cleuren G, Sanderman R, et al. Prescription of beta-blockers in patients with advanced heart failure and preserved left ventricular ejection fraction. Clinical implications and survival. Eur J Heart Fail. 2007 Mar;9(3):280-6. | PubMed |
Dobre D, van Veldhuisen DJ, DeJongste MJ, Lucas C, Cleuren G, Sanderman R, et al. Prescription of beta-blockers in patients with advanced heart failure and preserved left ventricular ejection fraction. Clinical implications and survival. Eur J Heart Fail. 2007 Mar;9(3):280-6. | PubMed | Nodari S, Metra M, Dei Cas L. Beta-blocker treatment of patients with diastolic heart failure and arterial hypertension. A prospective, randomized, comparison of the long-term effects of atenolol vs. nebivolol. Eur J Heart Fail. 2003 Oct;5(5):621-7. | PubMed |
Nodari S, Metra M, Dei Cas L. Beta-blocker treatment of patients with diastolic heart failure and arterial hypertension. A prospective, randomized, comparison of the long-term effects of atenolol vs. nebivolol. Eur J Heart Fail. 2003 Oct;5(5):621-7. | PubMed | Flather MD, Shibata MC, Coats AJ, Van Veldhuisen DJ, Parkhomenko A, Borbola J, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005 Feb;26(3):215-25. | PubMed |
Flather MD, Shibata MC, Coats AJ, Van Veldhuisen DJ, Parkhomenko A, Borbola J, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005 Feb;26(3):215-25. | PubMed | Yanagihara K, Kinugasa Y, Sugihara S, Hirai M, Yamada K, Ishida K, et al. Discharge use of carvedilol is associated with higher survival in Japanese elderly patients with heart failure regardless of left ventricular ejection fraction. J Cardiovasc Pharmacol. 2013 Nov;62(5):485-90. | CrossRef | PubMed |
Yanagihara K, Kinugasa Y, Sugihara S, Hirai M, Yamada K, Ishida K, et al. Discharge use of carvedilol is associated with higher survival in Japanese elderly patients with heart failure regardless of left ventricular ejection fraction. J Cardiovasc Pharmacol. 2013 Nov;62(5):485-90. | CrossRef | PubMed | Hernandez AF, Fonarow GC, Hammill BG, Al-Khatib SM, Yancy CW, O'Connor CM, et al. Clinical effectiveness of implantable cardioverter-defibrillators among medicare beneficiaries with heart failure. Circ Heart Fail. 2010 Jan;3(1):7-13. | CrossRef | PubMed |
Hernandez AF, Fonarow GC, Hammill BG, Al-Khatib SM, Yancy CW, O'Connor CM, et al. Clinical effectiveness of implantable cardioverter-defibrillators among medicare beneficiaries with heart failure. Circ Heart Fail. 2010 Jan;3(1):7-13. | CrossRef | PubMed | han JD, Rea TD, Smith NL, Siscovick D, Heckbert SR, Lumley T, et al. Association of beta-blocker use with mortality among patients with congestive heart failure in the Cardiovascular Health Study (CHS). Am Heart J. 2005 Sep;150(3):464-70. | PubMed |
han JD, Rea TD, Smith NL, Siscovick D, Heckbert SR, Lumley T, et al. Association of beta-blocker use with mortality among patients with congestive heart failure in the Cardiovascular Health Study (CHS). Am Heart J. 2005 Sep;150(3):464-70. | PubMed | El-Refai M, Peterson EL, Wells K, Swadia T, Sabbah HN, Spertus JA, Williams LK, Lanfear DE. Comparison of β-blocker effectiveness in heart failure patients with preserved ejection fraction versus those with reduced ejection fraction. J Card Fail. 2013 Feb;19(2):73-9. | CrossRef | PubMed |
El-Refai M, Peterson EL, Wells K, Swadia T, Sabbah HN, Spertus JA, Williams LK, Lanfear DE. Comparison of β-blocker effectiveness in heart failure patients with preserved ejection fraction versus those with reduced ejection fraction. J Card Fail. 2013 Feb;19(2):73-9. | CrossRef | PubMed | Patel K, Fonarow GC, Ekundayo OJ, Aban IB, Kilgore ML, Love TE, et al. Beta-blockers in older patients with heart failure and preserved ejection fraction: class, dosage, and outcomes. Int J Cardiol. 2014 May 15;173(3):393-401. | CrossRef | PubMed |
Patel K, Fonarow GC, Ekundayo OJ, Aban IB, Kilgore ML, Love TE, et al. Beta-blockers in older patients with heart failure and preserved ejection fraction: class, dosage, and outcomes. Int J Cardiol. 2014 May 15;173(3):393-401. | CrossRef | PubMed | Tehrani F, Phan A, Chien CV, Morrissey RP, Rafique AM, Schwarz ER. Value of medical therapy in patients >80 years of age with heart failure and preserved ejection fraction. Am J Cardiol. 2009 Mar 15;103(6):829-33. | CrossRef | PubMed |
Tehrani F, Phan A, Chien CV, Morrissey RP, Rafique AM, Schwarz ER. Value of medical therapy in patients >80 years of age with heart failure and preserved ejection fraction. Am J Cardiol. 2009 Mar 15;103(6):829-33. | CrossRef | PubMed | Takeda Y, Fukutomi T, Suzuki S, Yamamoto K, Ogata M, Kondo H, et al. Effects of carvedilol on plasma B-type natriuretic peptide concentration and symptoms in patients with heart failure and preserved ejection fraction. Am J Cardiol. 2004 Aug 15;94(4):448-53. | PubMed |
Takeda Y, Fukutomi T, Suzuki S, Yamamoto K, Ogata M, Kondo H, et al. Effects of carvedilol on plasma B-type natriuretic peptide concentration and symptoms in patients with heart failure and preserved ejection fraction. Am J Cardiol. 2004 Aug 15;94(4):448-53. | PubMed | McMurray JJ V, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart. Eur Heart J. 2012 Jul;33(14):1787-847. | CrossRef | PubMed |
McMurray JJ V, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart. Eur Heart J. 2012 Jul;33(14):1787-847. | CrossRef | PubMed | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327. | CrossRef | PubMed |
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








