Abstract
Variceal bleeding is one of the most serious complications of liver cirrhosis. Nonselective beta-blockers and endoscopic ligation are considered effective strategies for primary prevention of variceal bleeding, but there is no consensus about which alternative constitutes the best option. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified seven systematic reviews including 21 randomized controlled trials addressing the question of this article. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded variceal ligation probably decreases the risk of variceal bleeding and it is associated to less adverse effects when compared with nonselective beta blockers, although probably there is no difference in terms of mortality.
Problem
Gastro-esophageal varices are common in liver cirrhosis. The prevalence in stable cirrhosis varies between 30 and 40%, while in decompensated cirrhosis it reaches 60%. In patients with varices, the annual risk of bleeding is estimated at 30%, with a mortality rate ranging from 20 to 50% in each episode [1]. Nonselective beta-blockers are low-cost drugs that have proven effective in preventing variceal bleeding [2],[3], through reduction in porto-systemic pressure gradient, an important factor conditioning the rupture of varices. However, some patients do not tolerate them because of adverse effects. On the other hand, endoscopic ligation with elastic bands also prevents variceal bleeding in high risk patients [4],[5], but they have a higher cost, are more difficult to implement and have other associated risks. The aim of this article is to summarize the evidence comparing both prophylactic alternatives in patients with liver cirrhosis and high risk of variceal upper gastrointestinal bleeding.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found seven systematic reviews [1],[4],[5],[6],[7], [8],[9] including 21 randomized controlled trials reported in 26 references addressing the question of interest [10], [11],[12],[13],[14],[15],[16],[17],[18],[19],[20],[21], [22],[23],[24],[25],[26],[27],[28],[29],[30],[31],[32], [33],[34],[35]. |
|
What types of patients were included |
All of the studies included patients with liver cirrhosis and presence of high-risk of bleeding varices, either by their large size (grade III or IV) or red spots. |
|
What types of interventions were included |
Eighteen trials [10],[12],[14],[15],[16],[17],[18],[19], [20],[21],[22],[25],[29],[30],[31],[32],[33],[34], used propranolol as beta-blocker, one trial [26] used nadolol, another [28] used carvedilol and one study [35] did not report the type of beta blocking agent used. Nine studies [12],[14],[19],[21],[25],[29],[30],[31],[34], conducted more than three ligation sessions and four studies [16],[17],[26],[28] performed fewer than three sessions. The other eight studies [10],[15],[18],[20],[22],[27],[32],[33] did not report the number of ligation sessions. Follow-up was longer than 1 year in all studies. |
|
What types of outcomes |
The studies measured multiple outcomes, however those incorporated by most systematic reviews were: Overall mortality, bleeding related mortality, upper gastrointestinal bleeding from any cause and adverse effects. |
Summary of findings
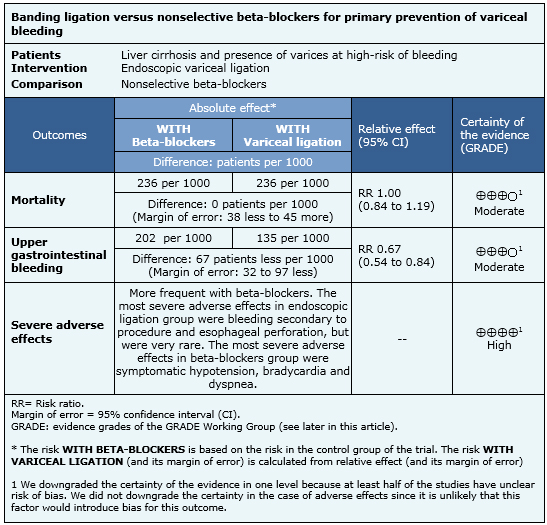
The information on the comparison between nonselective beta-blockers and ligation in primary prophylaxis of variceal bleeding is based on 21 randomized controlled trials involving 1659 patients. Twenty trials measured overall mortality (one study did not report this outcome [35]), 14 studies measured upper gastrointestinal bleeding from any cause and 10 studies evaluated adverse effects. The summary of findings is as follows:
- Primary prophylaxis with variceal ligation probably has little or no effect on the risk of mortality compared with nonselective beta blockers. The certainty of the evidence is moderate.
- Primary prophylaxis with variceal ligation probably reduces the risk of bleeding compared with nonselective beta-blockers. The certainty of the evidence is moderate.
- Primary prophylaxis with variceal ligation is associated to fewer adverse effects in comparison to nonselective beta-blockers. The certainty of the evidence is high.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
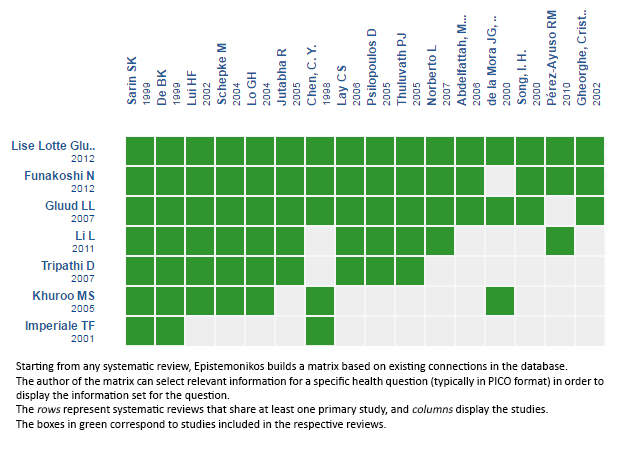
Follow the link to access the interactive version: Banding ligation versus beta-blockers for primary prevention of variceal bleeding.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

La hemorragia digestiva alta variceal es una de las complicaciones más serias de la cirrosis hepática. Los betabloqueadores no selectivos y la ligadura endoscópica se consideran efectivos como estrategia de prevención primaria de hemorragia variceal, pero no hay consenso sobre cuál de las dos constituye la mejor opción. Utilizando la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en 30 bases de datos, identificamos siete revisiones sistemáticas que en conjunto incluyen 21 estudios aleatorizados. Realizamos un metanálisis y tablas de resumen de los resultados utilizando el método GRADE. Concluimos que la ligadura variceal probablemente disminuye el riesgo de sangrado digestivo variceal y se asocia a menos efectos adversos al ser comparada con betabloqueadores no selectivos, aunque probablemente no existen diferencias en términos de mortalidad.
 Authors:
Petre Cotoras Viedma[1,2], Roberto Candia[1,2,3,4]
Authors:
Petre Cotoras Viedma[1,2], Roberto Candia[1,2,3,4]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Programa de Salud Basada en Evidencia, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Departamento de Gastroenterología, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
E-mail: roberto.candia@gmail.com
Author address:
[1] Facultad de Medicina
Pontificia Universidad Católica de Chile
Lira 63
Santiago Centro
Chile

Citation: Cotoras Viedma P, Candia R. Banding ligation or beta-blockers for primary prevention of variceal bleeding?. Medwave 2016;16(Suppl 5):e6564 doi: 10.5867/medwave.2016.6564
Publication date: 4/10/2016

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Funakoshi N, Duny Y, Valats JC, Ségalas-Largey F, Flori N, Bismuth M, et al. Meta-analysis: beta-blockers versus banding ligation for primary prophylaxis of esophageal variceal bleeding. Ann Hepatol. 2012 May-Jun;11(3):369-83. | PubMed |
- Pagliaro L, D'Amico G, Sörensen TI, Lebrec D, Burroughs AK, Morabito A, et al. Prevention of first bleeding in cirrhosis. A meta-analysis of randomized trials of nonsurgical treatment. Ann Intern Med. 1992 Jul 1;117(1):59-70. | PubMed |
- D'Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19(4):475-505. | PubMed |
- Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD004544. | CrossRef | PubMed |
- Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD004544. | CrossRef | PubMed |
- Imperiale TF, Chalasani N. A meta-analysis of endoscopic variceal ligation for primary prophylaxis of esophageal variceal bleeding. Hepatology. 2001 Apr;33(4):802-7. | PubMed |
- Li L, Yu C, Li Y. Endoscopic band ligation versus pharmacological therapy for variceal bleeding in cirrhosis: a meta-analysis. Can J Gastroenterol. 2011 Mar;25(3):147-55. | PubMed |
- Khuroo MS, Khuroo NS, Farahat KL, Khuroo YS, Sofi AA, Dahab ST. Meta-analysis: endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleeding. Aliment Pharmacol Ther. 2005 Feb 15;21(4):347-61. | PubMed |
- Tripathi D, Graham C, Hayes PC. Variceal band ligation versus beta-blockers for primary prevention of variceal bleeding: a meta-analysis. Eur J Gastroenterol Hepatol. 2007 Oct;19(10):835-45. | PubMed |
- Gheorghe C, Gheorghe L, Vadan R, Hrehoret D, Popescu I. Prophylactic banding ligation of high risk esophageal varices inpatients on the waiting list for liver transplantation: an interim report. J Hepatol. 2002;36(Suppl 1):38. | CrossRef |
- Drastich P, Lata J, Petrtyl J, Bruha R, Prochazka V, Vanasek T, et al. Endoscopic variceal band ligation compared with propranolol for prophylaxis of first variceal bleeding. Ann Hepatol. 2011 Apr-Jun;10(2):142-9. | PubMed |
- Psilopoulos D, Galanis P, Goulas S, Papanikolaou IS, Elefsiniotis I, Liatsos C, et al. Endoscopic variceal ligation vs. ropranolol for prevention of first variceal bleeding: a randomized controlled trial. Eur J Gastroenterol Hepatol. 2005 Oct;17(10):1111-7. | PubMed |
- Schepke M, Kleber G, Nürnberg D, Willert J, Koch L, Veltzke-Schlieker W, et al. Ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology. 2004 Jul;40(1):65-72. | PubMed |
- Norberto L, Polese L, Cillo U, Grigoletto F, Burroughs AK, Neri D, et al. A randomized study comparing ligation with propranolol for primary prophylaxis of variceal bleeding in candidates for liver transplantation. Liver Transpl. 2007 Sep;13(9):1272-8. | PubMed |
- Lopez-Acosta ME, Mora-Levy J-G, Blancas-Valencia J-M, Paz-Flores V-M. Primary prophylaxis of variceal bleeding comparing propranolol versus recharging a multiple band ligator: up to 4 years follow-up. Gastrointestinal Endoscopy.2002;55(5):AB195.
- Thuluvath PJ, Maheshwari A, Jagannath S, Arepally A. A randomized controlled trial of beta-blockers versus endoscopic band ligation for primary prophylaxis: a large sample size is required to show a difference in bleeding rates. Dig Dis Sci. 2005 Feb;50(2):407-10. | PubMed |
- Schepke M, Kleber G, Nürnberg D, Willert J, Koch L, Veltzke-Schlieker W, et al. Ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology. 2004 Jul;40(1):65-72. | PubMed |
- Song, I. H., Shin, J. W., Kim, I. H., Choi, J., Lim, C. Y., Kim, J. W., Roe, I. H.. A prospective randomized trial between the prophylactic endoscopic variceal ligation and propranolol administration for prevention of first bleeding in cirrhotic patients with high-risk esophageal varices. J Hepatol. 2000;32(Suppl 2):41.
- Lay CS, Tsai YT, Lee FY, Lai YL, Yu CJ, Chen CB, et al. Endoscopic variceal ligation versus propranolol in prophylaxis of first variceal bleeding in patients with cirrhosis. J Gastroenterol Hepatol. 2006 Feb;21(2):413-9. | PubMed |
- Drastich P, Lata J, Petrtyl J, Bruha R, Prochazka V, Vanasek T, Zdenek P, Skibova J, Hucl T, Spicak J. Endoscopic variceal band ligation compared with propranolol for prophylaxis of first variceal bleeding. Annals of hepatology. 2011;10(2):142-9.
- Chen CY, Sheu MZ, Su SY. Prophylactic endoscopic variceal ligation (EVL) with multiple band ligator for esophageal varices. Gastroenterology. 1998;114:A1224. | CrossRef |
- de la Mora JG, Farca-Belsaguy AA, Uribe M, de Hoyos-Garza A. Ligation vs propranolol for primary prophylaxis of variceal bleeding using multiple band ligator and objective measurements of treatment adequacy: preliminary results. Gastroenterology. 2000;118(4 Part 2):A1434–A1435. | CrossRef |
- Jutbha R, Jensen DM, Martin P, et al. Initial report of a randomized, prospective study of prophylactic propranolol compared to rubber band ligation for prevention of first variceal hemorrhage in cirrhotics with large oesophageal varices. Gastroenterology. 2000;118:212. | Link |
- Lui HF, Stanley AJ, Forrest EH, Jalan R, Hislop WS, Mills PR, et al. Primary prophylaxis of variceal hemorrhage: a randomized controlled trial comparing band ligation, propranolol, and isosorbide mononitrate. Gastroenterology. 2002 Sep;123(3):735-44. | PubMed |
- De BK, Ghoshal UC, Das T, Santra A, Biswas PK. Endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleed: preliminary report of a randomized controlled trial. J Gastroenterol Hepatol. 1999 Mar;14(3):220-4. | PubMed |
- Lo GH, Chen WC, Chen MH, Lin CP, Lo CC, Hsu PI, Cheng JS, Lai KH. Endoscopic ligation vs. nadolol in the prevention of first variceal bleeding in patients with cirrhosis. Gastrointest Endosc. 2004 Mar;59(3):333-8. | PubMed |
- Sarin, SK, Lamba, GS, Kumar, M, Mishra, A, Murthy, NS. Randomized trial of propranolol vs. endoscopic variceal ligation (EVL) in the primary prophylaxis of bleeding from high risk varices in cirrhosis: An interim analysis. Hepatology. 1997;26(4):928-928.
- Tripathi D, Ferguson JW, Kochar N, Leithead JA, Therapondos G, McAvoy NC, et al. Randomized controlled trial of carvedilol versus variceal band ligation for the prevention of the first variceal bleed. Hepatology. 2009 Sep;50(3):825-33. | CrossRef | PubMed |
- Jutabha R, Jensen DM, Martin P, Savides T, Han SH, Gornbein J. Randomized study comparing banding and propranolol to prevent initial variceal hemorrhage in cirrhotics with high-risk esophageal varices. Gastroenterology. 2005 Apr;128(4):870-81. | PubMed |
- Lui HF, Stanley AJ, Forrest EH, Jalan R, Hislop WS, Mills PR, et al. Primary prophylaxis of variceal hemorrhage: a randomized controlled trial comparing band ligation, propranolol, and isosorbide mononitrate. Gastroenterology. 2002 Sep;123(3):735-44. | PubMed |
- Sarin SK, Lamba GS, Kumar M, Misra A, Murthy NS. Comparison of endoscopic ligation and propranolol for the primary prevention of variceal bleeding. N Engl J Med. 1999 Apr 1;340(13):988-93. | PubMed |
- Abdelfattah, M.H., Rashed, M.A., Elfakhry, A.A., Soliman, M.A., Shiha, G.E.. Endoscopic variceal ligation versus pharmacologic treatment for primary prophylaxis of variceal bleeding: a randomised study. Journal of Hepatology. 2006;44:S83-S83. | CrossRef |
- Abulfutuh, AR, Morsy, M, Solyman, AEG. Study of variceal band ligation, propranolol and isosorbide mononitrate in the prevention of the first variceal bleeding. Gastroenterology. 2003;124(4):A780-A780. | CrossRef |
- Pérez-Ayuso RM, Valderrama S, Espinoza M, Rollán A, Sánchez R, Otarola F, et al. Endoscopic band ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhotic patients with high risk esophageal varices. Ann Hepatol. 2010 Jan-Mar;9(1):15-22. | PubMed |
- Gill M, Sattar S, Khokhar N. Outcomes of endoscopic variceal band ligation versus pharmacological treatment with non selective beta blocker for primary prophylaxis of variceal bleed. Gut. 2006;55:A308.
- de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015 Sep;63(3):743-52. | CrossRef | PubMed |
- Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, et al. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015 Nov;64(11):1680-704. | CrossRef | PubMed |
- Endoscopic Band Ligation (EBL) Versus Propranolol for Primary Prophylaxis of Variceal Bleeding 2009 [on line]. | Link |
 Funakoshi N, Duny Y, Valats JC, Ségalas-Largey F, Flori N, Bismuth M, et al. Meta-analysis: beta-blockers versus banding ligation for primary prophylaxis of esophageal variceal bleeding. Ann Hepatol. 2012 May-Jun;11(3):369-83. | PubMed |
Funakoshi N, Duny Y, Valats JC, Ségalas-Largey F, Flori N, Bismuth M, et al. Meta-analysis: beta-blockers versus banding ligation for primary prophylaxis of esophageal variceal bleeding. Ann Hepatol. 2012 May-Jun;11(3):369-83. | PubMed | Pagliaro L, D'Amico G, Sörensen TI, Lebrec D, Burroughs AK, Morabito A, et al. Prevention of first bleeding in cirrhosis. A meta-analysis of randomized trials of nonsurgical treatment. Ann Intern Med. 1992 Jul 1;117(1):59-70. | PubMed |
Pagliaro L, D'Amico G, Sörensen TI, Lebrec D, Burroughs AK, Morabito A, et al. Prevention of first bleeding in cirrhosis. A meta-analysis of randomized trials of nonsurgical treatment. Ann Intern Med. 1992 Jul 1;117(1):59-70. | PubMed | D'Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19(4):475-505. | PubMed |
D'Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19(4):475-505. | PubMed | Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD004544. | CrossRef | PubMed |
Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD004544. | CrossRef | PubMed | Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD004544. | CrossRef | PubMed |
Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012 Aug 15;(8):CD004544. | CrossRef | PubMed | Imperiale TF, Chalasani N. A meta-analysis of endoscopic variceal ligation for primary prophylaxis of esophageal variceal bleeding. Hepatology. 2001 Apr;33(4):802-7. | PubMed |
Imperiale TF, Chalasani N. A meta-analysis of endoscopic variceal ligation for primary prophylaxis of esophageal variceal bleeding. Hepatology. 2001 Apr;33(4):802-7. | PubMed | Li L, Yu C, Li Y. Endoscopic band ligation versus pharmacological therapy for variceal bleeding in cirrhosis: a meta-analysis. Can J Gastroenterol. 2011 Mar;25(3):147-55. | PubMed |
Li L, Yu C, Li Y. Endoscopic band ligation versus pharmacological therapy for variceal bleeding in cirrhosis: a meta-analysis. Can J Gastroenterol. 2011 Mar;25(3):147-55. | PubMed | Khuroo MS, Khuroo NS, Farahat KL, Khuroo YS, Sofi AA, Dahab ST. Meta-analysis: endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleeding. Aliment Pharmacol Ther. 2005 Feb 15;21(4):347-61. | PubMed |
Khuroo MS, Khuroo NS, Farahat KL, Khuroo YS, Sofi AA, Dahab ST. Meta-analysis: endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleeding. Aliment Pharmacol Ther. 2005 Feb 15;21(4):347-61. | PubMed | Tripathi D, Graham C, Hayes PC. Variceal band ligation versus beta-blockers for primary prevention of variceal bleeding: a meta-analysis. Eur J Gastroenterol Hepatol. 2007 Oct;19(10):835-45. | PubMed |
Tripathi D, Graham C, Hayes PC. Variceal band ligation versus beta-blockers for primary prevention of variceal bleeding: a meta-analysis. Eur J Gastroenterol Hepatol. 2007 Oct;19(10):835-45. | PubMed | Gheorghe C, Gheorghe L, Vadan R, Hrehoret D, Popescu I. Prophylactic banding ligation of high risk esophageal varices inpatients on the waiting list for liver transplantation: an interim report. J Hepatol. 2002;36(Suppl 1):38. | CrossRef |
Gheorghe C, Gheorghe L, Vadan R, Hrehoret D, Popescu I. Prophylactic banding ligation of high risk esophageal varices inpatients on the waiting list for liver transplantation: an interim report. J Hepatol. 2002;36(Suppl 1):38. | CrossRef | Drastich P, Lata J, Petrtyl J, Bruha R, Prochazka V, Vanasek T, et al. Endoscopic variceal band ligation compared with propranolol for prophylaxis of first variceal bleeding. Ann Hepatol. 2011 Apr-Jun;10(2):142-9. | PubMed |
Drastich P, Lata J, Petrtyl J, Bruha R, Prochazka V, Vanasek T, et al. Endoscopic variceal band ligation compared with propranolol for prophylaxis of first variceal bleeding. Ann Hepatol. 2011 Apr-Jun;10(2):142-9. | PubMed | Psilopoulos D, Galanis P, Goulas S, Papanikolaou IS, Elefsiniotis I, Liatsos C, et al. Endoscopic variceal ligation vs. ropranolol for prevention of first variceal bleeding: a randomized controlled trial. Eur J Gastroenterol Hepatol. 2005 Oct;17(10):1111-7. | PubMed |
Psilopoulos D, Galanis P, Goulas S, Papanikolaou IS, Elefsiniotis I, Liatsos C, et al. Endoscopic variceal ligation vs. ropranolol for prevention of first variceal bleeding: a randomized controlled trial. Eur J Gastroenterol Hepatol. 2005 Oct;17(10):1111-7. | PubMed | Schepke M, Kleber G, Nürnberg D, Willert J, Koch L, Veltzke-Schlieker W, et al. Ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology. 2004 Jul;40(1):65-72. | PubMed |
Schepke M, Kleber G, Nürnberg D, Willert J, Koch L, Veltzke-Schlieker W, et al. Ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology. 2004 Jul;40(1):65-72. | PubMed | Norberto L, Polese L, Cillo U, Grigoletto F, Burroughs AK, Neri D, et al. A randomized study comparing ligation with propranolol for primary prophylaxis of variceal bleeding in candidates for liver transplantation. Liver Transpl. 2007 Sep;13(9):1272-8. | PubMed |
Norberto L, Polese L, Cillo U, Grigoletto F, Burroughs AK, Neri D, et al. A randomized study comparing ligation with propranolol for primary prophylaxis of variceal bleeding in candidates for liver transplantation. Liver Transpl. 2007 Sep;13(9):1272-8. | PubMed | Lopez-Acosta ME, Mora-Levy J-G, Blancas-Valencia J-M, Paz-Flores V-M. Primary prophylaxis of variceal bleeding comparing propranolol versus recharging a multiple band ligator: up to 4 years follow-up. Gastrointestinal Endoscopy.2002;55(5):AB195.
Lopez-Acosta ME, Mora-Levy J-G, Blancas-Valencia J-M, Paz-Flores V-M. Primary prophylaxis of variceal bleeding comparing propranolol versus recharging a multiple band ligator: up to 4 years follow-up. Gastrointestinal Endoscopy.2002;55(5):AB195.  Thuluvath PJ, Maheshwari A, Jagannath S, Arepally A. A randomized controlled trial of beta-blockers versus endoscopic band ligation for primary prophylaxis: a large sample size is required to show a difference in bleeding rates. Dig Dis Sci. 2005 Feb;50(2):407-10. | PubMed |
Thuluvath PJ, Maheshwari A, Jagannath S, Arepally A. A randomized controlled trial of beta-blockers versus endoscopic band ligation for primary prophylaxis: a large sample size is required to show a difference in bleeding rates. Dig Dis Sci. 2005 Feb;50(2):407-10. | PubMed | Schepke M, Kleber G, Nürnberg D, Willert J, Koch L, Veltzke-Schlieker W, et al. Ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology. 2004 Jul;40(1):65-72. | PubMed |
Schepke M, Kleber G, Nürnberg D, Willert J, Koch L, Veltzke-Schlieker W, et al. Ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology. 2004 Jul;40(1):65-72. | PubMed | Song, I. H., Shin, J. W., Kim, I. H., Choi, J., Lim, C. Y., Kim, J. W., Roe, I. H.. A prospective randomized trial between the prophylactic endoscopic variceal ligation and propranolol administration for prevention of first bleeding in cirrhotic patients with high-risk esophageal varices. J Hepatol. 2000;32(Suppl 2):41.
Song, I. H., Shin, J. W., Kim, I. H., Choi, J., Lim, C. Y., Kim, J. W., Roe, I. H.. A prospective randomized trial between the prophylactic endoscopic variceal ligation and propranolol administration for prevention of first bleeding in cirrhotic patients with high-risk esophageal varices. J Hepatol. 2000;32(Suppl 2):41.  Lay CS, Tsai YT, Lee FY, Lai YL, Yu CJ, Chen CB, et al. Endoscopic variceal ligation versus propranolol in prophylaxis of first variceal bleeding in patients with cirrhosis. J Gastroenterol Hepatol. 2006 Feb;21(2):413-9. | PubMed |
Lay CS, Tsai YT, Lee FY, Lai YL, Yu CJ, Chen CB, et al. Endoscopic variceal ligation versus propranolol in prophylaxis of first variceal bleeding in patients with cirrhosis. J Gastroenterol Hepatol. 2006 Feb;21(2):413-9. | PubMed | Drastich P, Lata J, Petrtyl J, Bruha R, Prochazka V, Vanasek T, Zdenek P, Skibova J, Hucl T, Spicak J. Endoscopic variceal band ligation compared with propranolol for prophylaxis of first variceal bleeding. Annals of hepatology. 2011;10(2):142-9.
Drastich P, Lata J, Petrtyl J, Bruha R, Prochazka V, Vanasek T, Zdenek P, Skibova J, Hucl T, Spicak J. Endoscopic variceal band ligation compared with propranolol for prophylaxis of first variceal bleeding. Annals of hepatology. 2011;10(2):142-9.  Chen CY, Sheu MZ, Su SY. Prophylactic endoscopic variceal ligation (EVL) with multiple band ligator for esophageal varices. Gastroenterology. 1998;114:A1224. | CrossRef |
Chen CY, Sheu MZ, Su SY. Prophylactic endoscopic variceal ligation (EVL) with multiple band ligator for esophageal varices. Gastroenterology. 1998;114:A1224. | CrossRef | de la Mora JG, Farca-Belsaguy AA, Uribe M, de Hoyos-Garza A. Ligation vs propranolol for primary prophylaxis of variceal bleeding using multiple band ligator and objective measurements of treatment adequacy: preliminary results. Gastroenterology. 2000;118(4 Part 2):A1434–A1435. | CrossRef |
de la Mora JG, Farca-Belsaguy AA, Uribe M, de Hoyos-Garza A. Ligation vs propranolol for primary prophylaxis of variceal bleeding using multiple band ligator and objective measurements of treatment adequacy: preliminary results. Gastroenterology. 2000;118(4 Part 2):A1434–A1435. | CrossRef | Jutbha R, Jensen DM, Martin P, et al. Initial report of a randomized, prospective study of prophylactic propranolol compared to rubber band ligation for prevention of first variceal hemorrhage in cirrhotics with large oesophageal varices. Gastroenterology. 2000;118:212.
| Link |
Jutbha R, Jensen DM, Martin P, et al. Initial report of a randomized, prospective study of prophylactic propranolol compared to rubber band ligation for prevention of first variceal hemorrhage in cirrhotics with large oesophageal varices. Gastroenterology. 2000;118:212.
| Link | Lui HF, Stanley AJ, Forrest EH, Jalan R, Hislop WS, Mills PR, et al. Primary prophylaxis of variceal hemorrhage: a randomized controlled trial comparing band ligation, propranolol, and isosorbide mononitrate. Gastroenterology. 2002 Sep;123(3):735-44. | PubMed |
Lui HF, Stanley AJ, Forrest EH, Jalan R, Hislop WS, Mills PR, et al. Primary prophylaxis of variceal hemorrhage: a randomized controlled trial comparing band ligation, propranolol, and isosorbide mononitrate. Gastroenterology. 2002 Sep;123(3):735-44. | PubMed | De BK, Ghoshal UC, Das T, Santra A, Biswas PK. Endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleed: preliminary report of a randomized controlled trial. J Gastroenterol Hepatol. 1999 Mar;14(3):220-4. | PubMed |
De BK, Ghoshal UC, Das T, Santra A, Biswas PK. Endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleed: preliminary report of a randomized controlled trial. J Gastroenterol Hepatol. 1999 Mar;14(3):220-4. | PubMed | Lo GH, Chen WC, Chen MH, Lin CP, Lo CC, Hsu PI, Cheng JS, Lai KH. Endoscopic ligation vs. nadolol in the prevention of first variceal bleeding in patients with cirrhosis. Gastrointest Endosc. 2004 Mar;59(3):333-8. | PubMed |
Lo GH, Chen WC, Chen MH, Lin CP, Lo CC, Hsu PI, Cheng JS, Lai KH. Endoscopic ligation vs. nadolol in the prevention of first variceal bleeding in patients with cirrhosis. Gastrointest Endosc. 2004 Mar;59(3):333-8. | PubMed | Sarin, SK, Lamba, GS, Kumar, M, Mishra, A, Murthy, NS. Randomized trial of propranolol vs. endoscopic variceal ligation (EVL) in the primary prophylaxis of bleeding from high risk varices in cirrhosis: An interim analysis. Hepatology. 1997;26(4):928-928.
Sarin, SK, Lamba, GS, Kumar, M, Mishra, A, Murthy, NS. Randomized trial of propranolol vs. endoscopic variceal ligation (EVL) in the primary prophylaxis of bleeding from high risk varices in cirrhosis: An interim analysis. Hepatology. 1997;26(4):928-928.  Tripathi D, Ferguson JW, Kochar N, Leithead JA, Therapondos G, McAvoy NC, et al. Randomized controlled trial of carvedilol versus variceal band ligation for the prevention of the first variceal bleed. Hepatology. 2009 Sep;50(3):825-33. | CrossRef | PubMed |
Tripathi D, Ferguson JW, Kochar N, Leithead JA, Therapondos G, McAvoy NC, et al. Randomized controlled trial of carvedilol versus variceal band ligation for the prevention of the first variceal bleed. Hepatology. 2009 Sep;50(3):825-33. | CrossRef | PubMed | Jutabha R, Jensen DM, Martin P, Savides T, Han SH, Gornbein J. Randomized study comparing banding and propranolol to prevent initial variceal hemorrhage in cirrhotics with high-risk esophageal varices. Gastroenterology. 2005 Apr;128(4):870-81. | PubMed |
Jutabha R, Jensen DM, Martin P, Savides T, Han SH, Gornbein J. Randomized study comparing banding and propranolol to prevent initial variceal hemorrhage in cirrhotics with high-risk esophageal varices. Gastroenterology. 2005 Apr;128(4):870-81. | PubMed | Lui HF, Stanley AJ, Forrest EH, Jalan R, Hislop WS, Mills PR, et al. Primary prophylaxis of variceal hemorrhage: a randomized controlled trial comparing band ligation, propranolol, and isosorbide mononitrate. Gastroenterology. 2002 Sep;123(3):735-44. | PubMed |
Lui HF, Stanley AJ, Forrest EH, Jalan R, Hislop WS, Mills PR, et al. Primary prophylaxis of variceal hemorrhage: a randomized controlled trial comparing band ligation, propranolol, and isosorbide mononitrate. Gastroenterology. 2002 Sep;123(3):735-44. | PubMed | Sarin SK, Lamba GS, Kumar M, Misra A, Murthy NS. Comparison of endoscopic ligation and propranolol for the primary prevention of variceal bleeding. N Engl J Med. 1999 Apr 1;340(13):988-93. | PubMed |
Sarin SK, Lamba GS, Kumar M, Misra A, Murthy NS. Comparison of endoscopic ligation and propranolol for the primary prevention of variceal bleeding. N Engl J Med. 1999 Apr 1;340(13):988-93. | PubMed | Abdelfattah, M.H., Rashed, M.A., Elfakhry, A.A., Soliman, M.A., Shiha, G.E.. Endoscopic variceal ligation versus pharmacologic treatment for primary prophylaxis of variceal bleeding: a randomised study. Journal of Hepatology. 2006;44:S83-S83. | CrossRef |
Abdelfattah, M.H., Rashed, M.A., Elfakhry, A.A., Soliman, M.A., Shiha, G.E.. Endoscopic variceal ligation versus pharmacologic treatment for primary prophylaxis of variceal bleeding: a randomised study. Journal of Hepatology. 2006;44:S83-S83. | CrossRef | Abulfutuh, AR, Morsy, M, Solyman, AEG. Study of variceal band ligation, propranolol and isosorbide mononitrate in the prevention of the first variceal bleeding. Gastroenterology. 2003;124(4):A780-A780. | CrossRef |
Abulfutuh, AR, Morsy, M, Solyman, AEG. Study of variceal band ligation, propranolol and isosorbide mononitrate in the prevention of the first variceal bleeding. Gastroenterology. 2003;124(4):A780-A780. | CrossRef | Pérez-Ayuso RM, Valderrama S, Espinoza M, Rollán A, Sánchez R, Otarola F, et al. Endoscopic band ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhotic patients with high risk esophageal varices. Ann Hepatol. 2010 Jan-Mar;9(1):15-22. | PubMed |
Pérez-Ayuso RM, Valderrama S, Espinoza M, Rollán A, Sánchez R, Otarola F, et al. Endoscopic band ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhotic patients with high risk esophageal varices. Ann Hepatol. 2010 Jan-Mar;9(1):15-22. | PubMed | Gill M, Sattar S, Khokhar N. Outcomes of endoscopic variceal band ligation versus pharmacological treatment with non selective beta blocker for primary prophylaxis of variceal bleed. Gut. 2006;55:A308.
Gill M, Sattar S, Khokhar N. Outcomes of endoscopic variceal band ligation versus pharmacological treatment with non selective beta blocker for primary prophylaxis of variceal bleed. Gut. 2006;55:A308.  de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015 Sep;63(3):743-52. | CrossRef | PubMed |
de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015 Sep;63(3):743-52. | CrossRef | PubMed | Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, et al. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015 Nov;64(11):1680-704. | CrossRef | PubMed |
Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, et al. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015 Nov;64(11):1680-704. | CrossRef | PubMed | Endoscopic Band Ligation (EBL) Versus Propranolol for Primary Prophylaxis of Variceal Bleeding 2009 [on line]. | Link |
Endoscopic Band Ligation (EBL) Versus Propranolol for Primary Prophylaxis of Variceal Bleeding 2009 [on line]. | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








