Key Words: medicine family, family health, health, primary health care strategy
Abstract
Policies that generated designs health systems in Brazil have had a high participation of civil society. This is the case of the Family Health Strategy, based on the basic principles of the Health System of Brazil (SUS): universality, equity and integration, in the context of decentralization and social control of management. In this review are disclosed milestones HSB and its institutional mission, delving into what is meant by family health, describing how family medicine and community and family health have been a strategy to provide primary health care to all.
Conceptual Guideline
In most Latin-America’s countries policies have been developed in order to change structures and processes by which health system were delivered with the aim of improving performance, as well as health indicators. The most widespread measures were discussed and developed within the influential World Bank (1993) World Development Report (WDR). ‘Typically, reform includes strategies for decentralization, participation, basic packages of care, financing through increased cost-sharing or privatization and improved information systems’1. This has influenced the creation of the Brazilian National Health System (Sistema Unico de Saúde – Unified Health System) during the 80’s which has essentially reoriented the model of health care in Brazil. However, within this turmoil democratization of Brazil, the civil society has driven much the health sector reform rather than governments, political parties, or even international organizations2.
For the primary health care and Family medicine the apogee of Brazilian health reform was the adoption of “Family Health Strategy”. This strategy was strongly influenced by Alma-Ata declaration and Family Medicine experiences already running in the country. This process of conception was based on the crosscutting axes of universality, integration and equity, in a context of decentralization and social control of management, which are the basic principles of SUS, as laid out in constitutional and infra-constitutional legislation.
Milestones of the Unified Health System
- Sanitary reform movement of 80`s – social movement after 20 years of militarism.
- 1988 Constitution – Health as a citizen right.
- Health Laws: general directions (19 September 1990) and social control (28 December 1990).
- Central purpose: universal health care provided for every citizen.
- Access should be: Universal, integrated and comprehensive.
The expansion and improvement of primary health care, according to the Family Health Strategy, comprise a set of policy priorities put forward by the Ministry of Health and approved by the National Health Council. This conception supersedes the former proposal, which was focused exclusively on disease, and has been developed using democratic and participatory managerial and sanitary practices.
The Primary Health Care in Brazil is structured following the international conception having as its bases: access, comprehensiveness, continuity and coordination3. By clearly demarcating their users, the Family Health teams have managed to establish a link with the general public, making it possible for the professionals involved to commit themselves and to share responsibility with the users, family and the community. The challenge is to broaden the scope of these activities, with a view to more effective care, whereby Family Health is understood as the principal strategy for change, fully integrated into the overall context of re-organization of the health system.
Management
The Department of Primary Health Care (DAB), which is linked to the Health Care Secretariat of the Ministry of Health, has as its institutional mission the management of this policy at the federal level of SUS. This policy is implemented in partnership with the States and the municipalities. PHC Department is also responsible for elaborating mechanisms of control and evaluation of the program, for providing technical assistance to the other levels of management (states and municipalities), and for implementing and organizing the Family Health Strategy and Primary Health Care actions.
Family Health
Family Health is understood as a strategy for reorienting the health care model and is put into practice by teams formed by a cast of professionals working in primary health units. The health teams are responsible for supervising a set number of families in a specific geographical area. The teams undertake their work involving health promotion, prevention, recovery and rehabilitation, following more common illnesses and injuries, and maintaining the state of health of the community. The responsibility for a territory and for accompanying the families gives rise to the need to go beyond the traditional way of care focused only in illness4.
The Family Health Strategy is a dynamic project within the SUS, brought about by the historic evolution and organization of the health system in Brazil. The speed of expansion of Family Health is the evidence that State and municipal health care managers are in accordance to its principles. As a structural strategy within the health systems, Family Health has set off an important movement which aims to reorder the SUS care model. It seeks to rationalize the use of higher levels of care and has had a positive impact on the principal health indicators in the populations served by the family health teams.
These are the six main points for Primary Health Care (PHC) change in Brazil5:
- Definition of a national standard Family Health Team and its essential functions, integrated to a larger health network.
- Definition of responsibilities for each government level in PHC management.
- Changes in funding and growth of budget provisions for PHC.
- Development of monitoring and evaluation systems.
- Support from municipality managers and users.
- Positive outcomes and growth in political importance of PHC.
Health Teams
The work of the Family Health teams is the key plank in the constant effort to communicate and exchange experience and knowledge within team members and within them and the Community Health Workers. The Health Teams are composed of at least one Family and Community Doctor, a Nurse, a Nurse Assistant and four to twelve Community Health Workers. The extended groups include a Dentist and Dental Assistant2.
Each team is assigned to a defined geographical area and is responsible for about 3.000 people (maximum 4.000). They must visit households and do have to understand social processes and conditions in the areas under their responsibility. The teams work together on clinical care, public health, health promotion, and social issues.
Further features include: establishing ties of commitment and joint responsibility with the local population; encouraging communities to organize themselves to oversee health services and action; to use information systems for monitoring and decision-making; to operate through partnerships with various sectors of society and institutions looking for ways to intervene in situations that lie beyond the specific scope of the health sector, but nevertheless may have an impact on the living conditions and health of individuals, families and the community.
The Family Medicine and Family Health Strategy History in Brazil
The Family and Community Medicine in Brazil started its development in the middle of 70’s, even before Alma Ata Conference, when took place the tree first residences in this specialty, in Rio Grande do Sul, Rio de Janeiro and Pernambuco. These experiences were very important to bring the discussion about Primary Health Care in a new approach, out of vertical programs focused in diseases that were very strong at that moment6.
In 1981 was founded the Brazilian Society of Family and Community Medicine, at that time with the name of Brazilian Society of General and Communitarian Medicine, name that prevailed until 2001. In the 80’s and early 90’s the SBMFC struggled to stay active in national scenery with little or no incentive from the government to develop Primary Health Care. This panorama changed abruptly with the creation of the Family Health Program that was strongly influenced by some of the Family and Community Medicine experiences happening in Brazil at that moment. Nowadays, Brazil count with more than 190 residence programs in Family and Community Medicine.
The Family Health proposal started to be developed in Brazil in the early 90’s after almost 3 years of implementation of the Community Health Workers in some municipalities. The government was planning a way to put in action all the principles of the Brazilian Health System written in the national constitution in 1988, the implementation of this proposal should be an answer to the country’s health necessities. The proposal took shape as a Program, and the first teams started to work in twelve cities in 1994 under the name of Family Health Program teams4.
These teams in its majority succeeded, and other cities started to implement new teams in the following years, but the program suffered to take off in numbers of teams due to the bureaucratic form of to finance the program in the early years. The municipality at these time had to formulate an annual proposal to the Ministry appointing its needs and how many teams wanted to implement or maintain, this proposal had to be analyzed by the Ministry before to the parts celebrate an agreement and the resources start to be transferred. All this process usually took time and demanded a big effort to all parts involved, delays were common in the transfer due this process. In this regard, some municipalities choose not to implement new teams or even to discontinue the program, but still with these problems the country had 2054 teams working at July of 1998 with a big popular and political acceptance.
In 1998 the Ministry formulated a new mechanism to transfer Primary Health Care resources to the municipalities. The Federal government created the Fixed Basic Care Fund and the Variable Basic Care Fund to ensure the flow of money from the federal level to the municipal level, and stopped payment fee-for-service in PHC, this money afford a broad package of primary health care services that have to be delivered to the community by municipalities, and can’t be used for other actions non related to PHC.
The Fixed Basic Care Fund was calculated per capita and transferred to all municipalities independent to the actions performed, the Variable Basic Care Fund was action dependant and was calculated with the national data basis system’s information each month, whit a fixed amount per action implemented (Family Health Teams, Community Health Workers and Dental Health Teams)4.
The financing change on PHC increased the pace of expansion of family health teams all over the country, as shown in the figure below.
Figure 1. Family Health National Coverage (1998-2008). Source. System Info Basic Care.
Despite the huge expansion of health teams, the government analyzed this growth and saw that still had to develop new financial criteria to keep improving the PHC in some poor rural areas and particularly in the Amazon region. In attempt to improve this situation, in 2004 the Brazilian Government had then a new distribution criteria of funding for the Family Health Teams working in municipalities with less than 50.000 inhabitants in the Amazon or less than 30.000 inhabitants and Human Development Index (HDI) below 0,7 in any region of the country. These municipalities started to receive from the federal government 50% bonus of the normal federal financial investment for each team under their responsibility. In addition, in April 2006 the Federal Government adopt the same policy for teams working in “quilombolas” areas and agrarian reform settlement areas. These communities, Quilombolas (formed by descendants from black slaves) and communities living in areas of agrarian reform settlement have had historically less access to governmental health actions7.
This new funding policy for these areas resulted in a significant enhance of health access to these populations, as a result of growth in the number of Family Health Teams, as showed in the down table:
Table I. Number of teams working (2006-2008). Source. System Info Basic Care.
In 2006 the Ministry formulated in union with the States and Municipalities the National Primary Health Care Policy, which brought a new political endorsement for PHC in Brazil and reaffirmed the Family Health as a national strategy, changing its name from Family Health Program to Family Health Strategy, what gave to it a more stable status5.
Nowadays, Brazil has more than 33.420 Family Health Teams working all over the country, which represent a national coverage superior to 54%. The teams work linked to more than 255.000 Community Health Workers and 22.000 Dental Health Teams. It means that the strategies counting together with more than 350.000 workers. The consequence is that the PHC strategy in Brazil represented more than a huge advance in terms of health quality, but also in terms of social inclusion for many families, considering that usually the common profile of the Community Health Agents were women with no previous occupation or salary.
Figure 2. Family health workers (August 2012). Source. System Info Basic Care.
It’s very important to spot that the growth in term of population coverage was followed for an increase in the federal expenditure for PHC, and what made possible to negotiate internally in the govern this increment were the good results achieved and the popular recognition of the strategy. The federal government increased the financial resources for PHC in a rate higher than 300% in the last 10 years as exposed in the figure below, for 2009 were reserved about 5 billion of US dollars to finance PHC action in municipality level.
Some results of Family Health Strategy after 18 years
After 18 years from the Family Health Strategy implementation, it has good results expressed in national and international studies. For example, for non-communicable diseases the declines were primarily for cardiovascular and chronic respiratory diseases, which has been associated with the successful implementation of health policies that lead to decreases in smoking and the expansion of access to primary health care6. An overview in trends of infant mortality in Brazil over the three decades shows a steady decline rate of 5.5/year in 1980s and 1990s following by 4.4/year from 2000 onwards reaching in 2008 an average of 20% infant mortality rate8.
What follows are some studies which have revealed positive effects of the Family Health Strategy are quoted below:
Infant Mortality
- The study “Going to scale with community-based primary care: An analysis of the family health program and infant mortality in Brazil, 1999–2004” showed that, controlling for other health determinants, a 10 percent increase in Family Health Strategy coverage was associated with a 0.45 percent decrease in IMR, a 0.6 percent decline in post neonatal mortality, and a 1 percent decline in diarrhea mortality (p<0.05)10.
- A study publicized in the American Journal of Public Health demonstrate that Family Health Strategy contributed to a decrease in Infant Mortality Rates in Brazil, and appointed that the effects were stronger in areas with the higher Infant Mortality Rates and lower Human Development Index before the program was initiated, suggesting that the Family Health Strategy can contribute to decreases in social inequalities in health in Brazil11.
- A study about the evaluation of the impact of the Family Health Strategy on infant mortality in Brazil, showed that FHS expansion, along with other socioeconomic developments, were consistently associated with reductions in infant mortality12.
- Brazil was present in the cluster that obtained the best results inside the “Millennium Development Goals” priority countries analyzed for Infant Mortality Rate, and appointed that there are indicators that this can be attributed to two governmental actions: The Family Health Strategy (in special to the Community Health Workers), and to the governmental program of direct income transfer called “Bolsa Família” that have special requirements linked to health accompaniment13.
Infant Mortality and Social Development
- A new study showed “consistent effects of the program on reductions in mortality throughout the age distribution, but mainly at earlier ages. Municipalities in the poorest regions of the country benefit particularly from the program. For these regions, implementation of the program is also robustly associated with increased labor supply of adults, reduced fertility, and increased schooling. Evidence suggests that the Family Health Program is a highly cost-effective tool for improving health in poor areas”14.
Avoidable Hospitalizations
The study called “Primary Care and Avoidable Hospitalizations: Evidence From Brazil”, demonstrates that expansions of the Family Health Strategy were associated with reductions in hospitalizations for diabetes mellitus and respiratory problems, and the Community Health Workers expansions were associated with reductions in circulatory conditions hospitalizations. Strategy coverage may have contributed to an estimated 126 000 fewer hospitalizations between 1999 and 2002, corresponding to potential savings of 63 million US dollars15.
Elderly
A study demonstrated best results for Family Health Services when compared with other kind of Primary Care Services in the same municipalities in Brazil in terms of health care for elderly people16.
User Satisfaction
A study demonstrates the good evaluation of the Family Health for Users, Professionals and Managers17.
Offer, access and utilization of health services
A study demonstrated best results for Family Health Services when compared with other kind of Primary Care Services in the same municipalities in Brazil in terms of offer, access and utilization of the services18.
Implementation of the Strategy
The study “The degree of implementation of the Family Health Program and social indicators”, covering 125 municipalities in Brazil, found a interesting secondary result, that no correlation has been observed among the FHS implementation and the political group at local administration, showing that the decision to implement the strategy seems to be independent from the ideological wing in the government19.
Conclusions
The Family and Community Medicine in Brazil it is in a good pace of development following the Family Health Strategy growing. The development of the strategy was a partnership between federal, state and municipal government with a strong popular support and a strategic contribution of scientific societies like Brazilian Society of Family and Community Medicine. The PHC strategy demonstrates to be adaptable and replicable, whereas it is implemented all over the country even Brazil being a big nation with large differences between its regions. The initiative has more than eighteen years, having gone through five national elections, four different presidents and eleven different Health Ministers, and after all, it is still strong and counts with a large public acceptance, showing that besides political changes PHC can grow and bring good results for the population. Brazil can be inspirational for other countries to tackle their own health problems as long as there is high level of engagement by civil society in this direction of framing health as political right and organizing their system through a strong primary health strategy9.

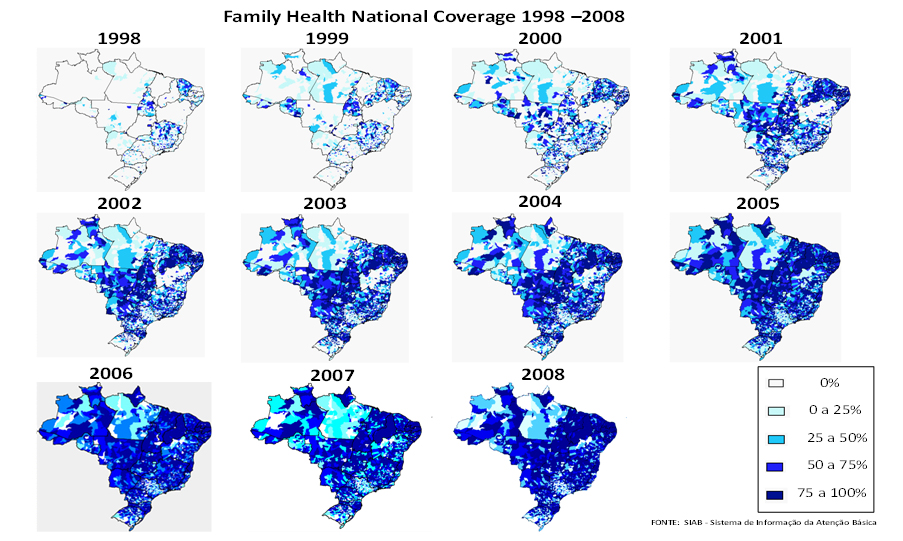 Figure 1. Family Health National Coverage (1998-2008). Source. System Info Basic Care.
Figure 1. Family Health National Coverage (1998-2008). Source. System Info Basic Care.

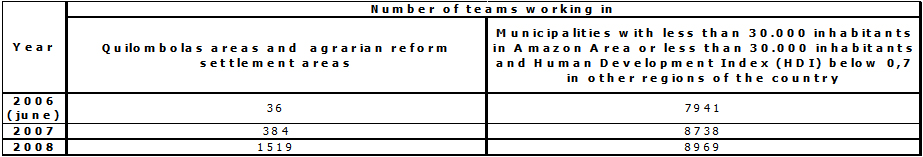 Table I. Number of teams working (2006-2008). Source. System Info Basic Care.
Table I. Number of teams working (2006-2008). Source. System Info Basic Care.

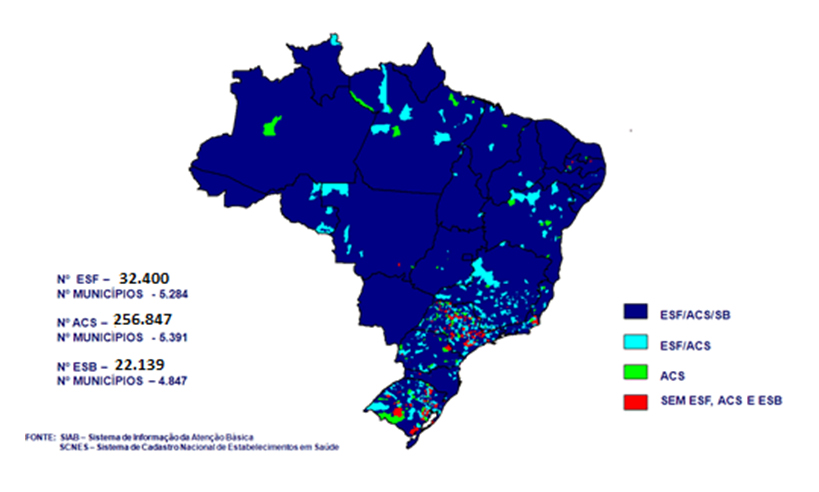 Figure 2. Family health workers (August 2012). Source. System Info Basic Care.
Figure 2. Family health workers (August 2012). Source. System Info Basic Care.

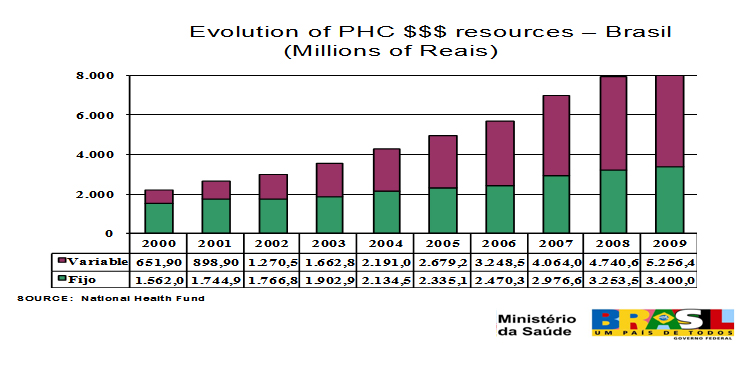 Table II. Family Health Strategy Brazil (2000 – 2009). Source. Financial Resources Allocated by the Federal Government.
Table II. Family Health Strategy Brazil (2000 – 2009). Source. Financial Resources Allocated by the Federal Government.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Las políticas que generaron los diseños de los sistemas de salud en Brasil han tenido una alta participación de la sociedad civil. Es el caso de la Estrategia de Salud Familiar, basada en los principios básicos del Sistema Único de Salud de Brasil (SUS): universalidad, integración y equidad, en un contexto de descentralización y control social de la gestión. En esta revisión se dan a conocer los hitos del SUS y su misión institucional, profundizando en lo que se entiende por salud familiar, describiendo como la medicina familiar y comunitaria y la salud de la familia han sido una estrategia para ofrecer atención primaria de salud para todos.


Submission date: 16/11/2012
Acceptance date: 30/11/2012
Publication date: 1/1/2013
Origin: commissioned
Type of review: peer-reviewed by 1 reviewer, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Atkinson S. Political cultures, health systems and health policy. Soc Sci Med. 2002 Jul;55(1):113-24. | CrossRef | PubMed |
- Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011 May 21;377(9779):1778-97. Epub 2011 May 9. | CrossRef | PubMed |
- Starfield B. Atenção Primária: equilíbrio entre necessidades de saúde, serviços e tecnologia. 1a ed. Brasília: UNESCO, Ministério Da Saúde, 2002. | Link |
- Sampaio FR. The Brazilian health system: highlighting the primary health care reform. IJPH. 2010;7(4):359-68. | Link |
- Brasil, Ministério da Saúde, Departamento de Atenção Básica. Política nacional de atenção. Brasília: Ministério da Saúde, 2006. Série Pactos pela Saúde Vol.4. | Link |
- Gusso G, Lopes JM. Tratado de medicina de família e comunidade. Princípios, formação e prática. Porto Alegre: ARTMED, 2012.
- Victora CG, Barreto ML, Leal C, Monteiro CA, Schmidt MI, Paim J, et al. Health conditions and health-policy innovations in Brazil: the way forward. Lancet. 2011 Jun 11;377(9782):2042-53. Epub 2011 May 9. | CrossRef | PubMed |
- Victora CG, Aquino EM, do Carmo M, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: progress and challenges. Lancet. 2011 May 28;377(9780):1863-76. Epub 2011 May 9. | CrossRef | PubMed |
- Buss P. Brazil: structuring cooperation for health. Lancet. 2011 May 21;377(9779):1722-3. Epub 2011 May 9. | CrossRef | PubMed |
- Macinko J, Marinho de Souza Mde F, Guanais FC, da Silva Simões CC. Going to scale with community-based primary care: an analysis of the family health program and infant mortality in Brazil, 1999-2004. Soc Sci Med. 2007 Nov;65(10):2070-80. Epub 2007 Aug 8. | PubMed |
- Barreto ML, Aquino R. Recent positive developments in the Brazilian health system. Am J Public Health. 2009 Jan;99(1):8. Epub 2008 Nov 13. | CrossRef | PubMed | PMC |
- Macinko J, Guanais FC, de Fátima M, de Souza M. Evaluation of the impact of the Family Health Program on infant mortality in Brazil, 1990-2002. J Epidemiol Community Health. 2006 Jan;60(1):13-9. | CrossRef | PubMed | PMC |
- Murray CJ, Laakso T, Shibuya K, Hill K, Lopez AD. Can we achieve Millennium Development Goal 4? New analysis of country trends and forecasts of under-5 mortality to 2015. Lancet. 2007 Sep 22;370(9592):1040-54. | CrossRef | PubMed |
- Rocha R, Soares RR. Evaluating the impact of community based health interventions: evidence from Brazil's Family Health Program. Bonn, Germany: IZA, 2009. Discussion Paper No. 4119, Apr 2009. | Link |
- Guanais F, Macinko J. Primary care and avoidable hospitalizations: evidence from Brazil. J Ambul Care Manage. 2009 Apr-Jun;32(2):115-22. | PubMed |
- Piccini RX, Facchini LA, Tomasi E, Thumé E, Silva D, Vinholes F, et al. Necessidades de saúde comuns aos idosos: efetividade na oferta e utilização em atenção básica à saúde. Ciênc Saúde Coletiva. 2006 Jul/Set;11(3):657-667. | CrossRef |
- Elias PE, Whitake C, Góis MC, Cohn A, Kishima V, Escrivão A, et al. Atenção Básica em Saúde: comparação entre PSF e UBS por estrato de exclusão social no município de São Paulo. Ciênc Saúde Coletiva. 2006 Jul /Set;11(3):633-641. | CrossRef |
- Facchini LA, Piccini RX, Tomasi E, Thumé E, Silva D, Vinholes F, et al. Desempenho do PSF no Sul e no nordeste do Brasil: avaliação institucional e epidemiológica da Atenção Básica à Saúde. Ciênc Saúde Coletiva. 2006 Jul /Set;11(3):669-681. | CrossRef |
- Henrique F, Calvo MC. Grau de implantação do Programa Saúde da Família e indicadores sociais. Ciênc Saúde Coletiva. 2009 Set/Oct;14(suppl.1):1359-1365. | CrossRef |
 Atkinson S. Political cultures, health systems and health policy. Soc Sci Med. 2002 Jul;55(1):113-24. | CrossRef | PubMed |
Atkinson S. Political cultures, health systems and health policy. Soc Sci Med. 2002 Jul;55(1):113-24. | CrossRef | PubMed | Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011 May 21;377(9779):1778-97. Epub 2011 May 9. | CrossRef | PubMed |
Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011 May 21;377(9779):1778-97. Epub 2011 May 9. | CrossRef | PubMed | Starfield B. Atenção Primária: equilíbrio entre necessidades de saúde, serviços e tecnologia. 1a ed. Brasília: UNESCO, Ministério Da Saúde, 2002. | Link |
Starfield B. Atenção Primária: equilíbrio entre necessidades de saúde, serviços e tecnologia. 1a ed. Brasília: UNESCO, Ministério Da Saúde, 2002. | Link | Sampaio FR. The Brazilian health system: highlighting the primary health care reform. IJPH. 2010;7(4):359-68. | Link |
Sampaio FR. The Brazilian health system: highlighting the primary health care reform. IJPH. 2010;7(4):359-68. | Link | Brasil, Ministério da Saúde, Departamento de Atenção Básica. Política nacional de atenção. Brasília: Ministério da Saúde, 2006. Série Pactos pela Saúde Vol.4. | Link |
Brasil, Ministério da Saúde, Departamento de Atenção Básica. Política nacional de atenção. Brasília: Ministério da Saúde, 2006. Série Pactos pela Saúde Vol.4. | Link | Gusso G, Lopes JM. Tratado de medicina de família e comunidade. Princípios, formação e prática. Porto Alegre: ARTMED, 2012.
Gusso G, Lopes JM. Tratado de medicina de família e comunidade. Princípios, formação e prática. Porto Alegre: ARTMED, 2012.  Victora CG, Barreto ML, Leal C, Monteiro CA, Schmidt MI, Paim J, et al. Health conditions and health-policy innovations in Brazil: the way forward. Lancet. 2011 Jun 11;377(9782):2042-53. Epub 2011 May 9. | CrossRef | PubMed |
Victora CG, Barreto ML, Leal C, Monteiro CA, Schmidt MI, Paim J, et al. Health conditions and health-policy innovations in Brazil: the way forward. Lancet. 2011 Jun 11;377(9782):2042-53. Epub 2011 May 9. | CrossRef | PubMed | Victora CG, Aquino EM, do Carmo M, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: progress and challenges. Lancet. 2011 May 28;377(9780):1863-76. Epub 2011 May 9. | CrossRef | PubMed |
Victora CG, Aquino EM, do Carmo M, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: progress and challenges. Lancet. 2011 May 28;377(9780):1863-76. Epub 2011 May 9. | CrossRef | PubMed | Buss P. Brazil: structuring cooperation for health. Lancet. 2011 May 21;377(9779):1722-3. Epub 2011 May 9. | CrossRef | PubMed |
Buss P. Brazil: structuring cooperation for health. Lancet. 2011 May 21;377(9779):1722-3. Epub 2011 May 9. | CrossRef | PubMed | Macinko J, Marinho de Souza Mde F, Guanais FC, da Silva Simões CC. Going to scale with community-based primary care: an analysis of the family health program and infant mortality in Brazil, 1999-2004. Soc Sci Med. 2007 Nov;65(10):2070-80. Epub 2007 Aug 8. | PubMed |
Macinko J, Marinho de Souza Mde F, Guanais FC, da Silva Simões CC. Going to scale with community-based primary care: an analysis of the family health program and infant mortality in Brazil, 1999-2004. Soc Sci Med. 2007 Nov;65(10):2070-80. Epub 2007 Aug 8. | PubMed | Barreto ML, Aquino R. Recent positive developments in the Brazilian health system. Am J Public Health. 2009 Jan;99(1):8. Epub 2008 Nov 13. | CrossRef | PubMed | PMC |
Barreto ML, Aquino R. Recent positive developments in the Brazilian health system. Am J Public Health. 2009 Jan;99(1):8. Epub 2008 Nov 13. | CrossRef | PubMed | PMC | Macinko J, Guanais FC, de Fátima M, de Souza M. Evaluation of the impact of the Family Health Program on infant mortality in Brazil, 1990-2002. J Epidemiol Community Health. 2006 Jan;60(1):13-9. | CrossRef | PubMed | PMC |
Macinko J, Guanais FC, de Fátima M, de Souza M. Evaluation of the impact of the Family Health Program on infant mortality in Brazil, 1990-2002. J Epidemiol Community Health. 2006 Jan;60(1):13-9. | CrossRef | PubMed | PMC | Murray CJ, Laakso T, Shibuya K, Hill K, Lopez AD. Can we achieve Millennium Development Goal 4? New analysis of country trends and forecasts of under-5 mortality to 2015. Lancet. 2007 Sep 22;370(9592):1040-54. | CrossRef | PubMed |
Murray CJ, Laakso T, Shibuya K, Hill K, Lopez AD. Can we achieve Millennium Development Goal 4? New analysis of country trends and forecasts of under-5 mortality to 2015. Lancet. 2007 Sep 22;370(9592):1040-54. | CrossRef | PubMed | Rocha R, Soares RR. Evaluating the impact of community based health interventions: evidence from Brazil's Family Health Program. Bonn, Germany: IZA, 2009. Discussion Paper No. 4119, Apr 2009. | Link |
Rocha R, Soares RR. Evaluating the impact of community based health interventions: evidence from Brazil's Family Health Program. Bonn, Germany: IZA, 2009. Discussion Paper No. 4119, Apr 2009. | Link | Guanais F, Macinko J. Primary care and avoidable hospitalizations: evidence from Brazil. J Ambul Care Manage. 2009 Apr-Jun;32(2):115-22. | PubMed |
Guanais F, Macinko J. Primary care and avoidable hospitalizations: evidence from Brazil. J Ambul Care Manage. 2009 Apr-Jun;32(2):115-22. | PubMed | Piccini RX, Facchini LA, Tomasi E, Thumé E, Silva D, Vinholes F, et al. Necessidades de saúde comuns aos idosos: efetividade na oferta e utilização em atenção básica à saúde. Ciênc Saúde Coletiva. 2006 Jul/Set;11(3):657-667. | CrossRef |
Piccini RX, Facchini LA, Tomasi E, Thumé E, Silva D, Vinholes F, et al. Necessidades de saúde comuns aos idosos: efetividade na oferta e utilização em atenção básica à saúde. Ciênc Saúde Coletiva. 2006 Jul/Set;11(3):657-667. | CrossRef | Elias PE, Whitake C, Góis MC, Cohn A, Kishima V, Escrivão A, et al. Atenção Básica em Saúde: comparação entre PSF e UBS por estrato de exclusão social no município de São Paulo. Ciênc Saúde Coletiva. 2006 Jul /Set;11(3):633-641. | CrossRef |
Elias PE, Whitake C, Góis MC, Cohn A, Kishima V, Escrivão A, et al. Atenção Básica em Saúde: comparação entre PSF e UBS por estrato de exclusão social no município de São Paulo. Ciênc Saúde Coletiva. 2006 Jul /Set;11(3):633-641. | CrossRef | Facchini LA, Piccini RX, Tomasi E, Thumé E, Silva D, Vinholes F, et al. Desempenho do PSF no Sul e no nordeste do Brasil: avaliação institucional e epidemiológica da Atenção Básica à Saúde. Ciênc Saúde Coletiva. 2006 Jul /Set;11(3):669-681. | CrossRef |
Facchini LA, Piccini RX, Tomasi E, Thumé E, Silva D, Vinholes F, et al. Desempenho do PSF no Sul e no nordeste do Brasil: avaliação institucional e epidemiológica da Atenção Básica à Saúde. Ciênc Saúde Coletiva. 2006 Jul /Set;11(3):669-681. | CrossRef | Henrique F, Calvo MC. Grau de implantação do Programa Saúde da Família e indicadores sociais. Ciênc Saúde Coletiva. 2009 Set/Oct;14(suppl.1):1359-1365. | CrossRef |
Henrique F, Calvo MC. Grau de implantação do Programa Saúde da Família e indicadores sociais. Ciênc Saúde Coletiva. 2009 Set/Oct;14(suppl.1):1359-1365. | CrossRef |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








