Key Words: Occupational Health, Occupational Health Services/organization & administration, Workplace/organization & administration, Psychosocial Risks, Global Evidence Mapping
Abstract
Objective
To identify preventive practices for psychosocial risks in Ibero-American health centers, including gaps in evidence, and to synthesize effectiveness according to dimensions and level of intervention.
Methods
Design: a global evidence mapping type systematic review. Data sources: Cochrane Central Register of Controlled Trials, Health Systems Evidence, The Campbell Collaboration, PubMed, BioMed Central, CINAHL, EMBASE, Lilacs, and Health Evidence Portal. Review methods: Ad hoc descriptors were used to identify randomized controlled trials and other types of studies. The search was done between January 2003 and March 2020, limited to the English, Portuguese, and Spanish. The PRISMA-P protocol was applied to register the synthesis of the included studies. The quality of the evidence was evaluated according to the GRADE protocol and by three external evaluators.
Results
A total of 8959 studies were identified, and, after screening and eligibility assessment, 18 studies were included in the systematic review, involving 1777 workers from 176 health centers in Spain, Portugal, Mexico, Nicaragua, Colombia, Brazil, Peru, and Argentina. Half of the included studies are randomized controlled trials; 37.2% of the included studies were deemed of moderate quality, while 18.7% were of high quality.
Conclusions
Preventive practices with strong evidence correspond to policies that improve the working conditions of night hospital work. We found low-quality evidence in six preventive dimensions for the practices based on multi-component interventions. We found evidence gaps in five domains of preventive interventions for psychosocial risks.
Main messages
|
Introduction
Occupational health has been considered the basic element of sustainable development, and the healthy, motivated, and productive worker, the key agent for socioeconomic development[1]. Thus, the number of occupational studies has been growing and diversifying[2],[3]. Because of the changing nature of work and the existence of austerity policies, currently, there are various inequities and demands, such as organizational competitiveness versus cost reduction[4], which have generated the appearance of psychosocial risks at work; this is the result of the interaction between organizational elements, work management, and environmental conditions, but also of the interaction between the functions and the needs of the workers[5].
This polarity has created a link between the work environment and the worker's bio-psychosocial health[6], with a greater impact on workers of the health sector, which by the very nature of their functions are more vulnerable[6],[7]. The impact of the work environment on workers' health also affects job performance[8]. Consequently, interventions aimed at improving safety and occupational health management may be more effective in the healthcare work environment than on individuals alone[9]. Such interventions could represent a competitive advantage because the concept of social responsibility to promote the benefits of prevention culture is of use to institutional performance, thus avoiding negative repercussions on health[5],[10].
Regarding psychosocial risks in healthcare workers in the Ibero-American context, in Santiago de Chile, about a third of the workers in three primary care health centers were exposed to psychosocial risks that negatively impacted their health[11]. In Guadalajara, Mexico, the prevalence of negative psychosocial factors was 32.2% (128/397)[12]. In various clinics of Buenos Aires and La Plata, Argentina, over 50% of the workers perceived high demands and pressure to increase their work rhythm[13], and 25% of social workers experienced high emotional pressure[14]. Similarly, in Cali, Colombia, the greatest negative impact was high emotional-labor demand, with high-risk levels in 55.8% (87/156) of the workers[15]. In São Paulo, Brazil, 45% (195/433) of workers performed demanding tasks with low levels of social support from colleagues and supervisors[16].
In Lima, Peru, occupational dissatisfaction related to culture, organizational environment, tasks, and interpersonal relationships affected up to 26.1% (48/184) of workers[17]. In Valencia, Spain, there was also a high level of psychological demand in 74.3% (81/109) of workers, with a perception of job insecurity in 65.1% (71/109) of the cases; there was also a lack of social support and low quality of leadership in 46% (50/109), and small possibilities of professional development in 36.8% (39/109) of the cases[18]. Finally, in Porto, Portugal, given the high levels of psychosocial risks at work in emergency services, coping was dysfunctional in 32.6% (118/362) of workers[19].
Because the preventive strategies in the organizational context of psychosocial risks in healthcare workers are unclear[19], because of the high cost-effectiveness ratio of risk prevention (1: 4), and because of potential health benefits and improved productivity[5], it is necessary to identify and assess the available evidence according to the dimensions of the intervention with the following considerations:
- The evidence should be based on economic, political, and organizational aspects and the specifications of job descriptions[20].
- The evidence should involve specific factors of the organizational environment and culture, including working conditions[21].
Framework
The formulation of evidence-based health policies and programs constitutes good health practices, providing support to politicians and managers to improve decision-making with transparency, making it possible to assess interventions' effects and benefits[22]. The references that establish a link between business management and the worker's health state are 1) the model known as "labor demand-resources" and 2) the specific model of managerial behavior. According to these models, psychosocial risks at work represent a condition of the work process directed to either exhaustion or commitment. When these risks involve excessive physical and psychological demands, they lead to exhaustion[23]. In contrast, access to resources (e.g., support and control) encourages commitment through motivation or recognition[23]. For this reason, the leadership styles adopted by managers can significantly influence psychosocial health[16],[24]. For example, transformational leadership is often related to cognitive components[25] and authoritarian leadership to stress[9].
Recent studies show that psychosocial health in healthcare workers is more affected by tangible manifestations, such as autonomy support behavior and workers' attitude[16],[26],[27]. It has been reported that everyday behavior can have a significant impact on psychosocial health[28]. Also, psychosocial health risks may be greater in situations in which the work team is fragmented, does not have social support[5],[29], or when staff turnover is very high[30]. Finally, the managerial role is decisive in the reduction of psychosocial risks at work[9].
Three levels of intervention are taken into consideration for the prevention of psychosocial risks in healthcare workers:
- Training on skills for the resolution of interpersonal problems, and the improvement of communication and cognitive skills, including the prevention of stress risk factors[16],[31];
- Improvement of job skills, working conditions, and the promotion of physical activity at work[31];
- Multi-component interventions, the lowest level of which is awareness-raising, followed by training. The most profound and comprehensive level of multi-component interventions is applying occupational health and safety management policies, which involves organizational changes and the design of job positions[24],[31].
In developed countries, academic reports related to the strategies for reducing psychosocial risks and the promotion of psychosocial health[24] correspond mainly to the industry, public management, education, transport and storage, waste management, production, art, and entertainment[9]. This study[9] proposes reaching significant conclusions by exploring preventive practices for psychosocial risks in Ibero-American healthcare workers. These conclusions should be based on randomized controlled trials and multi-component interventions[32], aim to promote institutional changes and be applied to preventive practices in Brazilian maternal health[33]. The outcomes regarding the interaction of multistage educational meetings were moderate; in contrast, the outcomes were very low and were of short duration[32] for interaction practices for institutional changes that only included expositions or talks[32].
These low-quality results contrast with other studies, which despite being very favorable, cannot be extrapolated to the Ibero-American context[34],[35],[36],[37],[38],[39]. Specifically, the results obtained from a recent meta-analysis based on multi-component interventions do not apply to the Ibero-American context[40], although these results support the formulation of policies to improve working conditions for healthcare personnel.
On the other hand, exploring the evidence on preventive practices is relevant to establish public policies for the prevention of psychosocial risks in healthcare workers; these policies may benefit workers, employers, or managers[6],[21], because the conditions of workers are part of the social determinants of psychosocial health, and because these conditions must be improved within the framework of international guidelines on preventive interventions or practices[41],[42].
This study's objectives were to identify preventive practices for psychosocial risks in Ibero-American health centers, identify the gaps in evidence, and synthesize the effectiveness of the interventions according to their dimension and level of intervention.
We sought to answer the following questions:
- What practices allow the establishment of policies for the prevention of psychosocial risks in Ibero-American health centers?
- How are preventive practices grouped?
- What are the gaps in evidence for future lines of research?
Methods
We used global evidence mapping[43] systematic review design to identify studies on preventing psychosocial risks in healthcare workers, including evidence gaps[44].
Inclusion criteria
- We used the PICO (participants, interventions, comparisons, outcomes) question approach to assess the inclusion of studies using the PRISMA (Preferred reporting items for systematic review and meta-analysis) protocol[45]. Participants were Ibero-American health center workers (health professionals, interns, volunteers, managers, supervisors, and administrative personnel)[46]. Interventions aimed to prevent psychosocial risks in healthcare workers.
- Studies should be published studies or belong to gray literature but should have applied experimental designs (e.g., randomized controlled trials), quasi-experimental designs (before-after type or interrupted time series). We also included observational or descriptive studies.
- Experimental or quasi-experimental studies should have similar characteristics and include at least one treatment group and one control group with current, pre-, and post-intervention measurements to demonstrate the effects of preventive interventions.
- The experimental group should be constituted by healthcare workers[45].
- Psychologists or other health professionals should have led the experimental interventions.
Exclusion criteria
Subjects who were not Ibero-American healthcare workers, and studies whose interventions were not preventive or lacked a psychosocial approach, were excluded from the review.
Search strategies
- The following occupational health-related databases were consulted: Cochrane Central Register of Controlled Trials (The Cochrane Library; Cochrane Work Review Group), Health Systems Evidence (McMaster University & Cochrane Canada), and The Campbell Collaboration;
- PubMed, BioMed Central, CINAHL, EMBASE, Lilacs, and EBSCO-Host;
- Repositories of universities and web portals of international organizations, such as the World Health Organization Health Evidence Portal, Organization of American States, Pan American Health Organization, International Labor Organization, and Coordination of Aperfeiçoamento de Pessoal de Nível Superior from Brazil.
The search period was from January 2003 to March 2020. We limited the search to English, Portuguese, and Spanish languages. The following descriptors were used: "health and safety at work", "primary prevention", "clinical trial", "humans" and "healthcare"; "intervention", "health human resources", "innovation & research", and "healthcare staff". For the EMBASE database, a set of ad hoc algorithms was used.
For systematization of the information, 18 records of analysis and interpretation of studies were used according to the following factors[45]:
- Type and topic of intervention;
- Description of the evidence (method, design, phases, data collection techniques, comparison groups, baseline, scenarios, or context);
- Participants;
- Interventions (groups, number of participants, duration, sequence, characteristics);
- Quali-quantitative results; in case there were missing data, the Hedges and Olkin[47] or Morris[48] equations were applied;
- Annotations about the type of multi-component intervention, plus additional information on biases and score equivalences (Annex 1).
The quality of the evidence was evaluated according to the GRADE protocol (Grading of recommendations, assessment, development, and evaluation), which allowed us to generate summary tables of evidence for each outcome and topic of psychosocial risks at work, using the GRADEpro GDT software (Cochrane Community). Evidence was categorized as high, moderate, low, and very low quality, based on the following criteria: type of design, risk of bias (selection bias, blinding bias, and reporting bias, among other types of bias), inconsistency degree, indirect evidence, and publication bias. The factors that reduced the base quality of evidence were inadequate sample size and selection.
González and Cuadrado[50] were used as references to categorize evidence as evidence with a certainty of GRADE quality. High quality of evidence was indicated when research provided a very good indication of the probable effect and when the probability of a different effect is low. Very low quality of evidence was indicated when the research did not provide a reliable estimate of the probable effect or when the probability of an effect different than the expected was high.
Three external evaluators participated to ensure the transparency of the evidence of the studies that were included in this work (JLGM, Spain; GECG, Peru; JMRM, Brazil). External evaluators filled out the evaluation sheets based on ten evaluation criteria (suitable Kendall test: p = 0.012); they focused on three criteria: compliance with the PRISMA protocol, evaluation of the intervention, and sample size.
Results
According to the PRISMA statement checklist recommendation for the flow of information in the different phases of a systematic review[45], a total of 8959 studies were identified; 8899 of these studies corresponded to the first and second search strategy, and 60 corresponding to the third search strategy. After screening the titles and abstracts of the studies for inclusion and exclusion criteria (screening and eligibility phases, Figure 1), eighteen studies were included in the present systematic review on preventive practices for psychosocial risks at work in Ibero-American health centers. Six studies were included for a quantitative meta-analysis (which was not the subject of the present study).
Figure 1. Information flow diagram according to the PRISMA-P phases of the systematic review[45]
Studies included in the systematic review with the highest level of evidence corresponded to randomized controlled trials (50% of the studies, 9/18) from Portugal, Argentina, Spain, Puerto Rico, Mexico, and Peru. Quasi-experimental studies were 33.3% of the total (6/18); and 16.7% (3/18) were descriptive studies (Table 1). The total number of workers in 176 Ibero-American health centers was 1777. Doctors from Spain, Portugal, Mexico, Nicaragua, Puerto Rico, Brazil, Colombia, Peru, and Argentina corresponded to 34% of the total (606/1777). We highlight the participation of government workers (medical directors, managers of health centers, and heads of nursing services) with the ability to establish policies for the prevention of psychosocial risks in healthcare workspaces; these participants corresponded to 10.4 % of all healthcare workers [46] (185/1777) (Table 1).
Preventive practices for psychosocial risks in Ibero-American healthcare workers
1. Preventive practices to establish policies that improve working conditions
1a) Evidence based on the prevention of the effects of drowsiness and sleep disorders, derived from hospital shift work (nurses and doctors from different areas), indicates that workers exposed to full-spectrum bright white light (2-4 exposures of 15 minutes per night, alternating three times per nap), having two 10-minute breaks, managed to significantly reduce the effects of drowsiness compared to the control group[51],[52],[53].
Similarly, workers performing physical exercises in the morning, who applied the Health Sleep Program plus a night nap (30 minutes per shift), have decreased drowsiness effects and improved psychomotor reaction relative to the control group[54],[55],[56] (Table 2).
1b) Evidence on the promotion of occupational health based on workplace gymnastics (physical exercises at least 30 minutes per day) reveals improvement in adaptation to the emotional demands of third parties, improvement in self-perception of the state of health (the number of medical consultations increased, sleep habits improved, and fat consumption decreased), and a significant decrease in stress levels[57],[58] (Table 2).
1c) Evidence on risk prevention in workers at key organizational positions indicates that the number of adverse incidents decreases (for example, cuts or punctures with clinical instruments), and adherence to hand washing and the use of respirators increases; these changes were promoted through training that applied educational-participatory methodology[59]. Communication and debate opportunities increased, as did the formulation of solutions to work issues (Table 2).
2. Preventive practices to improve decision-making and organizational communication
2a) Evidence shows that international training programs and programs focused on strengthening responses from decision-makers and psychosocial health planners can generate positive attitudes towards financing policies for preventive interventions[60] (Table 2).
2b) Evidence extracted from multi-component interventions on the management of interpersonal conflicts, and from psychosocial training interventions for changing attitudes and behaviors in professional practice (through interactive workshops combined with other interventions), shows that interpersonal relationships improve and psychosocial occupational health is promoted [61]. In contrast, talks, presentations, or awareness visits do not generate changes because they are complex behaviors (Table 2).
3. Preventive practices to support personal and professional development
3a) Evidence on the implementation of training plans (training to develop leadership in preventive health, leadership skills, and conflict management) indicates that communication in multidisciplinary teams improves while promoting participatory techniques in preventive projects and personal development[62]. These plans also include emotional support and health innovation through continuous education (two years) for quality management and health promotion.
3b) Evidence focused on training and professional training practices for the promotion of psychosocial occupational health (through implementation and improvement of preventive and recuperative interventions from multi-component interventions) facilitate the design and validation of educational materials for primary care providers (guidelines for prevention, diagnosis, and treatment of depressive disorders) and promote randomized controlled trials[63] (Table 2).
3c) Evidence on mixed education programs (two face-to-face 5 hours sessions plus 30 hours online) for the prevention of psychosocial occupational health, with independent and collaborative learning through multifaceted interventions, shows improvement in knowledge and practical prevention skills in nurses, but no improvement in attitudes[64].
4. Preventive practices to develop leadership
In contrast to psychosocial training aimed at changing attitudes (through interactive workshops combined with other interventions that achieved substantial improvements), moderate improvement in leadership skills was achieved through training to evaluate evidence related to consulting mechanisms, participation, and work negotiation. Gains were also recorded from educational leadership training programs for prevention and management in psychosocial occupational health (according to multi-component interventions); these programs were 6-hours monthly workshops plus six accompanying monthly visits[61] (Table 2).
5. Preventive practices to establish policies related to teamwork
5a) Evidence suggests that the promotion of workers' participation in decision-making, the development of skills for teamwork[65], and the participatory management style with organizational improve group cohesion, teamwork, and decision-making in doctors. On the other hand, the promotion of leadership for teamwork, the culture of support, and the motivation for change increase the participation of multidisciplinary teams (doctors, nurses, and pharmacists), with the participation of medical personnel being the success factor[66] ( Table 2).
5b) Other evidence shows that the generation of trust, the generation of emotional support, and the improvement of the interaction in the team of workers (disaggregating the multi-component interventions but including participatory techniques and interactive mentality-changing workshops to that involve identification, care, and preventive management) optimize the effectiveness of training-awareness for behavior change and promotion of psychosocial occupational health. It should be noted that a single talk or conference does not generate any changes [61],[67],[68].
5c) The evidence focused on mixed behavior changes (multi-component interventions) shows moderate changes in complex behaviors, active participation of healthcare workers, and changes in attitude for the promotion of psychosocial health (Table 2). Mixed behavior changes were promoted through experiential workshops on healthy lifestyles, behavior modification techniques, evidence-based lectures or demonstrations, occupational gymnastics, illustrative materials, and promotional project proposals[61]. The techniques used were role-playing games (led by psychologists or social workers)[67] with 5-7 contextual interviews (30 minutes with social medical doctors), and cognitive-behavioral interventions for problem-solving and depressive reactions[68] (Tabla 2).
According to GRADE evidence (Table 2), the highest frequency of outcomes corresponds to moderate quality (37.5% of the studies, 6/16), followed by low quality (25%) (4/16) and high quality (18.8%) (3/16).
In summary, considering the number of studies[51],[52],[53],[54],[55],[56], and the quality of the evidence, type 1a interventions (Table 2) are sufficient to establish policies to improve working conditions. In contrast, for type 1b and 1c interventions (Table 2), the evidence is not enough to develop additional policies (according to the number of studies, n = 1-2). Similarly, the evidence is insufficient to support either decision-making and organizational communication, personal and professional development, or leadership (types of outcomes 2a, 2b, 3, and 4). For type 5a, 5b, and 5c interventions (Table 2), the evidence is insufficient to establish policies to promote teamwork in health centers.
Evidence gaps are linked to job design, performance evaluation and instrumentalization systems, institutional objectives, interpersonal relationships, and conflict resolution, improved organizational communication, and organizational changes in Ibero-American health centers (Table 3).
Discussion
From the preventive practices for psychosocial risks in healthcare workers identified and synthesized in this work, it becomes evident that the current trend in Latin America is to emphasize policies that improve working conditions. Of relevance are also multi-component interventions[31] linked to the promotion of teamwork and reinforcement for decision-making through training and education. In addition, awareness is promoted for the involvement of workers and the improvement of organizational communication. Finally, we corroborate that there is interest in supporting personal-professional development to improve healthcare workers' leadership skills.
The high-quality evidence showing reduced effects of drowsiness, reduced sleep disorders derived from shift hospital work[51],[52],[53], or improved psychomotor reactions[54],[55],[56] coincides with reports from developed countries[35],[36]; these reports also show that naps improved the effects of drowsiness, improved alertness-wakefulness, and improved cognitive performance. This evidence encourages government workers to establish policies that will enhance working conditions in nursing and medical personnel, as they know that omitting such practices would be counterproductive, both for occupational health[37] and for the health systems[38],[39].
The evidence from the Ibero-American context regarding the first type of outcome (1a) is more solid compared to the evidence from other countries, such as Australia, Finland, and the United States; this evidence is more solid because in the reports from Ibero-America the effects of exposure to light during naps positively extend to the alertness, and because there are a decrease in irritability, eye discomfort, and headaches[34]. In case an infrequent and unexpected event occurs that requires a quick and effective response, scheduled naps improve long-term attention. In addition, scheduled naps reduce fatigue or drowsiness symptoms and, most importantly, improve the work performance of medical personnel and emergency workers[38].
Favorable evidence on the first type of outcome (1a) differs in context, in the number of included studies (six randomized controlled trials in Latin America versus two randomized controlled trials in other countries), and the inadequate comparison between shifts (day versus night). In another study[37] addressing Norway, Canada, the United States, Japan, Switzerland, and Taiwan (13 low quality randomized controlled trials), with three intervention groups, there were also differences in the frequency of naps (2 to 4 in Latin America versus one in other countries) and the number of follow-ups (8 to 12 in Latin America versus one in other countries). The duration of naps was also different (10 minutes in Latin America versus 8.4 to 15 minutes in Europe, North America, and Asia), as was the existence of quasi-experimental studies[39],[40].
The quality of the evidence in the multi-component interventions related to policies for teamwork through the promotion of group cohesion is low (for decision-making in the first place, and active participation of medical personnel in second place[65],[66]); it is thus pertinent to adopt the guidelines of the WHO5 and of other academic reports that recommend social support and team management practices through representativity and cooperation among workers, based on the integrity and fairness of health government workers[9],[29],[41],[42].
Regarding the interventions related to the change of behaviors in non-medical personnel, evidence on raising awareness for the prevention of psychosocial risks at work was of very low-quality[32],[61],[67],[68]; the academia thus proposes the adoption of management practices such as task assignment (autonomy for the execution of tasks) and trust towards subordinates [9]. Here it is assumed that healthcare leaders promote an organizational culture that fosters collaborative learning and motivation in healthcare personnel[29].
Regarding complex behavioral changes (with evidence of very low quality on the participation of workers in promoting psychosocial occupational health[67],[68]) several studies[16],[26],[27],[28] agree that government workers' attitude has a high impact. These studies indicate that the practices that would promote change and improve participation are supervision with feedback, task management and assistance, cooperation, and willingness to listen. These activities generate trust, dialogues, and anticipation between government workers and other workers[9].
The evidence on the development of leadership in workers and managers in health centers is of moderate quality, even when consulting, participation, and negotiation mechanisms are involved[61]; these practices are far from those where employees share common objectives to gain a general vision[9] or to influence the prevention of psychosocial risks at work through cognitive changes[25]. This is due to the presence of stress-generating leadership styles and to the high levels of generalized emotional demands in different contexts[14],[15],[16],[18],[23], which increase the perception of job insecurity[18]. Consequently, the need to promote a positive organizational culture is strengthened, where communication and trust of health care government workers should predominate[29] and management practices aimed at preventing and promoting psychosocial occupational health. In other words, it is necessary to balance work and personal life[23],[41],[42].
Finally, in contrast to the positive evidence found on interventions for transformational leadership[25],[29], and for changes in behavior and attitudes in support of autonomy[16],[26],[27],[28], the evidence gaps found revealed the current prevalence of preventive practices based on multi-component interventions in the Ibero-American agenda. Despite the benefits for both psychosocial health and work productivity[5], these practices exacerbate risks related to the lack of support from supervisors in four countries[11],[16],[18],[19], to the high demands and emotional pressure in three Latin American countries and Portugal[14],[15],[16],[19], and to the negative factors linked to the organizational environment and culture in health centers in three countries[11],[17],[19].
Limitations
The review's limitation is that only a fifth of the outcomes presents a high quality of evidence, which only supports policies that improve working conditions. The rest of the evidence ranges from moderate to very low quality (80% of the studies, 13/16), which does not allow the selection of more efficient practices. For this reason, more studies of better quality are required. The strength of the present study is that, in addition to addressing a context and work sector that has not been well studied, we identified evidence gaps that constitute eight future research lines, either for preventive or recuperative interventions for psychosocial risks in occupational health.
Conclusions
The preventive practices that allow the establishment of policies for the prevention of psychosocial risks in Ibero-American health centers are linked to preventing the effects of drowsiness and sleep disorders derived from night shift hospital work in doctors and nurses.
The evidence of moderate quality on preventive practices based on multi-component interventions (e.g., interactive psychosocial training workshops for changing attitudes and work gymnastics) does not support conclusive improvements in adaptation to third parties' emotional demands. Moreover, talks or awareness visits do not generate any changes.
Training practices, consulting mechanisms, labor participation-negotiation, or training-education do not generate significant changes in leadership capacities or multidisciplinary communication.
Low- and very low-quality evidence does not endorse policies for teamwork that use training practices and participatory management with organizational support or interactive-experiential workshops with participatory techniques and contextual or awareness-raising interviews.
New systematic reviews that include high quality randomized controlled trials are required. Systematic reviews that include more randomized controlled trials are also required.
Preventive practices for psychosocial risks in Ibero-American health centers can be grouped into four levels of intervention:
a) Improvement policies for working conditions and the promotion of teamwork;
b) Leadership development;
c) Support for decision-making and organizational communication;
d) Support for personal and professional development.
Evidence gaps on psychosocial risks in Ibero-American health centers are related to job design, performance evaluation, instrumentalization systems, institutional objectives, interpersonal relationships and conflict resolution, improvement of organizational communication, and organizational changes.
Notes
Authorship contributions
The author was responsible for the elaboration, preparation, and revision of the manuscript.
Competing interests
The author has completed the ICMJE conflict of interest declaration form, and declares that he has not received funding for the report; he has not had financial relationships with organizations that may have an interest in the published article in the last three years; and does not have other relationships or activities that could influence the publication of this paper. The corresponding forms can be requested by contacting the author or the editorial of the Journal.
Funding
The author declares that there were no external sources of funding.
From the editors
The original version of this manuscript was submitted in Spanish, which was the version used for peer review. This English version was provided by the authors and has been copyedited by the Journal.
Declaration of data availability
Part of this paper's results comes from the author's doctoral thesis in public health at the National University Federico Villarreal. The author declares that the data obtained from this research are available upon request and in the open-access academic repository FIGSHARE, with doi 10.6084/m9.figshare.12580970. The link to the document is as follows.
Acknowledgments
I thank Prof. Dr. Roger dos Santos Rosa, PPG em Saúde Coletiva, UFRGS, Brazil, and the OEA / OPS-GCUB-V2015 Scholarship Program, which provided academic and financial support for data collection from UFRGS, Brazil.
Annexes
Annex 1.

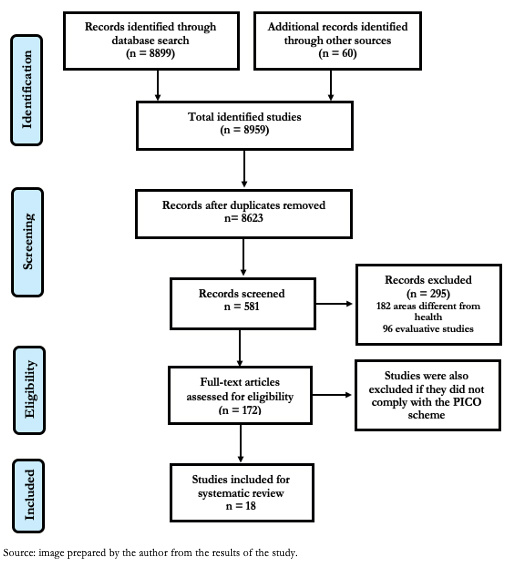 Figure 1. Information flow diagram according to the PRISMA-P phases of the systematic review[45]
Figure 1. Information flow diagram according to the PRISMA-P phases of the systematic review[45]

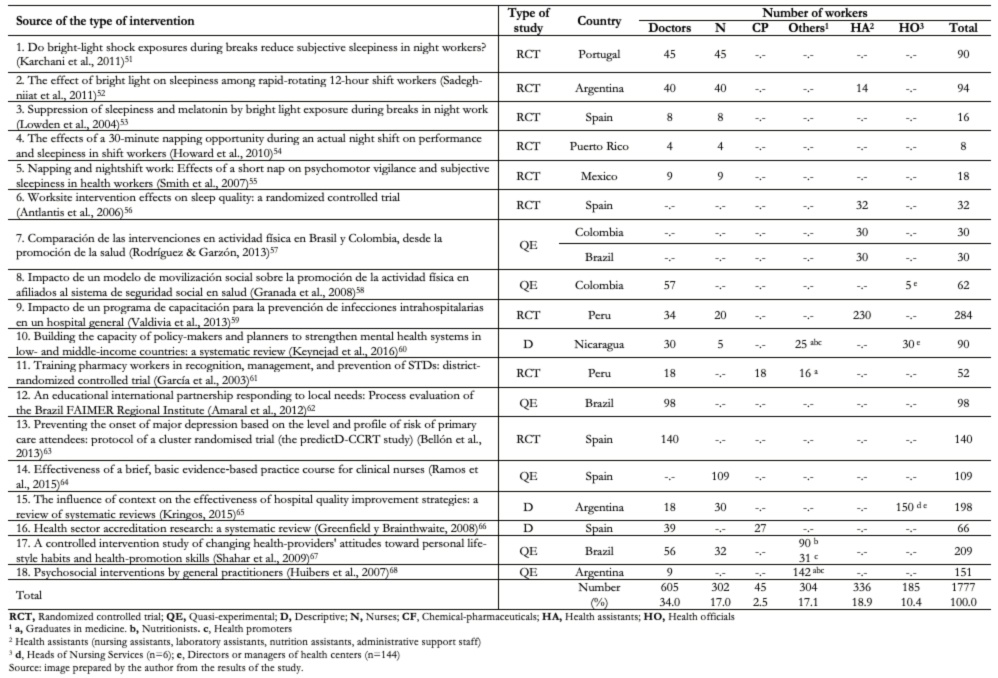 Table 1. Studies included in this work according to the country and the number of healthcare workers involved. Period 2003 to 2016.
Table 1. Studies included in this work according to the country and the number of healthcare workers involved. Period 2003 to 2016.

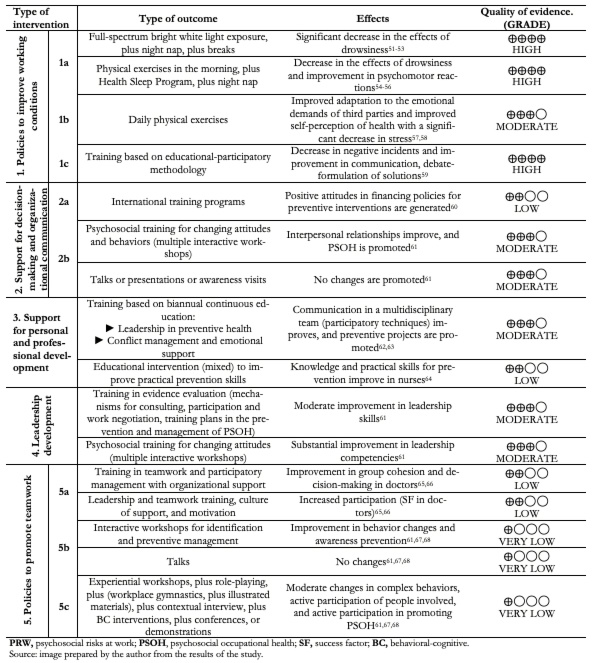 Table 2. Summary of types of intervention, type of outcome, effects, and quality of evidence (GRADE).
Table 2. Summary of types of intervention, type of outcome, effects, and quality of evidence (GRADE).

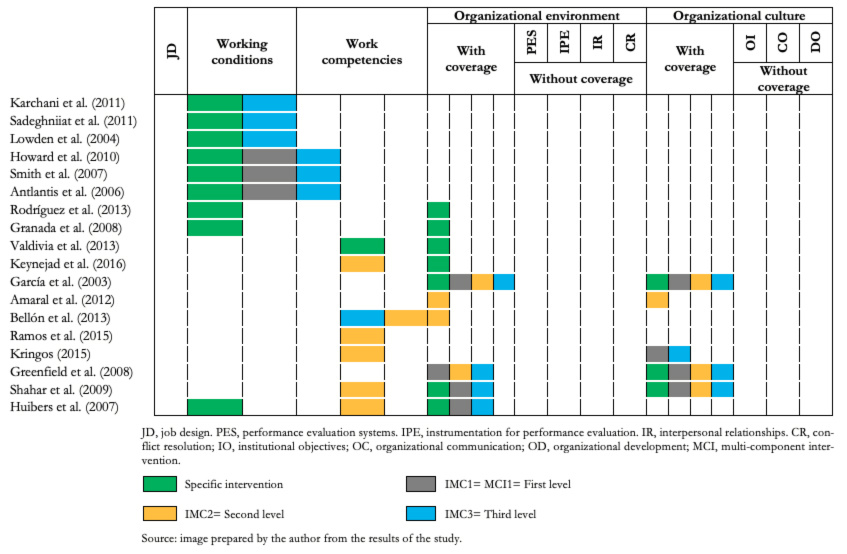 Table 3. Evidence gaps according to domains of psychosocial risk prevention intervention. Time period 2003 to 2016.
Table 3. Evidence gaps according to domains of psychosocial risk prevention intervention. Time period 2003 to 2016.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Objective
To identify preventive practices for psychosocial risks in Ibero-American health centers, including gaps in evidence, and to synthesize effectiveness according to dimensions and level of intervention.
Methods
Design: a global evidence mapping type systematic review. Data sources: Cochrane Central Register of Controlled Trials, Health Systems Evidence, The Campbell Collaboration, PubMed, BioMed Central, CINAHL, EMBASE, Lilacs, and Health Evidence Portal. Review methods: Ad hoc descriptors were used to identify randomized controlled trials and other types of studies. The search was done between January 2003 and March 2020, limited to the English, Portuguese, and Spanish. The PRISMA-P protocol was applied to register the synthesis of the included studies. The quality of the evidence was evaluated according to the GRADE protocol and by three external evaluators.
Results
A total of 8959 studies were identified, and, after screening and eligibility assessment, 18 studies were included in the systematic review, involving 1777 workers from 176 health centers in Spain, Portugal, Mexico, Nicaragua, Colombia, Brazil, Peru, and Argentina. Half of the included studies are randomized controlled trials; 37.2% of the included studies were deemed of moderate quality, while 18.7% were of high quality.
Conclusions
Preventive practices with strong evidence correspond to policies that improve the working conditions of night hospital work. We found low-quality evidence in six preventive dimensions for the practices based on multi-component interventions. We found evidence gaps in five domains of preventive interventions for psychosocial risks.
 Author:
Luis Fidel Abregú-Tueros[1]
Author:
Luis Fidel Abregú-Tueros[1]
Affiliation:
[1] Universidade Federal do Rio Grande do Sul, Post-Graduate Program in Social and Institutional Psychology, Porto Alegre, RS, Brazil
E-mail: luis.abregu@unas.edu.pe
Author address:
[1] Ramiro Barcelos 2600 Santa Cecilia,
Porto Alegre, RS, 90035-003, Brazil

Citation: Abregú-Tueros LF. A systematic review of the preventive practices for psychosocial risks in Ibero-American health centers. Medwave 2020;20(7):e8000 doi: 10.5867/medwave.2020.07.8000
Submission date: 11/12/2019
Acceptance date: 19/7/2020
Publication date: 20/8/2020
Origin: Not commissioned.
Type of review: Externally peer-reviewed by four reviewers, double-blind.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Oficina Sanitaria Panamericana (OSP). Salud para todos: propuesta para una estrategia mundial de la OMS. Bol Oficina Sanit Panam. 1995 Nov; 119(5): 442-50. [Internet] | Link |
- Leka S, Jain A. Mental health in the workplace in Europe. Brussels: Funded by the European Union in the frame of the 3rd EU Health Programme. 2017. [Internet] | Link |
- Chambel MJ. Psicologia da saúde ocupacional. Lisboa: PACTOR. 2016.
- Landsbergis PA, Choi BC, Dobson M, Sembajwe G, Slatin C, Delp L, et al. The key role of work in population health inequities. Am J Public Health. 2018 Mar; 108(3): 296-7. | CrossRef | PubMed |
- World Health Organization (WHO). Mental health in the workplace. Information sheet, May 2019 WHO. 2019. [Internet] | Link |
- Vévoda J, Vévodová Š, Nakládalová M. Psychosocial risks in healthcare. Cas Lek Cesk. 2018 Dec; 157(1): 411-18. | PubMed |
- Cenk SC. An analysis of the exposure to violence and burnout levels of ambulance staff. Turk J Emerg Med. 2018 Sep 27;19(1):21-25. | CrossRef | PubMed |
- Gomes C, Curral L, Caetano A. The mediating effect of work engagement on the relationship between self‐leadership and individual innovation. Int J Innovat Manag. 2015 Feb; 19: 1550009. | CrossRef |
- Hilaire FS, Hélène M, Lefebvre R. Managerial practices to reduce psychosocial risk exposure: A competency‐based approach. Can J Adm Sci. 2018 Jul; 35(4): 535-50. | CrossRef |
- Uribe, ME. La responsabilidad social empresarial y el enfoque estratégico de la organización: evidencia empírica de dos sectores. 2018 Jun; 19(1): 113-39. | CrossRef |
- Ministerio de Salud de Chile. Protocolo de vigilancia de riesgos psicosociales en el trabajo. Santiago de Chile: Departamento de Salud Ocupacional, Subsecretaria de Salud Pública. 2013. p.11. [Internet] | Link |
- Aranda C, González R, Pando M, Hidalgo G. Factores de riesgo psicosocial laborales, apoyo social y síndrome de Burnout en médicos de familia de tres instituciones públicas de salud de Guadalajara (México). Salud Uninorte. 2013 Dic; 29(3): 487-500. [Internet] | Link |
- Malleville S. Qualidade na atenção, qualidade no emprego? as fontes de intensificação do trabalho em ocupações de cuidado, análise de dois estabelecimentos de saúde privada. Trabalho (En) Cena, 2019; 4: 88-107. | CrossRef |
- Henry ML. Salud laboral en el escenario productivo actual. La creciente incidencia de los riesgos psicosociales. Rev. Cien. Soc. 2019 Jun; 32(44): 171-96. | CrossRef |
- Sarsosa K, Charria-Ortiz VH, Arenas-Ortiz F. Caracterización de los riesgos psicosociales intralaborales en jefes asistenciales de cinco clínicas nivel III de Santiago de Cali (Colombia). Rev. Gerenc. Polit. Salud. 2014 Dic; 13(27): 348-61. | CrossRef |
- Tenório A, De Souza C, Susser E, Rossi R. Depresión relacionada con el trabajo en personal de equipos de atención primaria en Brasil. Rev Panam Salud Publica. 2016; 106: 1990-7. | CrossRef | PubMed |
- Arroyo J, Hartz J, Lau M. Recursos humanos en salud al 2011: Evidencias para la toma de decisiones. Lima: Ministerio de Salud. 2011. [Internet] | CrossRef | Link |
- Marín-Lluch P, García C, Muñoz JL, Rabanaque G. Detección de riesgos psicosociales en profesionales sanitarios de un área de salud. Aten Primaria. 2006 Mar; 37(5): 302-3. [Internet] | Link |
- Fonseca S, Cunha S, Campos R, Gonçalves S, Queirós C. Saúde ocupacional dos profissionais de emergência pré-hospitalar: Contributo do trauma e coping. International Journal on Working Conditions. 2019 Jun; 17(1): 69-88. | CrossRef |
- Segarra M, Villena BM, González MN, Romero A, Rodríguez A. Occupational risk-prevention diagnosis: A study of construction SMEs in Spain. Saf Sci. 2017 Feb; 92(1): 104-15. | CrossRef |
- Beck D, Lenhardt U. Consideration of psychosocial factors in workplace risk assessments: findings from a company survey in Germany. Int Arch Occup Environ Health. 2019 Apr; 92(3): 435-51. | CrossRef | PubMed |
- Salas-Zapata W, Ríos-Osorio L, Gómez-Arias RD, Álvarez-Del Castillo X. Paradigmas en el análisis de políticas públicas de salud: Limitaciones y desafíos. Rev Panam Salud Publica. 2012 jul; 32(1): 77-81. [Internet] | Link |
- Taris TW, Schaufeli WB. The job demands‐resources model. In: Clarke S, Probst TM, Guldenmund F, Passmore J. (Eds.). The psychology of occupational safety and workplace health. New Jersey: John Wiley & Sons, Ltd. 2016. p.155-80. | CrossRef |
- Lewis R, Yarker J, Donaldson-Feilder E. The vital role of line managers in managing psychosocial risks. In: Biron C, Karanika‐Murray M, Cooper CL. (Eds.). Improving organizational interventions for stress and well‐being. Addressing process and context. London: Psychology Press/Taylor & Francis Group. 2012, p.216-37.
- Harms PD, Credé M, Tynan M, Leon M, Wonho J. Leadership and stress: A meta‐analytic review. Leadership Quarterly. 2017 Feb; 28(1): 178-94. | CrossRef |
- Fallman SL, Jutengren G, Dellve L. The impact of restricted decision-making autonomy on health care managers’ health and work performance. J. Nurs. Manag. 2019 May; 27(4): 706-14. | CrossRef |
- Gilbert MH, Dagenais-Desmarais V, St‐Hilaire F. Transformational leadership and autonomy support management behaviours: The role of specificity in predicting employees' psychological health. Leadersh Org Dev J. 2017 Apr; 38(2): 320-32. | CrossRef |
- Hower K, Pfaff H, Kowalski C, Wensing M, Ansmann L. Measuring change attitudes in health care organizations. J Health Organ Manag. 2019 May; 33(3): 266-85. | CrossRef | PubMed |
- Goh SC, Chan C, Kuziemsky C. Teamwork, organizational learning, patient safety and job outcomes. Int J Health Care Qual Assur. 2013; 26(5): 420-32. | CrossRef | PubMed |
- Skagert K, Dellve L, Eklof M, Pousette A, Ahlbord GJ. Leaders' strategies for dealing with own and their subordinates' stress in public human service organisations. Appl Ergon. 2008 Nov; 39(1): 803-11. | CrossRef | PubMed |
- Czabała C, Charzyn´ska K, Mroziak B. Psychosocial interventions in workplace mental health promotion: an overview. Health Promot Int. 2011 Dec; 26(1): 70-84. | CrossRef | PubMed |
- Westphal MF, Taddei JAC, Venancio SI, Bogus CM. Breast-feeding training for health professionals and resultant institutional changes. Bull World Health Organ. 1995; 73(4): 461-8. | PubMed |
- Organización Mundial de la Salud (OMS). Crear lugares de trabajo saludables y equitativos para hombres y mujeres: Guía para empleadores y representantes de los trabajadores. Ginebra: OMS. 2011. [Internet] | Link |
- Pachito D, Eckeli A, Desouky A, Corbett M, Partonen T, Rajaratnam S, at al. Workplace lighting for improving alertness and mood in daytime e workers. Cochrane Database Syst Rev. 2018 Mar; 3: CD012243. | CrossRef |
- Faraut B, Andrillon T, Vecchierini MF, Leger D. Napping: a public health issue. From epidemiological to laboratory studies. Sleep Med Ver. 2017 Oct; 35(1): 85-100. | CrossRef | PubMed |
- Lovato N, Lack L. The effects of napping on cognitive functioning. Prog Brain Res. 2010; 185(1): 155-6. | CrossRef | PubMed |
- Slanger TE, Gross JV, Pinger A, Morfeld P, Bellinger M, Duhme AL, et al. Person-directed, non-pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work. Cochrane Database Syst Rev. 2016 Aug; 8: CD010641. | CrossRef | PubMed |
- Martin-Hill C, Barger LK, Moore C, Higgins JS, Teasley L, Weiss PM. Effects of napping during shift work on sleepiness and performance in emergency medical services personnel and similar shift workers: A systematic review and meta-analysis. Prehosp Emerg Care. 2018 Feb; 22(sup1): 47-57. | CrossRef | PubMed |
- Takahashi M, Nakata A, Haratani T, Ogawa Y, Arito H. Post-lunch nap as a worksite intervention to promote alertness on the job. Ergonomics. 2004 Jul; 47(9): 1003-13. | CrossRef | PubMed |
- Amin MM, Graber M, Ahmad K, Manta D, Hossain S, Belisova Z, et al. The effects of a mid-day nap on the neurocognitive performance of first-year medical residents: a controlled interventional pilot study. Acad Med. 2012 Oct; 87(10): 1428-33. | CrossRef | PubMed |
- Organización Mundial de la Salud (OMS). Plan de acción sobre salud mental 2013-2020. Ginebra: OMS. 2013, p.7,45-54. [Internet] | Link |
- Forastieri V. Prevención de riesgos psicosociales y estrés laboral. En: Organización Internacional del Trabajo. Boletín Internacional de Investigación Sindical. Riesgos psicosociales, estrés y violencia en el mundo del trabajo. Ginebra: PRODOC OIT. 2017. p.11-37. [Internet] | Link |
- Miake IM, Hempel S, Shanman R, Shekelle PG. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. 2016 Feb; 5: 28. | CrossRef | PubMed |
- Franco JVA, Arancibia M, Simancas-Racines D, Madrid E. Syntheses of biomedical information: narrative reviews, systematic reviews and emerging formats. Medwave. 2018 Nov; 18(7): e7354. | CrossRef | PubMed |
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009 Jul; 6(7): e1000097. | CrossRef | PubMed |
- Burton J. Entornos laborales saludables: Fundamentos y modelo de la OMS: Contextualización, prácticas y literatura de apoyo. Ginebra: OMS. 2010. p.44-69. [Internet] | Link |
- Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando FL: Academic Press. 2014 Jun.
- Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organ Res Methods. 2008 Mar; 11(2): 364-86. | CrossRef |
- Moberg J, Oxman AD, Rosenbaum S, Schünemann HJ, Guyatt G, Flottorp S, et al. GRADE Working Group. The GRADE Evidence to Decision (EtD) framework for health system and public health decisions. Health Res Policy Sys. 2018 May; 16(1): 45. | CrossRef | PubMed |
- González C, Cuadrado C. Interventions to reduce the impact of dual practice in the public health sector. Medwave. 2019 Jun; 19(5): e7643. | CrossRef | PubMed |
- Karchani M, Kakooei H, Yazdi Z, Zare M. Do bright-light shock exposures during breaks reduce subjective sleepiness in night workers?. Sleep Biol Rhythms. 2011 Apr; 9(1): 95-102. | CrossRef |
- Sadeghniiat-Haghighi K, Yazdi Z, Jahanihashemi H, Aminian O. The effect of bright light on sleepiness among rapid-rotating 12-hour shift workers. Scand J Work Environ Health. 2011 Jan; 37(1): 77-9. | CrossRef | PubMed |
- Lowden A, Akerstedt T, Wibom R. Suppression of sleepiness and melatonin by bright light exposure during breaks in night work. J Sleep Res. 2004 Mar; 13(1): 37-43. | CrossRef | PubMed |
- Howard ME, Radford L, Jackson ML, Swann P, Kennedy GA. The effects of a 30-minute napping opportunity during an actual night shift on performance and sleepiness in shift workers. Biol Rhythm Res. 2010; 41(2): 137-48. | CrossRef |
- Smith A, Kilby S, Jorgensen G,Douglas J. Napping and nightshift work: Effects of a short nap on psychomotor vigilance and subjective sleepiness in health workers. Sleep Biol. Rhythms. 2007 Abr; 5(2): 117-25. | CrossRef |
- Atlantis E, Chow CM, Kirby A, Singh MA. Worksite intervention effects on sleep quality: a randomized controlled trial. J Occup Health Psychol. 2006 Oct; 11(4): 291-304. | CrossRef | PubMed |
- Rodríguez-León DL, Garzón-Molina NM. Comparación de las intervenciones en actividad física en Brasil y Colombia, desde la promoción de la salud. Rev Fac Med. 2013; 61(4): 449-58. [Internet] | Link |
- Granada-Echeverri P, Zapata-Valencia CD, Giraldo-Trujillo JC. Impacto de un modelo de movilización social sobre la promoción de la actividad física en afiliados al sistema de seguridad social en salud. Rev Salud Pública. 2008 Jul; 10(3): 361-73. [Internet] | Link |
- Valdivia LM, Lam C, Mucha R, Chávez J, Tanta J, Alvarezcano J, et al. Impacto de un programa de capacitación para la prevención de infecciones intrahospitalarias en un hospital general. Trauma Fund MAPFRE. 2013; 24(2): 126-31. [Internet] | Link |
- Keynejad R, Semrau M, Toynbee M, Evans-Lacko S, Lund C, Gureje O, et al. Building the capacity of policy-makers and planners to strengthen mental health systems in low- and middle-income countries: a systematic review. BMC Health Serv Res. 2016 Oct; 16(1): 601. | CrossRef | PubMed |
- García P, Hughes J, Carcamo C, Holmes K. Training pharmacy workers in recognition, management, and prevention of STDs: district-randomized controlled trial. Bull World Health Organ. 2003; 81(11): 806-14. | PubMed |
- Amaral E, Campos HH, Friedman S, Morahan PS, Araujo MN, Carvalho PM, et al. An educational international partnership responding to local needs: Process evaluation of the Brazil FAIMER Regional Institute. Educ Health (Abingdon). 2012 Nov; 25(2): 116-23. | CrossRef | PubMed |
- Bellón JA, Conejo-Cerón S, Moreno-Peral P, King M, Nazareth I, Martín-Pérez C, et al. Preventing the onset of major depression based on the level and profile of risk of primary care attendees: protocol of a cluster randomised trial (the predictD-CCRT study). BMC Psychiatry. 2013 Jun; 13(171): 1-16. | CrossRef | PubMed |
- Ramos-Morcillo AJ, Fernández-Salazar S, Ruzafa-Martínez M, Del Pino-Casado R. Effectiveness of a brief, basic evidence‐based practice course for clinical nurses. Worldviews Evid Based Nurs. 2015 Aug; 12(4): 199–207. | CrossRef | PubMed |
- Kringos DS, Sunol R, Wagner C, Mannion R, Michel P, Klazinga NS, at al. The influence of context on the effectiveness of hospital quality improvement strategies: a review of systematic reviews. BMC Health Serv Res. 2015 Jul; 15(277): 1-13. | CrossRef | PubMed |
- Greenfield D, Braithwaite J. Health sector accreditation research: a systematic review. Int J Qual Health Care. 2008 Jun; 20(1): 172-83. | CrossRef | PubMed |
- Shahar DR, Henkin Y, Rozen GS, Adler D, Levy O, Safra C, at al. A controlled intervention study of changing health-providers' attitudes toward personal lifestyle habits and health-promotion skills. Nutrition. 2009 May; 25(5): 532-9. | CrossRef | PubMed |
- Huibers M, Beurskens A, Bleijenberg G, Van Schayck CP. Psychosocial interventions by general practitioners. Cochrane Database Syst Rev. 2007 Jul; (3): CD003494. | CrossRef | PubMed |
 Oficina Sanitaria Panamericana (OSP). Salud para todos: propuesta para una estrategia mundial de la OMS. Bol Oficina Sanit Panam. 1995 Nov; 119(5): 442-50. [Internet] | Link |
Oficina Sanitaria Panamericana (OSP). Salud para todos: propuesta para una estrategia mundial de la OMS. Bol Oficina Sanit Panam. 1995 Nov; 119(5): 442-50. [Internet] | Link | Leka S, Jain A. Mental health in the workplace in Europe. Brussels: Funded by the European Union in the frame of the 3rd EU Health Programme. 2017. [Internet] | Link |
Leka S, Jain A. Mental health in the workplace in Europe. Brussels: Funded by the European Union in the frame of the 3rd EU Health Programme. 2017. [Internet] | Link | Chambel MJ. Psicologia da saúde ocupacional. Lisboa: PACTOR. 2016.
Chambel MJ. Psicologia da saúde ocupacional. Lisboa: PACTOR. 2016.  Landsbergis PA, Choi BC, Dobson M, Sembajwe G, Slatin C, Delp L, et al. The key role of work in population health inequities. Am J Public Health. 2018 Mar; 108(3): 296-7. | CrossRef | PubMed |
Landsbergis PA, Choi BC, Dobson M, Sembajwe G, Slatin C, Delp L, et al. The key role of work in population health inequities. Am J Public Health. 2018 Mar; 108(3): 296-7. | CrossRef | PubMed | World Health Organization (WHO). Mental health in the workplace. Information sheet, May 2019 WHO. 2019. [Internet] | Link |
World Health Organization (WHO). Mental health in the workplace. Information sheet, May 2019 WHO. 2019. [Internet] | Link | Vévoda J, Vévodová Š, Nakládalová M. Psychosocial risks in healthcare. Cas Lek Cesk. 2018 Dec; 157(1): 411-18. | PubMed |
Vévoda J, Vévodová Š, Nakládalová M. Psychosocial risks in healthcare. Cas Lek Cesk. 2018 Dec; 157(1): 411-18. | PubMed | Cenk SC. An analysis of the exposure to violence and burnout levels of ambulance staff. Turk J Emerg Med. 2018 Sep 27;19(1):21-25. | CrossRef | PubMed |
Cenk SC. An analysis of the exposure to violence and burnout levels of ambulance staff. Turk J Emerg Med. 2018 Sep 27;19(1):21-25. | CrossRef | PubMed | Gomes C, Curral L, Caetano A. The mediating effect of work engagement on the relationship between self‐leadership and individual innovation. Int J Innovat Manag. 2015 Feb; 19: 1550009. | CrossRef |
Gomes C, Curral L, Caetano A. The mediating effect of work engagement on the relationship between self‐leadership and individual innovation. Int J Innovat Manag. 2015 Feb; 19: 1550009. | CrossRef | Hilaire FS, Hélène M, Lefebvre R. Managerial practices to reduce psychosocial risk exposure: A competency‐based approach. Can J Adm Sci. 2018 Jul; 35(4): 535-50. | CrossRef |
Hilaire FS, Hélène M, Lefebvre R. Managerial practices to reduce psychosocial risk exposure: A competency‐based approach. Can J Adm Sci. 2018 Jul; 35(4): 535-50. | CrossRef | Uribe, ME. La responsabilidad social empresarial y el enfoque estratégico de la organización: evidencia empírica de dos sectores. 2018 Jun; 19(1): 113-39. | CrossRef |
Uribe, ME. La responsabilidad social empresarial y el enfoque estratégico de la organización: evidencia empírica de dos sectores. 2018 Jun; 19(1): 113-39. | CrossRef | Ministerio de Salud de Chile. Protocolo de vigilancia de riesgos psicosociales en el trabajo. Santiago de Chile: Departamento de Salud Ocupacional, Subsecretaria de Salud Pública. 2013. p.11. [Internet] | Link |
Ministerio de Salud de Chile. Protocolo de vigilancia de riesgos psicosociales en el trabajo. Santiago de Chile: Departamento de Salud Ocupacional, Subsecretaria de Salud Pública. 2013. p.11. [Internet] | Link | Aranda C, González R, Pando M, Hidalgo G. Factores de riesgo psicosocial laborales, apoyo social y síndrome de Burnout en médicos de familia de tres instituciones públicas de salud de Guadalajara (México). Salud Uninorte. 2013 Dic; 29(3): 487-500. [Internet] | Link |
Aranda C, González R, Pando M, Hidalgo G. Factores de riesgo psicosocial laborales, apoyo social y síndrome de Burnout en médicos de familia de tres instituciones públicas de salud de Guadalajara (México). Salud Uninorte. 2013 Dic; 29(3): 487-500. [Internet] | Link | Malleville S. Qualidade na atenção, qualidade no emprego? as fontes de intensificação do trabalho em ocupações de cuidado, análise de dois estabelecimentos de saúde privada. Trabalho (En) Cena, 2019; 4: 88-107. | CrossRef |
Malleville S. Qualidade na atenção, qualidade no emprego? as fontes de intensificação do trabalho em ocupações de cuidado, análise de dois estabelecimentos de saúde privada. Trabalho (En) Cena, 2019; 4: 88-107. | CrossRef | Henry ML. Salud laboral en el escenario productivo actual. La creciente incidencia de los riesgos psicosociales. Rev. Cien. Soc. 2019 Jun; 32(44): 171-96. | CrossRef |
Henry ML. Salud laboral en el escenario productivo actual. La creciente incidencia de los riesgos psicosociales. Rev. Cien. Soc. 2019 Jun; 32(44): 171-96. | CrossRef | Sarsosa K, Charria-Ortiz VH, Arenas-Ortiz F. Caracterización de los riesgos psicosociales intralaborales en jefes asistenciales de cinco clínicas nivel III de Santiago de Cali (Colombia). Rev. Gerenc. Polit. Salud. 2014 Dic; 13(27): 348-61. | CrossRef |
Sarsosa K, Charria-Ortiz VH, Arenas-Ortiz F. Caracterización de los riesgos psicosociales intralaborales en jefes asistenciales de cinco clínicas nivel III de Santiago de Cali (Colombia). Rev. Gerenc. Polit. Salud. 2014 Dic; 13(27): 348-61. | CrossRef | Tenório A, De Souza C, Susser E, Rossi R. Depresión relacionada con el trabajo en personal de equipos de atención primaria en Brasil. Rev Panam Salud Publica. 2016; 106: 1990-7. | CrossRef | PubMed |
Tenório A, De Souza C, Susser E, Rossi R. Depresión relacionada con el trabajo en personal de equipos de atención primaria en Brasil. Rev Panam Salud Publica. 2016; 106: 1990-7. | CrossRef | PubMed | Arroyo J, Hartz J, Lau M. Recursos humanos en salud al 2011: Evidencias para la toma de decisiones. Lima: Ministerio de Salud. 2011. [Internet] | CrossRef | Link |
Arroyo J, Hartz J, Lau M. Recursos humanos en salud al 2011: Evidencias para la toma de decisiones. Lima: Ministerio de Salud. 2011. [Internet] | CrossRef | Link | Marín-Lluch P, García C, Muñoz JL, Rabanaque G. Detección de riesgos psicosociales en profesionales sanitarios de un área de salud. Aten Primaria. 2006 Mar; 37(5): 302-3. [Internet] | Link |
Marín-Lluch P, García C, Muñoz JL, Rabanaque G. Detección de riesgos psicosociales en profesionales sanitarios de un área de salud. Aten Primaria. 2006 Mar; 37(5): 302-3. [Internet] | Link | Fonseca S, Cunha S, Campos R, Gonçalves S, Queirós C. Saúde ocupacional dos profissionais de emergência pré-hospitalar: Contributo do trauma e coping. International Journal on Working Conditions. 2019 Jun; 17(1): 69-88. | CrossRef |
Fonseca S, Cunha S, Campos R, Gonçalves S, Queirós C. Saúde ocupacional dos profissionais de emergência pré-hospitalar: Contributo do trauma e coping. International Journal on Working Conditions. 2019 Jun; 17(1): 69-88. | CrossRef | Segarra M, Villena BM, González MN, Romero A, Rodríguez A. Occupational risk-prevention diagnosis: A study of construction SMEs in Spain. Saf Sci. 2017 Feb; 92(1): 104-15. | CrossRef |
Segarra M, Villena BM, González MN, Romero A, Rodríguez A. Occupational risk-prevention diagnosis: A study of construction SMEs in Spain. Saf Sci. 2017 Feb; 92(1): 104-15. | CrossRef | Beck D, Lenhardt U. Consideration of psychosocial factors in workplace risk assessments: findings from a company survey in Germany. Int Arch Occup Environ Health. 2019 Apr; 92(3): 435-51. | CrossRef | PubMed |
Beck D, Lenhardt U. Consideration of psychosocial factors in workplace risk assessments: findings from a company survey in Germany. Int Arch Occup Environ Health. 2019 Apr; 92(3): 435-51. | CrossRef | PubMed | Salas-Zapata W, Ríos-Osorio L, Gómez-Arias RD, Álvarez-Del Castillo X. Paradigmas en el análisis de políticas públicas de salud: Limitaciones y desafíos. Rev Panam Salud Publica. 2012 jul; 32(1): 77-81. [Internet] | Link |
Salas-Zapata W, Ríos-Osorio L, Gómez-Arias RD, Álvarez-Del Castillo X. Paradigmas en el análisis de políticas públicas de salud: Limitaciones y desafíos. Rev Panam Salud Publica. 2012 jul; 32(1): 77-81. [Internet] | Link | Taris TW, Schaufeli WB. The job demands‐resources model. In: Clarke S, Probst TM, Guldenmund F, Passmore J. (Eds.). The psychology of occupational safety and workplace health. New Jersey: John Wiley & Sons, Ltd. 2016. p.155-80. | CrossRef |
Taris TW, Schaufeli WB. The job demands‐resources model. In: Clarke S, Probst TM, Guldenmund F, Passmore J. (Eds.). The psychology of occupational safety and workplace health. New Jersey: John Wiley & Sons, Ltd. 2016. p.155-80. | CrossRef | Lewis R, Yarker J, Donaldson-Feilder E. The vital role of line managers in managing psychosocial risks. In: Biron C, Karanika‐Murray M, Cooper CL. (Eds.). Improving organizational interventions for stress and well‐being. Addressing process and context. London: Psychology Press/Taylor & Francis Group. 2012, p.216-37.
Lewis R, Yarker J, Donaldson-Feilder E. The vital role of line managers in managing psychosocial risks. In: Biron C, Karanika‐Murray M, Cooper CL. (Eds.). Improving organizational interventions for stress and well‐being. Addressing process and context. London: Psychology Press/Taylor & Francis Group. 2012, p.216-37.  Harms PD, Credé M, Tynan M, Leon M, Wonho J. Leadership and stress: A meta‐analytic review. Leadership Quarterly. 2017 Feb; 28(1): 178-94. | CrossRef |
Harms PD, Credé M, Tynan M, Leon M, Wonho J. Leadership and stress: A meta‐analytic review. Leadership Quarterly. 2017 Feb; 28(1): 178-94. | CrossRef | Fallman SL, Jutengren G, Dellve L. The impact of restricted decision-making autonomy on health care managers’ health and work performance. J. Nurs. Manag. 2019 May; 27(4): 706-14. | CrossRef |
Fallman SL, Jutengren G, Dellve L. The impact of restricted decision-making autonomy on health care managers’ health and work performance. J. Nurs. Manag. 2019 May; 27(4): 706-14. | CrossRef | Gilbert MH, Dagenais-Desmarais V, St‐Hilaire F. Transformational leadership and autonomy support management behaviours: The role of specificity in predicting employees' psychological health. Leadersh Org Dev J. 2017 Apr; 38(2): 320-32. | CrossRef |
Gilbert MH, Dagenais-Desmarais V, St‐Hilaire F. Transformational leadership and autonomy support management behaviours: The role of specificity in predicting employees' psychological health. Leadersh Org Dev J. 2017 Apr; 38(2): 320-32. | CrossRef | Hower K, Pfaff H, Kowalski C, Wensing M, Ansmann L. Measuring change attitudes in health care organizations. J Health Organ Manag. 2019 May; 33(3): 266-85. | CrossRef | PubMed |
Hower K, Pfaff H, Kowalski C, Wensing M, Ansmann L. Measuring change attitudes in health care organizations. J Health Organ Manag. 2019 May; 33(3): 266-85. | CrossRef | PubMed | Goh SC, Chan C, Kuziemsky C. Teamwork, organizational learning, patient safety and job outcomes. Int J Health Care Qual Assur. 2013; 26(5): 420-32. | CrossRef | PubMed |
Goh SC, Chan C, Kuziemsky C. Teamwork, organizational learning, patient safety and job outcomes. Int J Health Care Qual Assur. 2013; 26(5): 420-32. | CrossRef | PubMed | Skagert K, Dellve L, Eklof M, Pousette A, Ahlbord GJ. Leaders' strategies for dealing with own and their subordinates' stress in public human service organisations. Appl Ergon. 2008 Nov; 39(1): 803-11. | CrossRef | PubMed |
Skagert K, Dellve L, Eklof M, Pousette A, Ahlbord GJ. Leaders' strategies for dealing with own and their subordinates' stress in public human service organisations. Appl Ergon. 2008 Nov; 39(1): 803-11. | CrossRef | PubMed | Czabała C, Charzyn´ska K, Mroziak B. Psychosocial interventions in workplace mental health promotion: an overview. Health Promot Int. 2011 Dec; 26(1): 70-84. | CrossRef | PubMed |
Czabała C, Charzyn´ska K, Mroziak B. Psychosocial interventions in workplace mental health promotion: an overview. Health Promot Int. 2011 Dec; 26(1): 70-84. | CrossRef | PubMed | Westphal MF, Taddei JAC, Venancio SI, Bogus CM. Breast-feeding training for health professionals and resultant institutional changes. Bull World Health Organ. 1995; 73(4): 461-8. | PubMed |
Westphal MF, Taddei JAC, Venancio SI, Bogus CM. Breast-feeding training for health professionals and resultant institutional changes. Bull World Health Organ. 1995; 73(4): 461-8. | PubMed | Organización Mundial de la Salud (OMS). Crear lugares de trabajo saludables y equitativos para hombres y mujeres: Guía para empleadores y representantes de los trabajadores. Ginebra: OMS. 2011. [Internet] | Link |
Organización Mundial de la Salud (OMS). Crear lugares de trabajo saludables y equitativos para hombres y mujeres: Guía para empleadores y representantes de los trabajadores. Ginebra: OMS. 2011. [Internet] | Link | Pachito D, Eckeli A, Desouky A, Corbett M, Partonen T, Rajaratnam S, at al. Workplace lighting for improving alertness and mood in daytime e workers. Cochrane Database Syst Rev. 2018 Mar; 3: CD012243. | CrossRef |
Pachito D, Eckeli A, Desouky A, Corbett M, Partonen T, Rajaratnam S, at al. Workplace lighting for improving alertness and mood in daytime e workers. Cochrane Database Syst Rev. 2018 Mar; 3: CD012243. | CrossRef | Faraut B, Andrillon T, Vecchierini MF, Leger D. Napping: a public health issue. From epidemiological to laboratory studies. Sleep Med Ver. 2017 Oct; 35(1): 85-100. | CrossRef | PubMed |
Faraut B, Andrillon T, Vecchierini MF, Leger D. Napping: a public health issue. From epidemiological to laboratory studies. Sleep Med Ver. 2017 Oct; 35(1): 85-100. | CrossRef | PubMed | Lovato N, Lack L. The effects of napping on cognitive functioning. Prog Brain Res. 2010; 185(1): 155-6. | CrossRef | PubMed |
Lovato N, Lack L. The effects of napping on cognitive functioning. Prog Brain Res. 2010; 185(1): 155-6. | CrossRef | PubMed | Slanger TE, Gross JV, Pinger A, Morfeld P, Bellinger M, Duhme AL, et al. Person-directed, non-pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work. Cochrane Database Syst Rev. 2016 Aug; 8: CD010641. | CrossRef | PubMed |
Slanger TE, Gross JV, Pinger A, Morfeld P, Bellinger M, Duhme AL, et al. Person-directed, non-pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work. Cochrane Database Syst Rev. 2016 Aug; 8: CD010641. | CrossRef | PubMed | Martin-Hill C, Barger LK, Moore C, Higgins JS, Teasley L, Weiss PM. Effects of napping during shift work on sleepiness and performance in emergency medical services personnel and similar shift workers: A systematic review and meta-analysis. Prehosp Emerg Care. 2018 Feb; 22(sup1): 47-57. | CrossRef | PubMed |
Martin-Hill C, Barger LK, Moore C, Higgins JS, Teasley L, Weiss PM. Effects of napping during shift work on sleepiness and performance in emergency medical services personnel and similar shift workers: A systematic review and meta-analysis. Prehosp Emerg Care. 2018 Feb; 22(sup1): 47-57. | CrossRef | PubMed | Takahashi M, Nakata A, Haratani T, Ogawa Y, Arito H. Post-lunch nap as a worksite intervention to promote alertness on the job. Ergonomics. 2004 Jul; 47(9): 1003-13. | CrossRef | PubMed |
Takahashi M, Nakata A, Haratani T, Ogawa Y, Arito H. Post-lunch nap as a worksite intervention to promote alertness on the job. Ergonomics. 2004 Jul; 47(9): 1003-13. | CrossRef | PubMed | Amin MM, Graber M, Ahmad K, Manta D, Hossain S, Belisova Z, et al. The effects of a mid-day nap on the neurocognitive performance of first-year medical residents: a controlled interventional pilot study. Acad Med. 2012 Oct; 87(10): 1428-33. | CrossRef | PubMed |
Amin MM, Graber M, Ahmad K, Manta D, Hossain S, Belisova Z, et al. The effects of a mid-day nap on the neurocognitive performance of first-year medical residents: a controlled interventional pilot study. Acad Med. 2012 Oct; 87(10): 1428-33. | CrossRef | PubMed | Organización Mundial de la Salud (OMS). Plan de acción sobre salud mental 2013-2020. Ginebra: OMS. 2013, p.7,45-54. [Internet] | Link |
Organización Mundial de la Salud (OMS). Plan de acción sobre salud mental 2013-2020. Ginebra: OMS. 2013, p.7,45-54. [Internet] | Link | Forastieri V. Prevención de riesgos psicosociales y estrés laboral. En: Organización Internacional del Trabajo. Boletín Internacional de Investigación Sindical. Riesgos psicosociales, estrés y violencia en el mundo del trabajo. Ginebra: PRODOC OIT. 2017. p.11-37. [Internet] | Link |
Forastieri V. Prevención de riesgos psicosociales y estrés laboral. En: Organización Internacional del Trabajo. Boletín Internacional de Investigación Sindical. Riesgos psicosociales, estrés y violencia en el mundo del trabajo. Ginebra: PRODOC OIT. 2017. p.11-37. [Internet] | Link | Miake IM, Hempel S, Shanman R, Shekelle PG. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. 2016 Feb; 5: 28. | CrossRef | PubMed |
Miake IM, Hempel S, Shanman R, Shekelle PG. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. 2016 Feb; 5: 28. | CrossRef | PubMed | Franco JVA, Arancibia M, Simancas-Racines D, Madrid E. Syntheses of biomedical information: narrative reviews, systematic reviews and emerging formats. Medwave. 2018 Nov; 18(7): e7354. | CrossRef | PubMed |
Franco JVA, Arancibia M, Simancas-Racines D, Madrid E. Syntheses of biomedical information: narrative reviews, systematic reviews and emerging formats. Medwave. 2018 Nov; 18(7): e7354. | CrossRef | PubMed | Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009 Jul; 6(7): e1000097. | CrossRef | PubMed |
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009 Jul; 6(7): e1000097. | CrossRef | PubMed | Burton J. Entornos laborales saludables: Fundamentos y modelo de la OMS: Contextualización, prácticas y literatura de apoyo. Ginebra: OMS. 2010. p.44-69. [Internet] | Link |
Burton J. Entornos laborales saludables: Fundamentos y modelo de la OMS: Contextualización, prácticas y literatura de apoyo. Ginebra: OMS. 2010. p.44-69. [Internet] | Link | Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando FL: Academic Press. 2014 Jun.
Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando FL: Academic Press. 2014 Jun.  Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organ Res Methods. 2008 Mar; 11(2): 364-86. | CrossRef |
Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organ Res Methods. 2008 Mar; 11(2): 364-86. | CrossRef | Moberg J, Oxman AD, Rosenbaum S, Schünemann HJ, Guyatt G, Flottorp S, et al. GRADE Working Group. The GRADE Evidence to Decision (EtD) framework for health system and public health decisions. Health Res Policy Sys. 2018 May; 16(1): 45. | CrossRef | PubMed |
Moberg J, Oxman AD, Rosenbaum S, Schünemann HJ, Guyatt G, Flottorp S, et al. GRADE Working Group. The GRADE Evidence to Decision (EtD) framework for health system and public health decisions. Health Res Policy Sys. 2018 May; 16(1): 45. | CrossRef | PubMed | González C, Cuadrado C. Interventions to reduce the impact of dual practice in the public health sector. Medwave. 2019 Jun; 19(5): e7643. | CrossRef | PubMed |
González C, Cuadrado C. Interventions to reduce the impact of dual practice in the public health sector. Medwave. 2019 Jun; 19(5): e7643. | CrossRef | PubMed | Karchani M, Kakooei H, Yazdi Z, Zare M. Do bright-light shock exposures during breaks reduce subjective sleepiness in night workers?. Sleep Biol Rhythms. 2011 Apr; 9(1): 95-102. | CrossRef |
Karchani M, Kakooei H, Yazdi Z, Zare M. Do bright-light shock exposures during breaks reduce subjective sleepiness in night workers?. Sleep Biol Rhythms. 2011 Apr; 9(1): 95-102. | CrossRef | Sadeghniiat-Haghighi K, Yazdi Z, Jahanihashemi H, Aminian O. The effect of bright light on sleepiness among rapid-rotating 12-hour shift workers. Scand J Work Environ Health. 2011 Jan; 37(1): 77-9. | CrossRef | PubMed |
Sadeghniiat-Haghighi K, Yazdi Z, Jahanihashemi H, Aminian O. The effect of bright light on sleepiness among rapid-rotating 12-hour shift workers. Scand J Work Environ Health. 2011 Jan; 37(1): 77-9. | CrossRef | PubMed | Lowden A, Akerstedt T, Wibom R. Suppression of sleepiness and melatonin by bright light exposure during breaks in night work. J Sleep Res. 2004 Mar; 13(1): 37-43. | CrossRef | PubMed |
Lowden A, Akerstedt T, Wibom R. Suppression of sleepiness and melatonin by bright light exposure during breaks in night work. J Sleep Res. 2004 Mar; 13(1): 37-43. | CrossRef | PubMed | Howard ME, Radford L, Jackson ML, Swann P, Kennedy GA. The effects of a 30-minute napping opportunity during an actual night shift on performance and sleepiness in shift workers. Biol Rhythm Res. 2010; 41(2): 137-48. | CrossRef |
Howard ME, Radford L, Jackson ML, Swann P, Kennedy GA. The effects of a 30-minute napping opportunity during an actual night shift on performance and sleepiness in shift workers. Biol Rhythm Res. 2010; 41(2): 137-48. | CrossRef | Smith A, Kilby S, Jorgensen G,Douglas J. Napping and nightshift work: Effects of a short nap on psychomotor vigilance and subjective sleepiness in health workers. Sleep Biol. Rhythms. 2007 Abr; 5(2): 117-25. | CrossRef |
Smith A, Kilby S, Jorgensen G,Douglas J. Napping and nightshift work: Effects of a short nap on psychomotor vigilance and subjective sleepiness in health workers. Sleep Biol. Rhythms. 2007 Abr; 5(2): 117-25. | CrossRef | Atlantis E, Chow CM, Kirby A, Singh MA. Worksite intervention effects on sleep quality: a randomized controlled trial. J Occup Health Psychol. 2006 Oct; 11(4): 291-304. | CrossRef | PubMed |
Atlantis E, Chow CM, Kirby A, Singh MA. Worksite intervention effects on sleep quality: a randomized controlled trial. J Occup Health Psychol. 2006 Oct; 11(4): 291-304. | CrossRef | PubMed | Rodríguez-León DL, Garzón-Molina NM. Comparación de las intervenciones en actividad física en Brasil y Colombia, desde la promoción de la salud. Rev Fac Med. 2013; 61(4): 449-58. [Internet] | Link |
Rodríguez-León DL, Garzón-Molina NM. Comparación de las intervenciones en actividad física en Brasil y Colombia, desde la promoción de la salud. Rev Fac Med. 2013; 61(4): 449-58. [Internet] | Link | Granada-Echeverri P, Zapata-Valencia CD, Giraldo-Trujillo JC. Impacto de un modelo de movilización social sobre la promoción de la actividad física en afiliados al sistema de seguridad social en salud. Rev Salud Pública. 2008 Jul; 10(3): 361-73. [Internet] | Link |
Granada-Echeverri P, Zapata-Valencia CD, Giraldo-Trujillo JC. Impacto de un modelo de movilización social sobre la promoción de la actividad física en afiliados al sistema de seguridad social en salud. Rev Salud Pública. 2008 Jul; 10(3): 361-73. [Internet] | Link | Valdivia LM, Lam C, Mucha R, Chávez J, Tanta J, Alvarezcano J, et al. Impacto de un programa de capacitación para la prevención de infecciones intrahospitalarias en un hospital general. Trauma Fund MAPFRE. 2013; 24(2): 126-31. [Internet] | Link |
Valdivia LM, Lam C, Mucha R, Chávez J, Tanta J, Alvarezcano J, et al. Impacto de un programa de capacitación para la prevención de infecciones intrahospitalarias en un hospital general. Trauma Fund MAPFRE. 2013; 24(2): 126-31. [Internet] | Link | Keynejad R, Semrau M, Toynbee M, Evans-Lacko S, Lund C, Gureje O, et al. Building the capacity of policy-makers and planners to strengthen mental health systems in low- and middle-income countries: a systematic review. BMC Health Serv Res. 2016 Oct; 16(1): 601. | CrossRef | PubMed |
Keynejad R, Semrau M, Toynbee M, Evans-Lacko S, Lund C, Gureje O, et al. Building the capacity of policy-makers and planners to strengthen mental health systems in low- and middle-income countries: a systematic review. BMC Health Serv Res. 2016 Oct; 16(1): 601. | CrossRef | PubMed | García P, Hughes J, Carcamo C, Holmes K. Training pharmacy workers in recognition, management, and prevention of STDs: district-randomized controlled trial. Bull World Health Organ. 2003; 81(11): 806-14. | PubMed |
García P, Hughes J, Carcamo C, Holmes K. Training pharmacy workers in recognition, management, and prevention of STDs: district-randomized controlled trial. Bull World Health Organ. 2003; 81(11): 806-14. | PubMed | Amaral E, Campos HH, Friedman S, Morahan PS, Araujo MN, Carvalho PM, et al. An educational international partnership responding to local needs: Process evaluation of the Brazil FAIMER Regional Institute. Educ Health (Abingdon). 2012 Nov; 25(2): 116-23. | CrossRef | PubMed |
Amaral E, Campos HH, Friedman S, Morahan PS, Araujo MN, Carvalho PM, et al. An educational international partnership responding to local needs: Process evaluation of the Brazil FAIMER Regional Institute. Educ Health (Abingdon). 2012 Nov; 25(2): 116-23. | CrossRef | PubMed | Bellón JA, Conejo-Cerón S, Moreno-Peral P, King M, Nazareth I, Martín-Pérez C, et al. Preventing the onset of major depression based on the level and profile of risk of primary care attendees: protocol of a cluster randomised trial (the predictD-CCRT study). BMC Psychiatry. 2013 Jun; 13(171): 1-16. | CrossRef | PubMed |
Bellón JA, Conejo-Cerón S, Moreno-Peral P, King M, Nazareth I, Martín-Pérez C, et al. Preventing the onset of major depression based on the level and profile of risk of primary care attendees: protocol of a cluster randomised trial (the predictD-CCRT study). BMC Psychiatry. 2013 Jun; 13(171): 1-16. | CrossRef | PubMed | Ramos-Morcillo AJ, Fernández-Salazar S, Ruzafa-Martínez M, Del Pino-Casado R. Effectiveness of a brief, basic evidence‐based practice course for clinical nurses. Worldviews Evid Based Nurs. 2015 Aug; 12(4): 199–207. | CrossRef | PubMed |
Ramos-Morcillo AJ, Fernández-Salazar S, Ruzafa-Martínez M, Del Pino-Casado R. Effectiveness of a brief, basic evidence‐based practice course for clinical nurses. Worldviews Evid Based Nurs. 2015 Aug; 12(4): 199–207. | CrossRef | PubMed | Kringos DS, Sunol R, Wagner C, Mannion R, Michel P, Klazinga NS, at al. The influence of context on the effectiveness of hospital quality improvement strategies: a review of systematic reviews. BMC Health Serv Res. 2015 Jul; 15(277): 1-13. | CrossRef | PubMed |
Kringos DS, Sunol R, Wagner C, Mannion R, Michel P, Klazinga NS, at al. The influence of context on the effectiveness of hospital quality improvement strategies: a review of systematic reviews. BMC Health Serv Res. 2015 Jul; 15(277): 1-13. | CrossRef | PubMed | Greenfield D, Braithwaite J. Health sector accreditation research: a systematic review. Int J Qual Health Care. 2008 Jun; 20(1): 172-83. | CrossRef | PubMed |
Greenfield D, Braithwaite J. Health sector accreditation research: a systematic review. Int J Qual Health Care. 2008 Jun; 20(1): 172-83. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








