Key Words: hip arthroplasty, knee arthroplasty, osteoarthritis, epidemiology, survival analysis
Abstract
Background
The purpose of this study is to determine if patients with osteoarthritis that undergo hip or knee arthroplasty jeopardize their life expectancy in Chile.
Methods
A survival analysis study was designed and approved by our institutional ethics review board. Patients were included if they underwent surgery for hip or knee osteoarthritis and were 50 years or older at the time of surgery. Patients were excluded if arthroplasty was performed for fracture, hemophilia arthropathy, or tumor. A multiparametric Weibull regression was estimated, and the hazard ratio was reported. For internal validity, a bootstrap of 200 repetitions was performed.
Results
A total of 4 094 arthroplasties were included. The Kaplan-Meier curve estimates a higher survival than the general population up to 12 years, after which the median survival is less than the general population. The bootstrap multiparametric Weibull regression estimated a hazard ratio of 1.53 (95% confidence interval: 1.27 to 1.84) for women, 1.09 (1.08 to 1.10) for every year older, and 1.29 (1.07 to 1.53) for hip arthroplasty patients.
Conclusion
Mortality after hip and knee arthroplasty in Chile follows a bimodal behavior similar to reports from the United States and Europe. At first, mortality is lower than the general population but worsens after 12 to 15 years of surgery.
Main messages
|
Introduction
Osteoarthrosis is a frequent disease that causes pain, disability, and diminished quality of life. The most common compromised joint is the knee, followed by the hand and the hip[1]. Hip arthroplasty has been touted as the main surgery of the XXth century due to the impact it has had on patients' functionality and quality of life[2]. Knee arthroplasty indication has been increasing throughout this century, establishing it as a cost-effective treatment for knee osteoarthritis[3].
Implant survival has been widely studied. A recent systematic review has shown that the 25-year survival rate of hip prosthesis is 58%[4], and for knee prosthesis, the 20-year survival rate is above 80%[5]. Nevertheless, fewer studies have addressed the impact on patient’s survival compared to the general population; moreover, the results do not readily extrapolate to Chile or Latin-American reality due to many factors, among the most important might be the diversity of socioeconomic status[6]. A study carried out in the United States reported that survival after hip or knee arthroplasty had a bimodal behavior: initially greater survival than the general population and after 15 years, higher mortality than the general population[7]. A previous study performed in Sweden reported the same bimodal pattern, but the shift was at 12 years[8]. Similarly, a study performed in Denmark reported higher survival than the general population at a maximum follow-up of 12 years[9].
Patients before surgery commonly ask about mortality related to the procedure and their life expectancy after arthroplasty. The purpose of this study is to determine if patients with osteoarthritis that undergo hip or knee replacement jeopardize their life expectancy in Chile.
Methods
A survival analysis study was designed and approved by our institutional ethics review board. The patients were recruited from two general hospitals in Santiago, Chile: Hospital San Jose and Hospital Clínico Universidad de Chile. Both centers have access to the same type and brands of prostheses, and surgeons have a similar level of training; moreover, two of them work in both centers. The first hospital belongs to the public network of health centers, so all patients treated were affiliated to the public insurance, known as the National Health Fund. A public university owns the other center, and about half of the patients that received medical treatment were affiliated to the National Health Fund.
A search was conducted in both institutions using the National Health Fund code that identifies each procedure (2104129-11 for hip arthroplasty and 2104153-10 for knee arthroplasty). Patients were included if they underwent surgery for severe hip or knee osteoarthritis and were 50 years or older by the time of surgery. Patients were excluded if arthroplasty was performed for fracture, hemophilic arthropathy, or tumor. Also, revision arthroplasties were excluded. The review was done in the university hospital between January 1, 2002, to December 31, 2019, while the public hospital review was done from June 1, 2011, to February 29, 2020. Unfortunately, data before 2012 were not available. The flow chart of patient selection is shown in Figure 1. The patient’s full name, national ID number, gender, birth date, date of admission, date of discharge, surgery code, and surgery date were recorded. Patients with incomplete information were excluded. Then, by the National Transparency Act, we requested the National Civil Registry of Chile to inform whether the patients were alive by March 30, 2020; if deceased, they were asked to report the date of death.
Figure 1. Patient selection flow chart.
Continuous variables were summarized in median, range, and interquartile range (IQR, p25–p75). Absolute frequency and percent were used to describe discrete variables. The unmatched nonparametric median test was used to compare continuous variables, and Fisher’s exact test was used to compare discrete variables. A p-value of < 0.05 was interpreted as significant.
For survival analyses, the initial time (t0) was the date of surgery. The final follow-up was March 30, 2020, and failure was defined as death by any cause. Total time at risk, the annual incidence of death and the percentile of survival time were reported for hip arthroplasty and knee arthroplasty. A multiparametric regression was estimated, Weibull exponential and log-normal distribution were tested. The distribution that had the best fit model was determined using log-likelihood, the relation between Cox-Snell residual and Nelson Aalen cumulative hazard, and the linear relation between the natural logarithm of the survival probability and the analyzed time. The hazard ratio is reported. For internal validity, a bootstrap of 200 repetitions was performed. The covariables were tested using the Wald test, and the power of each hazard ratio was calculated
The 2016 publication of the Statistics National Institute of Chile (INE)[10] was used to compare this estimation to the expectancy of life of the general Chilean population, reported in groups of five years. The age of the cohort included in the study was grouped forming four groups: 50 to 59, 60 to 69, 70 to 79, and 80 years or older. Each group was compared to the adjusted expectancy of life by age and gender for the general population, assuming an exponential distribution.
A significance of 5% was used, and a 95% confidence interval were estimated. The data were processed using Stata version 15 (StataCorp LP, College Station, Texas, USA).
Results
A total of 4 094 arthroplasties were included, of which 1 733 were knee arthroplasty replacements (42.3%), and 2 361 were hip replacements (57.7%). The median age was 67 years old (range, 50 to 97; interquartile range, 60 to 74), and 2 602 (63.6%) were female patients. Patients that underwent knee arthroplasty were significantly older than hip arthroplasty patients. Also, a significantly higher proportion of women was found in the hip arthroplasty group. During the period studied, a total of 462 patients died after arthroplasty (11.3%) (Table 1).
The median follow-up was 4.98 years (interquartile range, 2.25 to 8.43). Follow-up was significantly longer in the hip arthroplasty patients (Table 1). The lethality at 30 days, six months, and one year were higher in the hip arthroplasty group, reaching a statistical difference.
The total time at risk was 24 035 years, with an incidence rate of death by year of 0.019. The 25 percentile of survival time was 12.75 years. In the hip arthroplasty patients, the incidence of death by year was 0.021, and in the knee arthroplasty was 0.179. The 25 percentile of survival time was 12.90 years in hip arthroplasty patients and 11.89 years in knee arthroplasty patients. The total time at risk, the incidence of death and the median survival time percentile are summarized in Tables 2 and 3. The Kaplan-Meir survival curve was estimated knee arthroplasty and hip arthroplasty compared to the adjusted general population survival showing bimodal mortality. The Kaplan-Meier curve estimates a higher survival than the general population at up to 12 years, after which the median survival is less than that of the general population (Figure 2).
Figure 2. Kaplan-Meier survival estimate compared to the general population adjusted by age and sex.
The Weibull distribution was the best fit. The bootstrap multiparametric Weibull regression estimated a hazard ratio of 1.53 (95% confidence interval: 1.27 to 1.84) for women, a hazard ratio of 1.09 (95% confidence interval: 1.08 to 1.10) for every year older, a hazard ratio of 1.29 (95% confidence interval: 1.07 to 1.53) for hip arthroplasty. The parameter of the Weibull regression was 1.38 (95% confidence interval: 1.24 to 1.53), meaning a significant increase of risk of death by year after arthroplasty to a rate of 32% annually (95% confidence interval: 0.22 to 0.43), Wald test was significant p = 0.000, and the power for each hazard ratio was 0.99. The institution where the surgery was performed was not significant in long-term survival (hazard ratio 0.96; 95% confidence interval: 0.81 to 1.15).
The Weibull estimation shows that knee arthroplasty and hip arthroplasty patients between 50 and 69 live at least 17 years longer than the general population (Figures 3 and 4). Meanwhile, patients over 70 years had a lower life expectancy 15 years after surgery (Figure 5). Also, patients above 80 years old had higher life expectancy than the general population until four years after surgery (Figure 6).
Figure 6. Survival curve for male and female patients 80 years or older that undergo arthroplasty.
Discussion
This study’s main finding shows that patients under 80 years old who undergo hip arthroplasty or knee arthroplasty do not compromise their life expectancy for the first 15 years after surgery, at least, which is consistent with the previous studies that report lower mortality than the general population during the first 12 to 15 years after surgery[7],[8],[9]. However, after this period of more prolonged survival, mortality was higher than the general population. This bimodal pattern was more abrupt in the population over 70 years. This bimodal pattern is similar to that reported in studies in the United States and Sweden, where the shift occurred between 12 and 15 years[7],[8].
The causes of this bimodal pattern are yet to be determined. The initial lower mortality is associated with patient selection, where patients that undergo arthroplasty must ascertain health status, and cardiovascular disease must be ruled out[7]. Moreover, patients that underwent successful arthroplasty achieved pain relief, which has been related to a higher life expectancy[11]. On the other hand, the increased mortality may be due to the increased risk of cardiovascular disease in patients with osteoarthritis compared to the general population. Patients with osteoarthritis have a 24% increased risk of developing cardiovascular disease, a relative risk of 2.80 (95% confidence interval: 2.25 to 3.49) to have heart failure, and a relative risk of 1.78 (95% confidence interval: 1.18 to 2.69) to have ischemic heart disease[12],[13]. This is supported by Swedish registry findings, where the leading cause of death in patients with osteoarthritis was cardiovascular disease[8]. Patients who have required a hip or knee prosthesis should be encouraged to follow routine controls for cardiovascular disease.
No difference in lethality after arthroplasty between the university and the public hospital was found in this study. Both centers were compared for lethality after hip fracture, and a higher lethality was found in the public center[14]. Therefore, socioeconomics and type of health insurance (public or private) play a minimum role in the bimodal behavior found in these patients, unlike hip fracture patients.
The time gap is shorter between the initial increase in survival and the later increase in mortality. Cardiovascular diseases are more prevalent as age increases, explaining the shorter gap of higher survival rates than the general population[15].
A significant hazard ratio in favor of knee replacement was found in this study. A patient undergoing hip replacement due to secondary osteoarthritis [hip dysplasia, inflammatory arthritis, and femoral head necrosis] does not achieve less mortality than the general population at any time[16]. Also, a significant proportion of knee procedures included in this study were done after 2012, so compared to an increased proportion of patients that underwent hip replacement before 2012, the comparison is uneven. An explosive increase in knee replacement procedures has been described in the last decades, and our cohort was not an exception[17],[18],[19]. Maradit-Kremers et al. demonstrate that comparing mortality rates between decades in patients that underwent arthroplasty is significantly different[7]. This could be explained by patients who underwent arthroplasty for femoral head necrosis or hip dysplasia, which were not an exclusion criterion in this study.
The findings in the over 80 years old cohort should encourage an interdisciplinary approach to diminish mortality after arthroplasty. Orthogeriatric should move forward from hip fracture to arthroplasty care[20]. Programs with good results have been reported in patients over 89 years old, reaching a better higher survival rate than the general population at four years follow up[21]. For knee osteoarthritis, unicompartmental arthroplasty is less invasive than total knee with similar functional and survival outcomes in patients over 75 years old[22],[23]. It could be that this less aggressive procedure tends to lower mortality rates in elderly patients.
This study has some limitations. The sample size is smaller and has a shorter follow up than the reports from the United States and Europe; nevertheless, the mortality trend is comparable. Also, the estimated regression model with good internal validity and high-power estimation of each hazard ratio minimizes the possible bias arising from the sample size.
Another limitation of this study is that the specific cause of mortality is unknown, so for example, a patient could have a hip arthroplasty performed but died because of lung cancer. Nevertheless, the number of patients studied minimizes this bias.
In addition, this study has a limitation in that the overall data were extracted from two hospitals and might differ in other regions of Chile or countries in Latin America. Nevertheless, the results obtained compared similarly to international reports, and there was no difference between public and private health institutions, making the results more generalizable.
Conclusion
Mortality after hip and knee arthroplasty in Chile follows a similar bimodal behavior over the years to reports from the United States and Europe. First, lower mortality than the general population is expected, but patients have increased mortality approximately after 12 to 15 years. The time gap is shorter in patients over 80 years, so this patient age-group must be carefully selected and adequately followed to optimize the results of this surgery; an interdisciplinary approach is mandatory. The risk of death after arthroplasty surgery is not constant and increases 0.32 by year. The survival rate after arthroplasty in this cohort of Chilean patients is similar to international reports.
Notes
Acknowledgments
The first author acknowledges the unconditional support of Leonel Barahona.
Roles and contributions of authorship
MB: Conceptualization, methodology, formal analysis, Investigation, data curation, writing (original draft preparation) and project administration. CB: Methodology, investigation, writing (review and editing), supervision and visualization. AM: Investigation, resources, writing (review and editing). JB: Investigation, resources, data curation, writing (original draft preparation). JPP: Data curation, investigation and writing (original draft preparation). JH: Validation, resources, investigation and writing (review and editing).
Conflict of interest
The authors declare that they have no competing interests.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Hospital Clínico Universidad de Chile ethics research board, as stated in certificate number 32, issued on July 1, 2020.
Availability of data
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Language of original submission
Submitted and peer-reviewed in English.

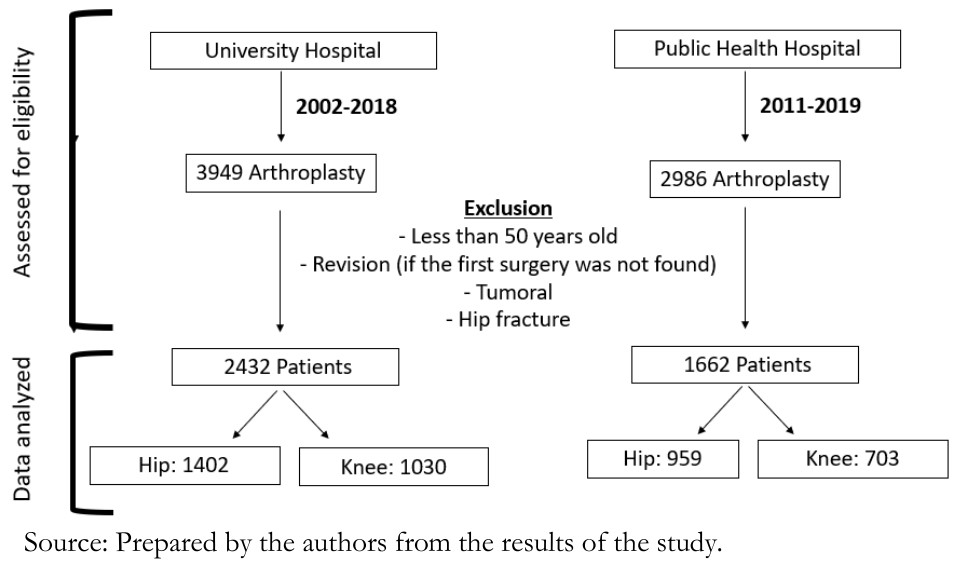 Figure 1. Patient selection flow chart.
Figure 1. Patient selection flow chart.

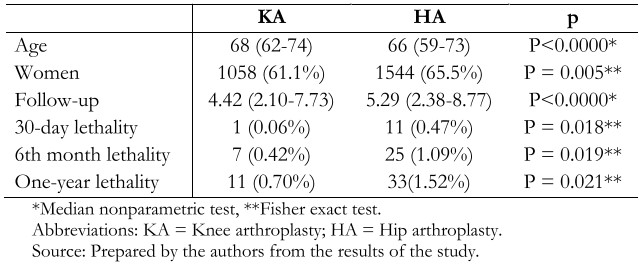 Table 1. Summary by type of arthroplasty, the median age, the proportion of women, median follow-up, 30-day, six-month, and one-year lethality. All variables reached a significant difference.
Table 1. Summary by type of arthroplasty, the median age, the proportion of women, median follow-up, 30-day, six-month, and one-year lethality. All variables reached a significant difference.

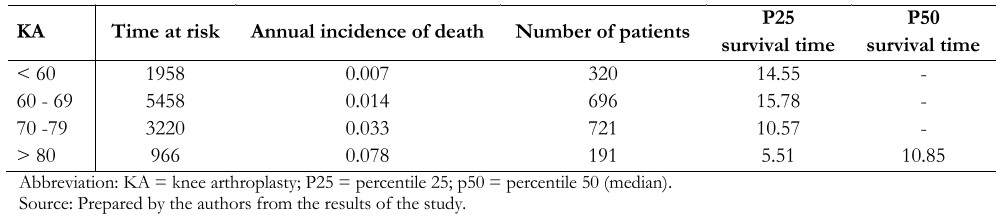 Table 2. The time at risk, the annual incidence of death, and the percentile of survival time in knee arthroplasty patients.
Table 2. The time at risk, the annual incidence of death, and the percentile of survival time in knee arthroplasty patients.

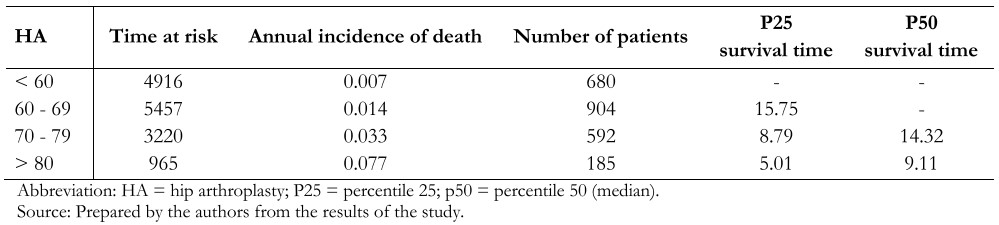 Table 3. The time at risk, the annual incidence of death, and the percentile of survival time in hip arthroplasty patients.
Table 3. The time at risk, the annual incidence of death, and the percentile of survival time in hip arthroplasty patients.

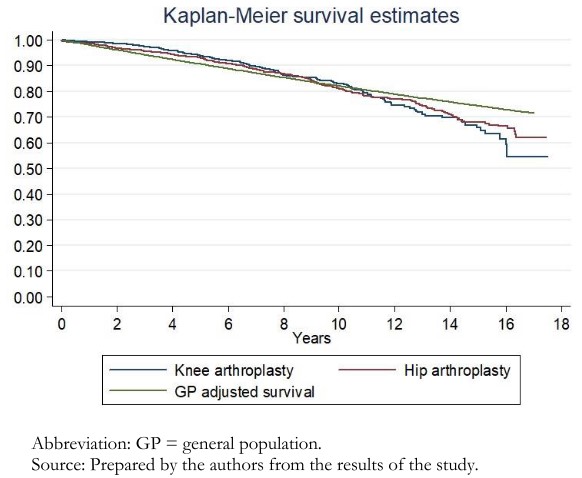 Figure 2. Kaplan-Meier survival estimate compared to the general population adjusted by age and sex.
Figure 2. Kaplan-Meier survival estimate compared to the general population adjusted by age and sex.

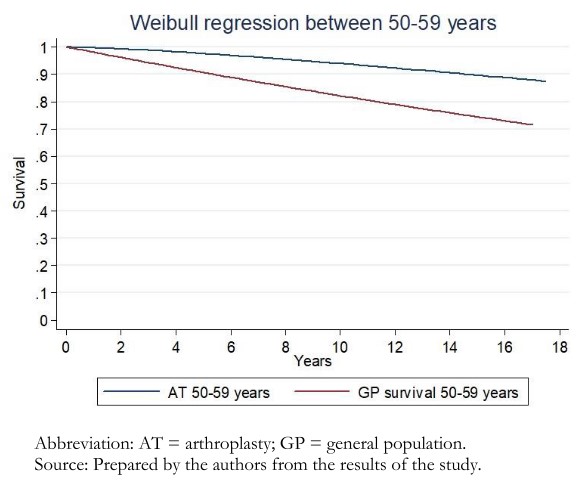 Figure 3. Survival curve after multiparametric bootstrap Weibull regression for patients between 50 to 59 years old that undergo arthroplasty.
Figure 3. Survival curve after multiparametric bootstrap Weibull regression for patients between 50 to 59 years old that undergo arthroplasty.

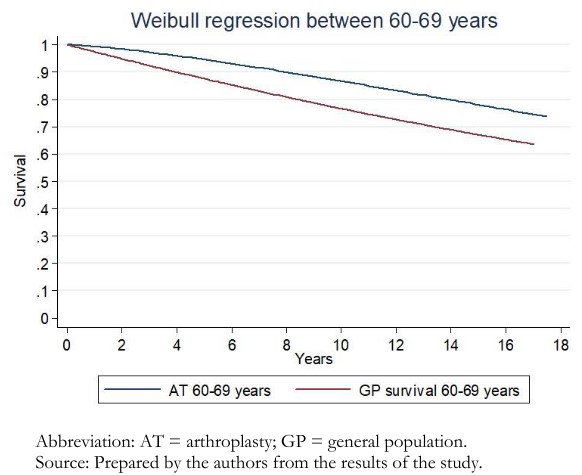 Figure 4. Survival curve after multiparametric bootstrap Weibull regression for patients between 60 to 69 years old that undergo arthroplasty.
Figure 4. Survival curve after multiparametric bootstrap Weibull regression for patients between 60 to 69 years old that undergo arthroplasty.

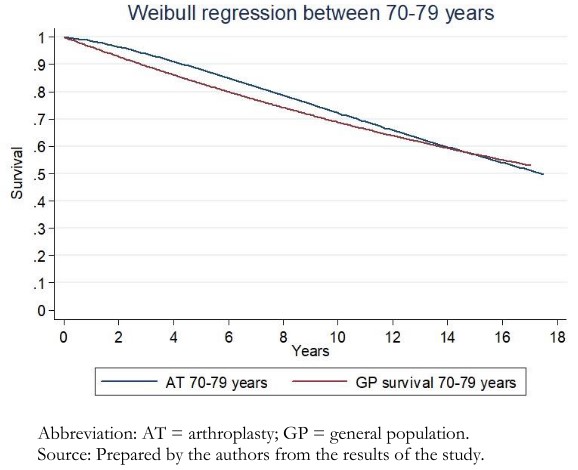 Figure 5. Survival curve after multiparametric bootstrap Weibull regression for patients between 70 to 79 years old that undergo arthroplasty.
Figure 5. Survival curve after multiparametric bootstrap Weibull regression for patients between 70 to 79 years old that undergo arthroplasty.

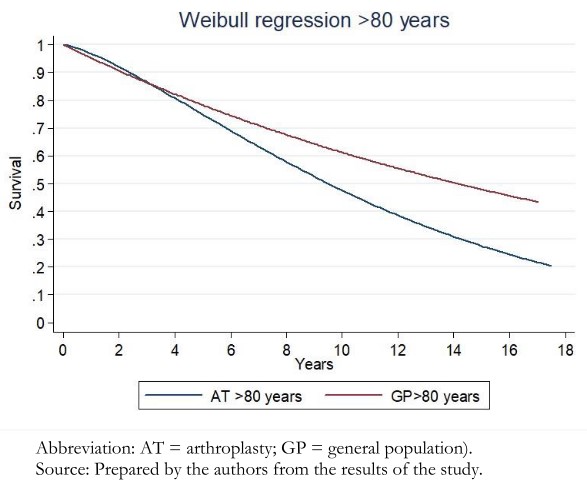 Figure 6. Survival curve for male and female patients 80 years or older that undergo arthroplasty.
Figure 6. Survival curve for male and female patients 80 years or older that undergo arthroplasty.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introducción
El propósito de este estudio es determinar si los pacientes con artrosis severa intervenidos con artroplastia de rodilla o cadera ponen en riesgo su expectativa de vida.
Método
Se diseñó un estudio de sobrevida el cual fue aprobado por el comité de ética de nuestra institución. Los pacientes fueron incluidos si fueron intervenidos de artroplastia de rodilla y cadera por artrosis severa y tenían más de 50 años. Los pacientes fueron excluidos si la artroplastia se realizó por fractura, hemofilia o un tumor. Una regresión multiparamétrica de Weibull fue estimada, siendo reportado el hazard ratio. Un bootstrap de 200 repeticiones fue realizada para validación interna.
Resultados
Un total de 4094 artroplastias fueron incluidos. La curva de Kaplan-Meier estima una mayor sobrevida que la población general hasta los 12 años, luego de lo cual la mediana de sobrevida es menor que la de la población general. La regresión multiparamétrica de Weibull estimó hazard ratios de 1,53 (intervalo de confianza 95%: 1,27 a 1,84) en mujeres, de 1,09 (1,08 a 1,10) por cada año de edad y de 1,29 (1,07 a 1,53) en artroplastia de cadera.
Conclusión
La mortalidad después de una intervención de artroplastia de rodilla o cadera sigue un comportamiento bimodal respecto a la población general similar a series reportadas en Estados Unidos y Suecia. Inicialmente la sobrevida es mayor que la población general, pero es menor luego de 12 a 15 años.
 Authors:
Maximiliano Barahona[1], Cristian Barrientos[1,2], Álvaro Martinez[2], Julián Brañes[1,2], Juan Pablo Prieto[1], Jaime Hinzpeter[1]
Authors:
Maximiliano Barahona[1], Cristian Barrientos[1,2], Álvaro Martinez[2], Julián Brañes[1,2], Juan Pablo Prieto[1], Jaime Hinzpeter[1]
Affiliation:
[1] Departamento de Ortopedia y Traumatología en Hospital Clínico Universidad de Chile, Santiago, Chile
[2] Departamento de Ortopedia y Traumatología en Hospital San José, Santiago, Chile
E-mail: maxbarahonavasquez@gmail.com
Author address:
[1] Santos Dumont 999, 3rd Floor, office 351 Postal code 8380456, Independencia, Santiago, Chile

Citation: Barahona M, Barrientos C, Martinez A, Brañes J, Prieto JP, Hinzpeter J. Mortality after hip or knee arthroplasty for osteoarthritis in Chile: A survival analysis. Medwave 2020;20(11):e8088 doi: 10.5867/medwave.2020.11.8088
Submission date: 11/7/2020
Acceptance date: 3/11/2020
Publication date: 17/12/2020
Origin: Not commissioned
Type of review: Externally peer-reviewed by three reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019 Apr 27;393(10182):1745-1759. | CrossRef | PubMed |
- Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007 Oct 27;370(9597):1508-19. | CrossRef | PubMed |
- Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, et al. Knee replacement. Lancet. 2018 Nov 3;392(10158):1672-1682. | CrossRef | PubMed |
- Evans JT, Evans JP, Walker RW, Blom AW, Whitehouse MR, Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019 Feb 16;393(10172):647-654. | CrossRef | PubMed |
- Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019 Feb 16;393(10172):655-663. | CrossRef | PubMed |
- Bilal U, Alazraqui M, Caiaffa WT, Lopez-Olmedo N, Martinez-Folgar K, Miranda JJ, et al. Inequalities in life expectancy in six large Latin American cities from the SALURBAL study: an ecological analysis. Lancet Planet Health. 2019 Dec;3(12):e503-e510. | CrossRef | PubMed |
- Maradit Kremers H, Larson DR, Noureldin M, Schleck CD, Jiranek WA, Berry DJ. Long-Term Mortality Trends After Total Hip and Knee Arthroplasties: A Population-Based Study. J Arthroplasty. 2016 Jun;31(6):1163-1169. | CrossRef | PubMed |
- Robertsson O, Stefánsdóttir A, Lidgren L, Ranstam J. Increased long-term mortality in patients less than 55 years old who have undergone knee replacement for osteoarthritis: results from the Swedish Knee Arthroplasty Register. J Bone Joint Surg Br. 2007 May;89(5):599-603. | CrossRef | PubMed |
- Pedersen AB, Baron JA, Overgaard S, Johnsen SP. Short- and long-term mortality following primary total hip replacement for osteoarthritis: a Danish nationwide epidemiological study. J Bone Joint Surg Br. 2011 Feb;93(2):172-7. | CrossRef | PubMed |
- Villalon GC, Schneider SV, Ortega FC. Chile, tabla de vida por método de mortalidad óptima. Santiago, Chile: Instituto Nacional de Estadistica de Chile; 2016. [On line]. | Link |
- Zimmer Z, Rubin S. Life Expectancy With and Without Pain in the U.S. Elderly Population. J Gerontol A Biol Sci Med Sci. 2016 Sep;71(9):1171-6. | CrossRef | PubMed |
- Hall AJ, Stubbs B, Mamas MA, Myint PK, Smith TO. Association between osteoarthritis and cardiovascular disease: Systematic review and meta-analysis. Eur J Prev Cardiol. 2016 Jun;23(9):938-46. | CrossRef | PubMed |
- Wang H, Bai J, He B, Hu X, Liu D. Osteoarthritis and the risk of cardiovascular disease: a meta-analysis of observational studies. Sci Rep. 2016 Dec 22;6:39672. | CrossRef | PubMed |
- Barahona M, Martinez Á, Barrientos C, Cavada G, Brañes J, Palet M, et al. Survival Analysis after Hip Fracture in Chile in Patients Over 50 Years Old: A Comparative Analysis between a Private and a Public Health Center. SSRN Electron J. 2019. [On line]. | Link |
- Weber M, Völlner F, Benditz A, Schwarz T, Wörner M, Craiovan B, et al. Kniegelenkersatz des älteren Menschen [Total knee arthroplasty in the elderly]. Orthopade. 2017 Jan;46(1):34-39. | CrossRef | PubMed |
- Cnudde P, Rolfson O, Timperley AJ, Garland A, Kärrholm J, Garellick G, et al. Do Patients Live Longer After THA and Is the Relative Survival Diagnosis-specific? Clin Orthop Relat Res. 2018 Jun;476(6):1166-1175. | CrossRef | PubMed |
- Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: Annual Report 2017. Adelaide: AOA; 2017. [On line]. | Link |
- Karrholm J, Rogmark C, Nauclér E, Vinblad J, Mohaddes M, Rolfson O. Swedish Hip Arthroplasty Register: Annual Report 2018. 2018. [On line]. | Link |
- National institute for health and Welfare. Finnish arthroplasty register. [On line]. | Link |
- Aw D, Sahota O. Orthogeriatrics moving forward. Age Ageing. 2014 May;43(3):301-5. | CrossRef | PubMed |
- Berend ME, Thong AE, Faris GW, Newbern G, Pierson JL, Ritter MA. Total joint arthroplasty in the extremely elderly: hip and knee arthroplasty after entering the 89th year of life. J Arthroplasty. 2003 Oct;18(7):817-21. | CrossRef | PubMed |
- Fabre-Aubrespy M, Ollivier M, Pesenti S, Parratte S, Argenson JN. Unicompartmental Knee Arthroplasty in Patients Older Than 75 Results in Better Clinical Outcomes and Similar Survivorship Compared to Total Knee Arthroplasty. A Matched Controlled Study. J Arthroplasty. 2016 Dec;31(12):2668-2671. | CrossRef | PubMed |
- Siman H, Kamath AF, Carrillo N, Harmsen WS, Pagnano MW, Sierra RJ. Unicompartmental Knee Arthroplasty vs Total Knee Arthroplasty for Medial Compartment Arthritis in Patients Older Than 75 Years: Comparable Reoperation, Revision, and Complication Rates. J Arthroplasty. 2017 Jun;32(6):1792-1797. | CrossRef | PubMed |
 Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019 Apr 27;393(10182):1745-1759. | CrossRef | PubMed |
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019 Apr 27;393(10182):1745-1759. | CrossRef | PubMed | Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007 Oct 27;370(9597):1508-19. | CrossRef | PubMed |
Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007 Oct 27;370(9597):1508-19. | CrossRef | PubMed | Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, et al. Knee replacement. Lancet. 2018 Nov 3;392(10158):1672-1682. | CrossRef | PubMed |
Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, et al. Knee replacement. Lancet. 2018 Nov 3;392(10158):1672-1682. | CrossRef | PubMed | Evans JT, Evans JP, Walker RW, Blom AW, Whitehouse MR, Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019 Feb 16;393(10172):647-654. | CrossRef | PubMed |
Evans JT, Evans JP, Walker RW, Blom AW, Whitehouse MR, Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019 Feb 16;393(10172):647-654. | CrossRef | PubMed | Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019 Feb 16;393(10172):655-663. | CrossRef | PubMed |
Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019 Feb 16;393(10172):655-663. | CrossRef | PubMed | Bilal U, Alazraqui M, Caiaffa WT, Lopez-Olmedo N, Martinez-Folgar K, Miranda JJ, et al. Inequalities in life expectancy in six large Latin American cities from the SALURBAL study: an ecological analysis. Lancet Planet Health. 2019 Dec;3(12):e503-e510. | CrossRef | PubMed |
Bilal U, Alazraqui M, Caiaffa WT, Lopez-Olmedo N, Martinez-Folgar K, Miranda JJ, et al. Inequalities in life expectancy in six large Latin American cities from the SALURBAL study: an ecological analysis. Lancet Planet Health. 2019 Dec;3(12):e503-e510. | CrossRef | PubMed | Maradit Kremers H, Larson DR, Noureldin M, Schleck CD, Jiranek WA, Berry DJ. Long-Term Mortality Trends After Total Hip and Knee Arthroplasties: A Population-Based Study. J Arthroplasty. 2016 Jun;31(6):1163-1169. | CrossRef | PubMed |
Maradit Kremers H, Larson DR, Noureldin M, Schleck CD, Jiranek WA, Berry DJ. Long-Term Mortality Trends After Total Hip and Knee Arthroplasties: A Population-Based Study. J Arthroplasty. 2016 Jun;31(6):1163-1169. | CrossRef | PubMed | Robertsson O, Stefánsdóttir A, Lidgren L, Ranstam J. Increased long-term mortality in patients less than 55 years old who have undergone knee replacement for osteoarthritis: results from the Swedish Knee Arthroplasty Register. J Bone Joint Surg Br. 2007 May;89(5):599-603. | CrossRef | PubMed |
Robertsson O, Stefánsdóttir A, Lidgren L, Ranstam J. Increased long-term mortality in patients less than 55 years old who have undergone knee replacement for osteoarthritis: results from the Swedish Knee Arthroplasty Register. J Bone Joint Surg Br. 2007 May;89(5):599-603. | CrossRef | PubMed | Pedersen AB, Baron JA, Overgaard S, Johnsen SP. Short- and long-term mortality following primary total hip replacement for osteoarthritis: a Danish nationwide epidemiological study. J Bone Joint Surg Br. 2011 Feb;93(2):172-7. | CrossRef | PubMed |
Pedersen AB, Baron JA, Overgaard S, Johnsen SP. Short- and long-term mortality following primary total hip replacement for osteoarthritis: a Danish nationwide epidemiological study. J Bone Joint Surg Br. 2011 Feb;93(2):172-7. | CrossRef | PubMed | Villalon GC, Schneider SV, Ortega FC. Chile, tabla de vida por método de mortalidad óptima. Santiago, Chile: Instituto Nacional de Estadistica de Chile; 2016. [On line]. | Link |
Villalon GC, Schneider SV, Ortega FC. Chile, tabla de vida por método de mortalidad óptima. Santiago, Chile: Instituto Nacional de Estadistica de Chile; 2016. [On line]. | Link | Zimmer Z, Rubin S. Life Expectancy With and Without Pain in the U.S. Elderly Population. J Gerontol A Biol Sci Med Sci. 2016 Sep;71(9):1171-6. | CrossRef | PubMed |
Zimmer Z, Rubin S. Life Expectancy With and Without Pain in the U.S. Elderly Population. J Gerontol A Biol Sci Med Sci. 2016 Sep;71(9):1171-6. | CrossRef | PubMed | Hall AJ, Stubbs B, Mamas MA, Myint PK, Smith TO. Association between osteoarthritis and cardiovascular disease: Systematic review and meta-analysis. Eur J Prev Cardiol. 2016 Jun;23(9):938-46. | CrossRef | PubMed |
Hall AJ, Stubbs B, Mamas MA, Myint PK, Smith TO. Association between osteoarthritis and cardiovascular disease: Systematic review and meta-analysis. Eur J Prev Cardiol. 2016 Jun;23(9):938-46. | CrossRef | PubMed | Wang H, Bai J, He B, Hu X, Liu D. Osteoarthritis and the risk of cardiovascular disease: a meta-analysis of observational studies. Sci Rep. 2016 Dec 22;6:39672. | CrossRef | PubMed |
Wang H, Bai J, He B, Hu X, Liu D. Osteoarthritis and the risk of cardiovascular disease: a meta-analysis of observational studies. Sci Rep. 2016 Dec 22;6:39672. | CrossRef | PubMed | Barahona M, Martinez Á, Barrientos C, Cavada G, Brañes J, Palet M, et al. Survival Analysis after Hip Fracture in Chile in Patients Over 50 Years Old: A Comparative Analysis between a Private and a Public Health Center. SSRN Electron J. 2019. [On line]. | Link |
Barahona M, Martinez Á, Barrientos C, Cavada G, Brañes J, Palet M, et al. Survival Analysis after Hip Fracture in Chile in Patients Over 50 Years Old: A Comparative Analysis between a Private and a Public Health Center. SSRN Electron J. 2019. [On line]. | Link | Weber M, Völlner F, Benditz A, Schwarz T, Wörner M, Craiovan B, et al. Kniegelenkersatz des älteren Menschen [Total knee arthroplasty in the elderly]. Orthopade. 2017 Jan;46(1):34-39. | CrossRef | PubMed |
Weber M, Völlner F, Benditz A, Schwarz T, Wörner M, Craiovan B, et al. Kniegelenkersatz des älteren Menschen [Total knee arthroplasty in the elderly]. Orthopade. 2017 Jan;46(1):34-39. | CrossRef | PubMed | Cnudde P, Rolfson O, Timperley AJ, Garland A, Kärrholm J, Garellick G, et al. Do Patients Live Longer After THA and Is the Relative Survival Diagnosis-specific? Clin Orthop Relat Res. 2018 Jun;476(6):1166-1175. | CrossRef | PubMed |
Cnudde P, Rolfson O, Timperley AJ, Garland A, Kärrholm J, Garellick G, et al. Do Patients Live Longer After THA and Is the Relative Survival Diagnosis-specific? Clin Orthop Relat Res. 2018 Jun;476(6):1166-1175. | CrossRef | PubMed | Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: Annual Report 2017. Adelaide: AOA; 2017. [On line]. | Link |
Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: Annual Report 2017. Adelaide: AOA; 2017. [On line]. | Link | Karrholm J, Rogmark C, Nauclér E, Vinblad J, Mohaddes M, Rolfson O. Swedish Hip Arthroplasty Register: Annual Report 2018. 2018. [On line]. | Link |
Karrholm J, Rogmark C, Nauclér E, Vinblad J, Mohaddes M, Rolfson O. Swedish Hip Arthroplasty Register: Annual Report 2018. 2018. [On line]. | Link | Aw D, Sahota O. Orthogeriatrics moving forward. Age Ageing. 2014 May;43(3):301-5. | CrossRef | PubMed |
Aw D, Sahota O. Orthogeriatrics moving forward. Age Ageing. 2014 May;43(3):301-5. | CrossRef | PubMed | Berend ME, Thong AE, Faris GW, Newbern G, Pierson JL, Ritter MA. Total joint arthroplasty in the extremely elderly: hip and knee arthroplasty after entering the 89th year of life. J Arthroplasty. 2003 Oct;18(7):817-21. | CrossRef | PubMed |
Berend ME, Thong AE, Faris GW, Newbern G, Pierson JL, Ritter MA. Total joint arthroplasty in the extremely elderly: hip and knee arthroplasty after entering the 89th year of life. J Arthroplasty. 2003 Oct;18(7):817-21. | CrossRef | PubMed | Fabre-Aubrespy M, Ollivier M, Pesenti S, Parratte S, Argenson JN. Unicompartmental Knee Arthroplasty in Patients Older Than 75 Results in Better Clinical Outcomes and Similar Survivorship Compared to Total Knee Arthroplasty. A Matched Controlled Study. J Arthroplasty. 2016 Dec;31(12):2668-2671. | CrossRef | PubMed |
Fabre-Aubrespy M, Ollivier M, Pesenti S, Parratte S, Argenson JN. Unicompartmental Knee Arthroplasty in Patients Older Than 75 Results in Better Clinical Outcomes and Similar Survivorship Compared to Total Knee Arthroplasty. A Matched Controlled Study. J Arthroplasty. 2016 Dec;31(12):2668-2671. | CrossRef | PubMed | Siman H, Kamath AF, Carrillo N, Harmsen WS, Pagnano MW, Sierra RJ. Unicompartmental Knee Arthroplasty vs Total Knee Arthroplasty for Medial Compartment Arthritis in Patients Older Than 75 Years: Comparable Reoperation, Revision, and Complication Rates. J Arthroplasty. 2017 Jun;32(6):1792-1797. | CrossRef | PubMed |
Siman H, Kamath AF, Carrillo N, Harmsen WS, Pagnano MW, Sierra RJ. Unicompartmental Knee Arthroplasty vs Total Knee Arthroplasty for Medial Compartment Arthritis in Patients Older Than 75 Years: Comparable Reoperation, Revision, and Complication Rates. J Arthroplasty. 2017 Jun;32(6):1792-1797. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








