Key Words: urinary incontinence, prevalence, primary health care, women
Abstract
Purpose
This research seeks to determine the prevalence of urinary incontinence in adult women in La Serena, Chile, exploring its association with known risk factors.
Methods
We conducted a cross-sectional, descriptive study with an analytical component. A validated questionnaire was applied to 371 women who consented, were aged 30 or older, and were users of primary health care centers.
Results
The prevalence obtained was 45.01%, associated with four main factors: hard work (odds ratio: 2.29; 95% confidence interval: 1.45 to 3.62), constipation (odds ratio: 1.99; 95% confidence interval: 1.21 to 2.76), type 2 diabetes (odds ratio: 1.88; 95% confidence interval: 1.16 to 3.06) and obesity (odds ratio: 1.09; 95% confidence interval: 1.05 to 1.14).
Conclusions
Given the high prevalence of urinary incontinence, its association with prevalent health problems, and its known impact on women's quality of life, the authors suggest that strategies be implemented to deal with this health problem at the primary care level.
Main messages
|
Introduction
Urinary incontinence is defined as "the involuntary loss of urine that conditions a hygienic and/or social problem, and that can be objectively demonstrated"[1]. Urinary incontinence is two to four times more frequent in women than in men and increases progressively with age[1],[2],[3]. A study conducted in Norway found a prevalence of 25% for urinary incontinence in women over 20 years old[2]. Another European study conducted in four countries reported that 35% of women over 18 presented symptoms of urinary incontinence[1]; the prevalence rates were 44% in France, 41% in Germany, 42% in the United Kingdom and 23% in Spain, with Stress urinary incontinece being the most common type. In Chile, Salazar et al. determined a urinary incontinence prevalence of 62.2% in women from the Chilean Air Force Hospital[4]. Harwardt et al. found a 77% prevalence in Easter Island women[5]. The prevalence study conducted by Rincón, in users of primary care facilities in the city of Chillán, showed a urinary incontinence prevalence of 62.6%[6].
The relevance of urinary incontinence lies in the negative impact that it generates in the quality of life of those who suffer it, at a psychological level, limiting autonomy and reducing self-esteem. For instance, women who have urinary incontinence avoid social interaction, leading to social isolation[6],[7],[8]. A cross-sectional study carried out in Spain concluded that the impact on the quality of life affects primarily two aspects: the limitation of physical activity and the negative impact on body image due to body odor or the use of pads, among other consequences. The aspects of daily life that are most affected by urinary incontinence are sleep, mobility, emotional behavior, social interaction, and leisure activities[6],[7],[8]. Additionally, the quality of life in people with urinary incontinence worsens with age due to increased severity of incontinence and increased urinary symptomatology if episodes of urinary tract infection are also associated[8]. The severity of urinary incontinence was categorized by Sandvik, who proposed a scale that relates the frequency and amount of urine loss per episode. The scale was validated by Hanley[3].
Published evidence shows that the most relevant risk factors associated with the development or presence of urinary incontinence are age, gender, increased body mass index, and diabetes[5],[6],[9]. The obstetric history (number of births, type of birth, and weight of the child), urogynaecological history, and onset of menopause are also relevant risk factors[5],[10]. Moreover, an association between urinary incontinence and constipation has been described[11],[12]. Additional risk factors include diseases of the central nervous system (such as dementia, Parkinson's disease, stroke, multiple sclerosis), musculoskeletal diseases that result in decreased mobility and also some occupational factors[13],[14]. The relationship between type of work and urinary incontinence has been seldom explored[15],[16]. A study in South Korea found a significant association between urinary incontinence and some work environments: feeling pressured by time, uncomfortable and non-ergonomic working position for long periods, and carrying heavy loads[15]. Thus, the relationship between labor and urinary incontinence is related to the work environment and the urinary habits that women develop in this context[15],[17],[18]. For the purposes of this study, and according to Chilean legislation for female workers, hard work was defined as "work that requires many hours of standing, moving heavy objects (greater than 20 kilograms), going up and down stairs, or more than eight hours of work daily"[19].
Epidemiological studies concerning urinary incontinence have been conducted mostly in Europe and the United States, the literature being scarce in Latin America and Chile. As it is a health complication that impacts on the quality of life of those who suffer from it [6],[7],[8],[9],[10], this research aims to determine the prevalence of urinary incontinence in adult women in the commune of the city of La Serena and to assess the relationship between urinary incontinence and known risk factors.
Methods
A cross-sectional, descriptive study with an analytical component was conducted to determine the prevalence of female urinary incontinence and to explore associated factors in La Serena, a coastal city located in the mid-north zone of Chile, from October 2018 until January 2019. The participants were women over 30 years of age who used the primary health care network of the city. Exclusion criteria were defined in order to avoid confusion bias. Exclusion criteria included: being pregnant, women who gave birth in the past 6 months, and women consulting for lower urinary tract symptoms. The questionnaire used was validated in the Rincón study[9], which defines urinary incontinence as involuntary urine loss in the last month and uses the Sandvik index to determine severity[3]. The questionnaire is presented as supplementary material. Sample size was calculated by assuming a prevalence of 40%. For a total of 55 574 women over 30 using the public health system, considering 95% confidence and 5% error, a minimum of 366 surveys was calculated to be needed. The sample was taken randomly by cluster, with a proportional distribution according to each health center. Surveys were conducted, in a private environment, by well-trained fourth-year medical students after obtaining informed consent from the participants, who had consulted spontaneously by various health problems in the six urban centers that are part of the city's primary health care network. The questionnaire's time of completion varied from ten to 15 minutes. Data were recorded by each surveyor through the Survey Monkey® application on a mobile device, under the supervision of the principal researcher. Analysis to determine possible relationships was performed by calculating odds ratios with the respective chi-squared test. Subsequently, variables with a strong univariate relationship were later assessed through multivariate logistic regression analysis, adjusting by age. Pearson's chi-squared test was used to evaluate the goodness of fit of the model. The level of confidence for all tests was 95%. Data analysis and tabulation was performed in Microsoft Excel® and IBM-SPSS V26®.
The research was approved in September 2018 by Resolution N° 86 of the Scientific Ethical Committee of the Universidad Católica del Norte, Coquimbo. All participants accepted and signed the informed consent form and the ethical principles where preserved at all times. Data were analyzed blindly, utilizing a code for each participant.
Results
A total of 371 women between 30 and 88 years old were surveyed. Fortunately, registers presented no missing data. The average age of the participants was 55.87 years. Table 1 gives details on nutritional status, type of work and gynaeco-obstetric characteristics. The range of deliveries was zero to ten children. The majority of women interviewed had at least one normal delivery and 62% of the women were post-menopausal.
Table 1.Characteristics of women surveyed.
The overall prevalence of urinary incontinence reached 45.01% (n = 167). According to the Sandvik scale, mild and moderate urinary incontinence represented 43% and 41%, respectively. 13.2% of women presented severe urinary incontinence (n = 22) and 2.4% presented highly severe incontinence (n = 4). Of the women who had urinary incontinence, only 18% (n = 31) reported having consulted a health professional. From those who consulted (76.7%), 7.8% visited a gynecologist, 6% went to a general practitioner, 4.8% to a midwife, and the remaining 4.8% to another health professional.
The results for the possible factors associated with urinary incontinence are presented in Table 2. There was no significant association with age. Regarding nutritional status, obese women were more likely to have urinary incontinence than those who were not obese (odds ratio: 1.43; confidence interval: 1.29 to 3.11). Also, women with diabetes had a higher risk of having urinary incontinence (odds ratio: 1.37; confidence interval: 1.15 to 3.06) than non-diabetics. Women exposed to hard work had a 1.15-fold chance of presenting with UI (odds ratio: 1.15; confidence interval: 1.45 to 3.62). For gynaecological history and type of birth, no significant differences were observed between women with and without urinary incontinence. Likewise, the number of deliveries and birthweight of newborn children were not significantly associated with urinary incontinence in the studied group. However, for women with a history of constipation, the presence of urinary incontinence was 1.32-fold more frequent than in those with normal bowel habits (odds ratio: 1.32; confidence interval: 1.09 to 2.75). Constipation was assessed through the question: Do you evacuate less than three times a week or do you have to exert yourself to evacuate?
Table 2. Raw Odds Ratio of the studied associated factors.
Finally, Table 3 shows the results of logistic regression analysis, adjusted by age. The variables significantly associated with the presence of UI, according to the model, were hard work, constipation, type 2 diabetes mellitus and obesity.
Table 3. Variables associated to urinary incontinence, adjusted by age.
Discussion
In this investigation, the prevalence of urinary incontinence was determined to be 45%. Other national investigations have found a higher prevalence: Harwart obtained 77% prevalence on Easter Island[8], Salazar found a prevalence of 62.2% in a hospital population of Santiago[4] and Rincón obtained 77% prevalence in women from Chillán[9]. European research determined prevalence between 25% and 45%[4], which are in accord with our results. Prevalence tended to increase with the age of the women studied. However, this relation was not statistically significant, in contrast to other published experiences[2],[6],[20],[21].
The present study found significant associations of urinary incontinence with four known risk factors: hard work, obesity, diabetes, and constipation. Indeed, exposure to hard work presented a strong relationship with the existence of urinary incontinence, which corresponds with other studies[18],[22]. This relationship could be explained by the physical effort made in this type of work, which tends to increase intra-abdominal and bladder pressure, facilitating incontinence. Other working conditions were not explored, so it was not possible to relate this factor with the urinary habit associated, for example, with the scarce availability of hygienic services, as evidenced by other studies[14],[15],[16],[17].
Other factors related to urinary incontinence were obesity and the presence of type 2 diabetes, as has been described by international evidence[6],[10]. Published research estimates that the risk of urinary incontinence in diabetic women is double compared to non-diabetic women[5],[9]. According to the last National Health Survey from 2016 to 2017, 33.7% of the female population will suffer from obesity, and 14% will present type 2 diabetes[23]. As a result, a high proportion of the adult female Chilean population will be at increased risk for urinary incontinence.
On the other hand, constipation was found to be strongly associated with urinary incontinence; this coincides with other studies indicating that urinary incontinence is more severe in patients with constipation and that this would be a significant predictor of exertion in urinary incontinence[12],[17]. Rodriguez also determined that there is an association between urinary incontinence and constipation and that neurological lesions of the pelvic area and striated anal sphincter occur with excessive pushing[24]. A recent meta-analysis showed that women with constipation have a 2.4-fold higher risk of urinary incontinence[11].
In international evidence, the number of deliveries and types of labor are well-known risk factors[4],[5],[6]. In this research, no statistically significant relationship was found for gynecological or obstetric antecedents, although the history of instrumental delivery (forceps) presented a slight association with the presence of urinary incontinence. It could be speculated that, as the fertility rate is currently diminishing in Chile[25]—only 1.68 children per woman—then, proportionally, the number of deliveries loses strength as a risk factor for urinary incontinence. At the same time, the high rate of cesarean sections—37% in the year 2018[26]—could reduce the influence of the type of birth and weight of the newborn child in the development of urinary incontinence.
It is noteworthy that a high proportion of women presenting urinary incontinence did not consult for this condition (76%). A qualitative Chilean study conducted in Concepción concluded that women learn to live with urinary incontinence, while also highlighting that the health system has access gaps to address regarding urinary incontinence[27]. The first finding agrees with a study carried out in Madrid[13]. Thus, urinary incontinence appeared to be an underestimated health problem affecting people's quality of life[13],[24].
A limitation of the study is that it was carried out in only one city. At the same time, the study was conducted only in the public sector healthcare centers, which could result in selection bias. Women with private insurance have a better social and economic situation that protects them from health risks while having a lower prevalence of chronic pathologies and better living and working conditions.
Nevertheless, the study also presents strengths. First, the sample was representative of Chilean adult women. La Serena is a city with more than 200 000 inhabitants, in which roughly 88% of the women are registered in primary care centers[28]. Consequently, both the universe and the sample make up a studied population even more comparable with populations at the national level or with other countries. Second, the questionnaire used was previously validated, and its results are consistent with other national and international studies. The above makes it possible to generalize the results to the rest of the country and even internationally by being consistent with international studies. Therefore, it would be possible to affirm that urinary incontinence is, in general, a highly prevalent health problem among adult women.
In Chile, urinary incontinence is currently not framed in a specific health program, so the treatment depends on the patients visualizing urinary incontinence as a relevant health problem and on their spending capacity[13],[22],[24],[29]. It is worth mentioning that neuromuscular intervention in the pelvic area improves the outcome in more than a third of cases, according to a meta-analysis carried out recently[30]. On the other hand, between 20% and 50% of urinary incontinence cases, depending on severity, would require surgical treatment, along with the cost that this entails[31].
A more extensive or multi-center prevalence study would be warranted to guide the design of a national program harmonizing preventive interventions, diagnostics, and multidisciplinary management of urinary incontinence. As a proposal for intervention, primary care centers should be considered the leading providers of education in urinary habits and treatment for mild and moderate stages of the condition. They can also intervene and treat other high-prevalence pathologies, such as obesity and diabetes, which are known risk factors for urinary incontinence. Other kinds of treatment (laser or surgery) could be addressed at secondary or tertiary levels. It has also been suggested that awareness should be created in women regarding urinary habits, together with urging their employers to maintain proper hygienic services in the workplace, as well as ensuring access to urinate when necessary.
Conclusions
This research provides evidence that urinary incontinence is a relevant condition among the Chilean female population, associated with working conditions, constipation, and health problems of high prevalence in the general female population, such as obesity and type 2 diabetes. The epidemiological evidence and the consequences of this condition on the affected women point to a need to tackle the condition, starting with primary health care strategies of intervention.
Notes
Authorship and contribution roles
ASM: protocol, project development, data collection, data analysis, writing the original manuscript. MRS: project development, data analysis, translation and editing.
Acknowledgments
The authors thank physiotherapists Montserrat Fariña and Susana González for their support in accomplishing the requirements of the Ethics Committee regarding giving an educational session to the women who were diagnosed with urinary infection during the study. Also, the authors thank the medical students who participated as surveyors and the health authorities who authorized the surveyors' access to the health facilities.
Funding
The Master's program in Public Health of the Faculty of Medicine, Universidad Católica del Norte, partially funded this research. This article is the result of a thesis to obtain the degree of Master in Public Health.
Competing interests
The authors declare no conflicts of interests.
Ethical aspects
The research was approved in September 2018 by Resolution N° 86 of the Scientific Ethical Committee of the Universidad Católica del Norte, Coquimbo. The data of the study are available upon request to the correspondence author.

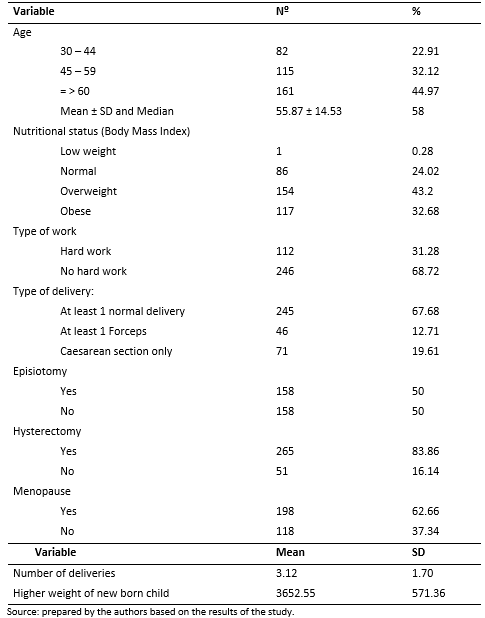 Table 1.Characteristics of women surveyed.
Table 1.Characteristics of women surveyed.

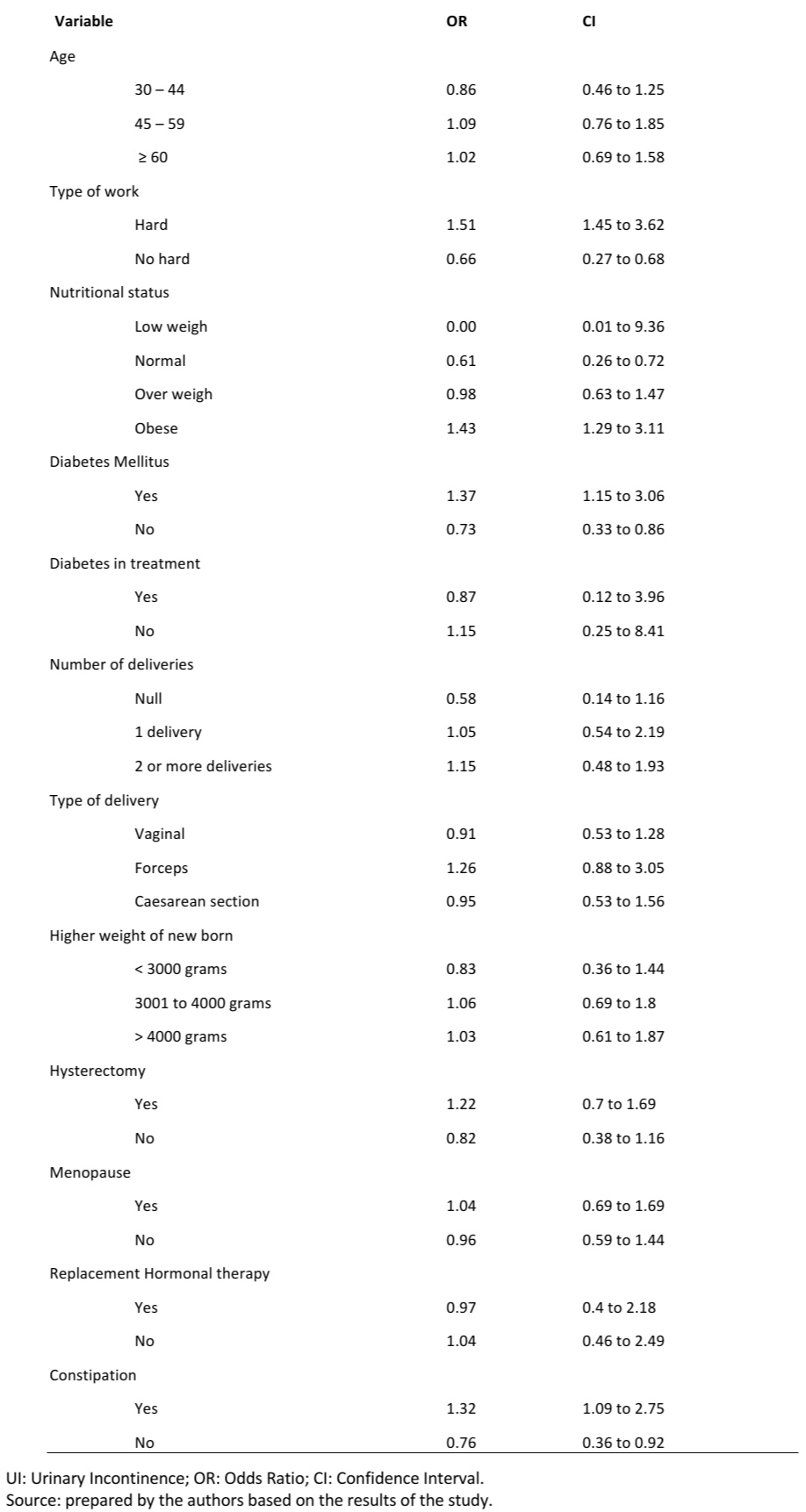 Table 2. Raw Odds Ratio of the studied associated factors.
Table 2. Raw Odds Ratio of the studied associated factors.

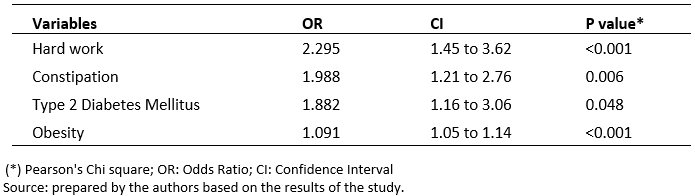 Table 3. Variables associated to urinary incontinence, adjusted by age.
Table 3. Variables associated to urinary incontinence, adjusted by age.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Objetivo
Determinar la prevalencia de incontinencia urinaria en mujeres adultas de la ciudad de La Serena, explorando la asociación con factores de riesgo conocidos.
Métodos
Estudio descriptivo transversal, con componente analítico. Se aplicó un cuestionario validado a 371 mujeres mayores de 30 años y usuarias de centros de atención primaria, que dieron su consentimiento.
Resultados
Se obtuvo una prevalencia de 45,01%, asociándose con trabajo pesado (Odds ratio: 2,29; intervalo de confianza 95%: 1,45 a 3,62); estreñimiento (Odds ratio: 1,99; intervalo de confianza 95%: 1,21 a 2,76); diabetes mellitus tipo 2 (Odds ratio: 1,88; intervalo de confianza 95%: 1,16 a 3,06) y obesidad (Odds ratio: 1,09; intervalo de confianza 95%: 1,05 a 1,14).
Conclusiones
Dada la alta prevalencia de incontinencia urinaria, su asociación con problemas de salud prevalentes y el impacto conocido en la calidad de vida de las mujeres, los autores sugieren la implementación de estrategias que aborden este problema en el nivel de atención primaria.
 Authors:
Andrés Salgado-Maldonado[1,2], Muriel Ramírez-Santana[2]
Authors:
Andrés Salgado-Maldonado[1,2], Muriel Ramírez-Santana[2]
Affiliation:
[1] Centro de Salud Familiar Doctor Sergio Aguilar, Coquimbo, Chile
[2] Departamento de Salud Pública, Facultad de Medicina, Universidad Católica del Norte, Coquimbo, Chile
E-mail: mramirezs@ucn.cl
Author address:
[1] Calle Larrondo 1281, Coquimbo, Chile

Citation: Salgado-Maldonado A, Ramírez-Santana M. Urinary incontinence in Chilean women: A prevalence study of the health profile and associated factors. Medwave 2020;20(6):e7976 doi: 10.5867/medwave.2020.06.7976
Submission date: 3/3/2020
Acceptance date: 4/6/2020
Publication date: 27/7/2020
Origin: Not commissioned
Type of review: Externally peer-reviewed by three reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol. 2002 Jul;187(1):116-26. | CrossRef | PubMed |
- Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trøndelag. J Clin Epidemiol. 2000 Nov;53(11):1150-7. | CrossRef | PubMed |
- Sandvik H, Seim A, Vanvik A, Hunskaar S. A severity index for epidemiological surveys of female urinary incontinence: comparison with 48-hour pad-weighing tests. Neurourol Urodyn. 2000;19(2):137-45. | CrossRef | PubMed |
- Salazar A, Oyanedel P, Montiglio C, Campero JM, Caro C, Monje B, et al. Prevalencia y factores de riesgo de la incontinencia de orina. Rev Chil Urol 2005; 70: 55–59. [On line] | Link |
- Harwardt T, Fuentes B, Venegas M, Leal C, Verdugo F, Benier P. Estudio de prevalencia de incontinencia urinaria en mujeres de Isla de Pascua. Rev Chil Urol 2004; 69: 29–34.[On line] | Link |
- Rincón Ardila O. Caracterización clínica de la incontinencia urinaria y factores asociados en usuarias de la Unidad de la Mujer del Centro de Salud Familiar Ultraestación en la ciudad de Chillán, Chile [Prevalence and risk factors for urinary incontinence among women consulting in primary care]. Rev Med Chil. 2015 Feb;143(2):203-12. Spanish. | CrossRef | PubMed |
- Suárez Serrano CM, Medrano Sánchez E, Díaz Mohedo E, de la Casa Almeida M, Chillón Martínez R, Chamorro Moriana G. Afectación de la calidad de vida en mujeres con incontinencia urinaria. Fisioterapia. 2013 Jan 1;35(1):18–23. [On line] | Link |
- Córcoles MB, Sánchez SA, Bachs GJ, Moreno DM, Navarro PH, Rodríguez VJ. Calidad de vida en las pacientes con incontinencia urinaria [Quality of life in patients with urinary incontinence]. Actas Urol Esp. 2008 Feb;32(2):202-10. Spanish. | CrossRef | PubMed |
- Phelan S, Grodstein F, Brown JS. Clinical research in diabetes and urinary incontinence: what we know and need to know. J Urol. 2009 Dec;182(6 Suppl):S14-7. | CrossRef | PubMed |
- Dhillon HK, MZain AZ, Quek KF, Singh HJ, Kaur G, Nordin RB. Prevalence and risk ractors of urinary incontinence and its impact on the quality of life and treatment seeking behavior among Malaysian women : A review. Women's Heal Care 2016; 5: 1–9. [On line] | Link |
- Lian WQ, Li FJ, Huang HX, Zheng YQ, Chen LH. Constipation and risk of urinary incontinence in women: a meta-analysis. Int Urogynecol J. 2019 Oct;30(10):1629-1634. | CrossRef | PubMed |
- Maeda T, Tomita M, Nakazawa A, Sakai G, Funakoshi S, Komatsuda A, et al. Female Functional Constipation Is Associated with Overactive Bladder Symptoms and Urinary Incontinence. Biomed Res Int. 2017;2017:2138073. | CrossRef | PubMed |
- Martinez Saura F, Fouz López C, Gil Díaz P, Téllez Martínez-Fornés M. Incontinencia urinaria : una visión desde Atención Primaria. MEDIFAM 2001; 11: 25–40.[On line] | Link |
- Reynolds WS, Kowalik C, Delpe SD, Kaufman M, Fowke JH, Dmochowski R. Toileting Behaviors and Bladder Symptoms in Women Who Limit Restroom Use at Work: A Cross-Sectional Study. J Urol. 2019 Nov;202(5):1008-1014. | CrossRef | PubMed |
- Kim Y, Kwak Y. Urinary incontinence in women in relation to occupational status. Women Health. 2017 Jan;57(1):1-18. | CrossRef | PubMed |
- Markland A, Chu H, Epperson CN, Nodora J, Shoham D, Smith A, et al.Occupation and lower urinary tract symptoms in women: A rapid review and meta-analysis from the PLUS research consortium. Neurourol Urodyn. 2018 Nov;37(8):2881-2892. | CrossRef | PubMed |
- Liao YM, Dougherty MC, Biemer PP, Liao CT, Palmer MH, Boyington AR, et al. Factors related to lower urinary tract symptoms among a sample of employed women in Taipei. Neurourol Urodyn. 2008;27(1):52-9. | CrossRef | PubMed |
- Pierce HM, Perry L, Gallagher R, Chiarelli P. Delaying voiding, limiting fluids, urinary symptoms, and work productivity: A survey of female nurses and midwives. J Adv Nurs. 2019 Nov;75(11):2579-2590. | CrossRef | PubMed |
- Gobierno de Chile, Ministerio del Trabajo y Previsión Social. Ley 20001. Biblioteca del Congreso Nacional de Chile. 2005. | Link |
- Islam RM, Oldroyd J, Rana J, Romero L, Karim MN. Prevalence of symptomatic pelvic floor disorders in community-dwelling women in low and middle-income countries: a systematic review and meta-analysis. Int Urogynecol J. 2019 Dec;30(12):2001-2011. | CrossRef | PubMed |
- Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003 May;20(6):327-36. | CrossRef | PubMed |
- Titman SC, Radley SC, Gray TG. Self-management in women with stress incontinence: strategies, outcomes and integration into clinical care. Res Rep Urol. 2019 Apr 17;11:111-121. | CrossRef | PubMed |
- Ministerio de Salud de Chile. Encuesta Nacional de Salud 2016-2017 Primeros resultados. 2017. [On line] | Link |
- Rodríguez Adams, EL. Non obstetric risk factors and quality of life in middle-aged women suffering from urinary incontinence. Rev Cuba Ginecol y Obstet 2014; 40: 119–135.[On line] | Link |
- Instituto Nacional de Estadísticas. Publicación Estadísticas Vitales, 2017. 2019. [On line] | Link |
- Ministerio de Salud de Chile. Departamento de Estadisticas e Informacion de Salud. Registro estadístico mensual. Atencion de maternidad.2018. [On line] | Link |
- Bascur-Castillo C, Araneda-Gatica V, Castro-Arias H, Carrasco-Portiño M, Ruiz-Cantero MT. Determinants in the process of seeking help for urinary incontinence in the Chilean health system. Int J Gynaecol Obstet. 2019 Jan;144(1):103-111. | CrossRef | PubMed |
- FONASA. Boletin estadistico agosto. Boletin estadistico 2017-2018. | Link |
- Cerruto MA, Asimakopoulos AD, Artibani W, Del Popolo G, La Martina M, Carone R, et al. Insight into new potential targets for the treatment of overactive bladder and detrusor overactivity. Urol Int. 2012;89(1):1-8. | CrossRef | PubMed |
- Robinson D, Giarenis I, Cardozo L. The medical management of refractory overactive bladder. Maturitas. 2013 Apr;74(4):386-90. | CrossRef | PubMed |
- Rubilotta E, Balzarro M, D'Amico A, Cerruto MA, Bassi S, Bovo C, et al. Pure stress urinary incontinence: analysis of prevalence, estimation of costs, and financial impact. BMC Urol. 2019 Jun 4;19(1):44. | CrossRef | PubMed |
 Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol. 2002 Jul;187(1):116-26. | CrossRef | PubMed |
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol. 2002 Jul;187(1):116-26. | CrossRef | PubMed | Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trøndelag. J Clin Epidemiol. 2000 Nov;53(11):1150-7. | CrossRef | PubMed |
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trøndelag. J Clin Epidemiol. 2000 Nov;53(11):1150-7. | CrossRef | PubMed | Sandvik H, Seim A, Vanvik A, Hunskaar S. A severity index for epidemiological surveys of female urinary incontinence: comparison with 48-hour pad-weighing tests. Neurourol Urodyn. 2000;19(2):137-45. | CrossRef | PubMed |
Sandvik H, Seim A, Vanvik A, Hunskaar S. A severity index for epidemiological surveys of female urinary incontinence: comparison with 48-hour pad-weighing tests. Neurourol Urodyn. 2000;19(2):137-45. | CrossRef | PubMed | Salazar A, Oyanedel P, Montiglio C, Campero JM, Caro C, Monje B, et al. Prevalencia y factores de riesgo de la incontinencia de orina. Rev Chil Urol 2005; 70: 55–59. [On line] | Link |
Salazar A, Oyanedel P, Montiglio C, Campero JM, Caro C, Monje B, et al. Prevalencia y factores de riesgo de la incontinencia de orina. Rev Chil Urol 2005; 70: 55–59. [On line] | Link | Harwardt T, Fuentes B, Venegas M, Leal C, Verdugo F, Benier P. Estudio de prevalencia de incontinencia urinaria en mujeres de Isla de Pascua. Rev Chil Urol 2004; 69: 29–34.[On line] | Link |
Harwardt T, Fuentes B, Venegas M, Leal C, Verdugo F, Benier P. Estudio de prevalencia de incontinencia urinaria en mujeres de Isla de Pascua. Rev Chil Urol 2004; 69: 29–34.[On line] | Link | Rincón Ardila O. Caracterización clínica de la incontinencia urinaria y factores asociados en usuarias de la Unidad de la Mujer del Centro de Salud Familiar Ultraestación en la ciudad de Chillán, Chile [Prevalence and risk factors for urinary incontinence among women consulting in primary care]. Rev Med Chil. 2015 Feb;143(2):203-12. Spanish. | CrossRef | PubMed |
Rincón Ardila O. Caracterización clínica de la incontinencia urinaria y factores asociados en usuarias de la Unidad de la Mujer del Centro de Salud Familiar Ultraestación en la ciudad de Chillán, Chile [Prevalence and risk factors for urinary incontinence among women consulting in primary care]. Rev Med Chil. 2015 Feb;143(2):203-12. Spanish. | CrossRef | PubMed | Suárez Serrano CM, Medrano Sánchez E, Díaz Mohedo E, de la Casa Almeida M, Chillón Martínez R, Chamorro Moriana G. Afectación de la calidad de vida en mujeres con incontinencia urinaria. Fisioterapia. 2013 Jan 1;35(1):18–23. [On line] | Link |
Suárez Serrano CM, Medrano Sánchez E, Díaz Mohedo E, de la Casa Almeida M, Chillón Martínez R, Chamorro Moriana G. Afectación de la calidad de vida en mujeres con incontinencia urinaria. Fisioterapia. 2013 Jan 1;35(1):18–23. [On line] | Link | Córcoles MB, Sánchez SA, Bachs GJ, Moreno DM, Navarro PH, Rodríguez VJ. Calidad de vida en las pacientes con incontinencia urinaria [Quality of life in patients with urinary incontinence]. Actas Urol Esp. 2008 Feb;32(2):202-10. Spanish. | CrossRef | PubMed |
Córcoles MB, Sánchez SA, Bachs GJ, Moreno DM, Navarro PH, Rodríguez VJ. Calidad de vida en las pacientes con incontinencia urinaria [Quality of life in patients with urinary incontinence]. Actas Urol Esp. 2008 Feb;32(2):202-10. Spanish. | CrossRef | PubMed | Phelan S, Grodstein F, Brown JS. Clinical research in diabetes and urinary incontinence: what we know and need to know. J Urol. 2009 Dec;182(6 Suppl):S14-7. | CrossRef | PubMed |
Phelan S, Grodstein F, Brown JS. Clinical research in diabetes and urinary incontinence: what we know and need to know. J Urol. 2009 Dec;182(6 Suppl):S14-7. | CrossRef | PubMed | Dhillon HK, MZain AZ, Quek KF, Singh HJ, Kaur G, Nordin RB. Prevalence and risk ractors of urinary incontinence and its impact on the quality of life and treatment seeking behavior among Malaysian women : A review. Women's Heal Care 2016; 5: 1–9. [On line] | Link |
Dhillon HK, MZain AZ, Quek KF, Singh HJ, Kaur G, Nordin RB. Prevalence and risk ractors of urinary incontinence and its impact on the quality of life and treatment seeking behavior among Malaysian women : A review. Women's Heal Care 2016; 5: 1–9. [On line] | Link | Lian WQ, Li FJ, Huang HX, Zheng YQ, Chen LH. Constipation and risk of urinary incontinence in women: a meta-analysis. Int Urogynecol J. 2019 Oct;30(10):1629-1634. | CrossRef | PubMed |
Lian WQ, Li FJ, Huang HX, Zheng YQ, Chen LH. Constipation and risk of urinary incontinence in women: a meta-analysis. Int Urogynecol J. 2019 Oct;30(10):1629-1634. | CrossRef | PubMed | Maeda T, Tomita M, Nakazawa A, Sakai G, Funakoshi S, Komatsuda A, et al. Female Functional Constipation Is Associated with Overactive Bladder Symptoms and Urinary Incontinence. Biomed Res Int. 2017;2017:2138073. | CrossRef | PubMed |
Maeda T, Tomita M, Nakazawa A, Sakai G, Funakoshi S, Komatsuda A, et al. Female Functional Constipation Is Associated with Overactive Bladder Symptoms and Urinary Incontinence. Biomed Res Int. 2017;2017:2138073. | CrossRef | PubMed | Martinez Saura F, Fouz López C, Gil Díaz P, Téllez Martínez-Fornés M. Incontinencia urinaria : una visión desde Atención Primaria. MEDIFAM 2001; 11: 25–40.[On line] | Link |
Martinez Saura F, Fouz López C, Gil Díaz P, Téllez Martínez-Fornés M. Incontinencia urinaria : una visión desde Atención Primaria. MEDIFAM 2001; 11: 25–40.[On line] | Link | Reynolds WS, Kowalik C, Delpe SD, Kaufman M, Fowke JH, Dmochowski R. Toileting Behaviors and Bladder Symptoms in Women Who Limit Restroom Use at Work: A Cross-Sectional Study. J Urol. 2019 Nov;202(5):1008-1014. | CrossRef | PubMed |
Reynolds WS, Kowalik C, Delpe SD, Kaufman M, Fowke JH, Dmochowski R. Toileting Behaviors and Bladder Symptoms in Women Who Limit Restroom Use at Work: A Cross-Sectional Study. J Urol. 2019 Nov;202(5):1008-1014. | CrossRef | PubMed | Kim Y, Kwak Y. Urinary incontinence in women in relation to occupational status. Women Health. 2017 Jan;57(1):1-18. | CrossRef | PubMed |
Kim Y, Kwak Y. Urinary incontinence in women in relation to occupational status. Women Health. 2017 Jan;57(1):1-18. | CrossRef | PubMed | Markland A, Chu H, Epperson CN, Nodora J, Shoham D, Smith A, et al.Occupation and lower urinary tract symptoms in women: A rapid review and meta-analysis from the PLUS research consortium. Neurourol Urodyn. 2018 Nov;37(8):2881-2892. | CrossRef | PubMed |
Markland A, Chu H, Epperson CN, Nodora J, Shoham D, Smith A, et al.Occupation and lower urinary tract symptoms in women: A rapid review and meta-analysis from the PLUS research consortium. Neurourol Urodyn. 2018 Nov;37(8):2881-2892. | CrossRef | PubMed | Liao YM, Dougherty MC, Biemer PP, Liao CT, Palmer MH, Boyington AR, et al. Factors related to lower urinary tract symptoms among a sample of employed women in Taipei. Neurourol Urodyn. 2008;27(1):52-9. | CrossRef | PubMed |
Liao YM, Dougherty MC, Biemer PP, Liao CT, Palmer MH, Boyington AR, et al. Factors related to lower urinary tract symptoms among a sample of employed women in Taipei. Neurourol Urodyn. 2008;27(1):52-9. | CrossRef | PubMed | Pierce HM, Perry L, Gallagher R, Chiarelli P. Delaying voiding, limiting fluids, urinary symptoms, and work productivity: A survey of female nurses and midwives. J Adv Nurs. 2019 Nov;75(11):2579-2590. | CrossRef | PubMed |
Pierce HM, Perry L, Gallagher R, Chiarelli P. Delaying voiding, limiting fluids, urinary symptoms, and work productivity: A survey of female nurses and midwives. J Adv Nurs. 2019 Nov;75(11):2579-2590. | CrossRef | PubMed | Gobierno de Chile, Ministerio del Trabajo y Previsión Social. Ley 20001. Biblioteca del Congreso Nacional de Chile. 2005. | Link |
Gobierno de Chile, Ministerio del Trabajo y Previsión Social. Ley 20001. Biblioteca del Congreso Nacional de Chile. 2005. | Link | Islam RM, Oldroyd J, Rana J, Romero L, Karim MN. Prevalence of symptomatic pelvic floor disorders in community-dwelling women in low and middle-income countries: a systematic review and meta-analysis. Int Urogynecol J. 2019 Dec;30(12):2001-2011. | CrossRef | PubMed |
Islam RM, Oldroyd J, Rana J, Romero L, Karim MN. Prevalence of symptomatic pelvic floor disorders in community-dwelling women in low and middle-income countries: a systematic review and meta-analysis. Int Urogynecol J. 2019 Dec;30(12):2001-2011. | CrossRef | PubMed | Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003 May;20(6):327-36. | CrossRef | PubMed |
Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003 May;20(6):327-36. | CrossRef | PubMed | Titman SC, Radley SC, Gray TG. Self-management in women with stress incontinence: strategies, outcomes and integration into clinical care. Res Rep Urol. 2019 Apr 17;11:111-121. | CrossRef | PubMed |
Titman SC, Radley SC, Gray TG. Self-management in women with stress incontinence: strategies, outcomes and integration into clinical care. Res Rep Urol. 2019 Apr 17;11:111-121. | CrossRef | PubMed | Ministerio de Salud de Chile. Encuesta Nacional de Salud 2016-2017 Primeros resultados. 2017. [On line]
| Link |
Ministerio de Salud de Chile. Encuesta Nacional de Salud 2016-2017 Primeros resultados. 2017. [On line]
| Link | Rodríguez Adams, EL. Non obstetric risk factors and quality of life in middle-aged women suffering from urinary incontinence. Rev Cuba Ginecol y Obstet 2014; 40: 119–135.[On line] | Link |
Rodríguez Adams, EL. Non obstetric risk factors and quality of life in middle-aged women suffering from urinary incontinence. Rev Cuba Ginecol y Obstet 2014; 40: 119–135.[On line] | Link | Instituto Nacional de Estadísticas. Publicación Estadísticas Vitales, 2017. 2019. [On line]
| Link |
Instituto Nacional de Estadísticas. Publicación Estadísticas Vitales, 2017. 2019. [On line]
| Link | Ministerio de Salud de Chile. Departamento de Estadisticas e Informacion de Salud. Registro estadístico mensual. Atencion de maternidad.2018. [On line] | Link |
Ministerio de Salud de Chile. Departamento de Estadisticas e Informacion de Salud. Registro estadístico mensual. Atencion de maternidad.2018. [On line] | Link | Bascur-Castillo C, Araneda-Gatica V, Castro-Arias H, Carrasco-Portiño M, Ruiz-Cantero MT. Determinants in the process of seeking help for urinary incontinence in the Chilean health system. Int J Gynaecol Obstet. 2019 Jan;144(1):103-111. | CrossRef | PubMed |
Bascur-Castillo C, Araneda-Gatica V, Castro-Arias H, Carrasco-Portiño M, Ruiz-Cantero MT. Determinants in the process of seeking help for urinary incontinence in the Chilean health system. Int J Gynaecol Obstet. 2019 Jan;144(1):103-111. | CrossRef | PubMed | Cerruto MA, Asimakopoulos AD, Artibani W, Del Popolo G, La Martina M, Carone R, et al. Insight into new potential targets for the treatment of overactive bladder and detrusor overactivity. Urol Int. 2012;89(1):1-8. | CrossRef | PubMed |
Cerruto MA, Asimakopoulos AD, Artibani W, Del Popolo G, La Martina M, Carone R, et al. Insight into new potential targets for the treatment of overactive bladder and detrusor overactivity. Urol Int. 2012;89(1):1-8. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








