Key Words: diabetic foot, hospital care, length of hospital stay, public health, peru
Abstract
Introduction
Diabetic foot is one of the main complications of diabetes mellitus; however, in hospitals of provinces from Perú, the relationship of this condition with hospital stay has not been calculated.
Objective
To determine the association between hospitalization time and diabetic foot in three hospitals from Cusco, Perú.
Methods
A cross-sectional study of secondary data analysis was conducted. We analyzed the data of patients with type 2 diabetes mellitus admitted to the internal medicine service between January and December 2016, in three tertiary hospitals in Cusco, Peru. Correlation coefficients and p-values were calculated using generalized linear models, with Gaussian family and identity function, adjusted by intervening variables. Values of p < 0.05 were considered statistically significant.
Results
Of the 153 patients, 14% (21) had a diabetic foot diagnosis, and their median age was 61 years (interquartile range 56 to 68). Those who had a diabetic foot had on average 20 hospitalization days. A strong association was found between a diabetic foot and the number of hospitalization days (17 days more, p = 0.003); adjusted by six variables. Those patients with a history of hypertension had more hospitalization days (10 days more, p = 0.011) and those admitted to a hospital of the Ministry of Health, had fewer hospitalization days (10 days less, p = 0.032).
Conclusion
The group of patients with diabetic foot had a longer hospitalization time. The longer hospitalization time could be due to complications of the disease or difficulties in management.
|
Key ideas
|
Introduction
Diabetic foot is one of the most important complications of diabetes mellitus. Around 25% of affected people will develop a foot ulcer during their lifetime, being more frequent in the age group 45-65 years[1]. In Peru, a diabetes prevalence of 7% has been reported in 2012[2], as well as a mortality of 3.9% in 2014[3].
According to an epidemiological surveillance report including about 3000 patients with diabetes from different hospitals in Peru, 30% of these patients experienced some vascular complications, having diabetic foot a prevalence of 6%[2].
Diabetic foot is one of the most disabling complications of diabetes. Local institutions such as the Medical Association of Peru (Colegio Médico del Perú) have assessed this situation and are creating strategies for its better handling[4]. This complication represents a higher disease burden and additional costs to the healthcare system[5],[6]. Patients are susceptible to inadequate management, risk of limb amputation, concomitant infections, and ulcers. These events increase the morbidity and mortality of those who suffer from this disease[7], resulting in high readmission rates and longer length of hospital stay[8].
There are few published studies in the provinces of Peru associating this complication with length of hospital stay. Thus, the objective of our study was to estimate the association between length of hospital stay and having diabetic foot among patients with type 2 diabetes admitted to three hospitals in Cusco (Peru) during 2016.
Methods
Design and population
We conducted an analytical cross-sectional study involving secondary data analysis of a previously published study[9], in inpatients between 1 January to 31 December 2016 with diagnosis of type 2 diabetes in three third-level regional reference hospitals in the city of Cusco, Peru: “Adolfo Guevara Velasco” National Hospital (establishment that belongs to the social security -EsSalud- and receives monthly contributions from its policy holders as opposed to other healthcare establishments in Cusco); Regional Hospital of Cusco; and “Antonio Lorena” Hospital, both hospitals of the Peruvian Ministry of Health (providing services mainly to people with integrated health insurance). It is important to study this population because Cusco is one of the main cities in the Andes of southern Peru where local patients as well as those referred from other Andean, and even Jungle, cities are treated. The entire data found in census sampling was used.
Selection of participants
We included all patients diagnosed with type 2 diabetes hospitalized in the internal medicine service in any of the hospitals above mentioned during 2016. They were then included in two groups: i) with diagnosis of diabetic foot, and ii) with other diagnoses different to the diabetic foot. Patients admitted only to be subjected to diagnostic or therapeutic procedures (renal biopsy, peritoneal dialysis catheter placement, pulses with corticoids) were excluded.
Study variables
To determine if a patient suffered from type 2 diabetes, we used the American Diabetes Association criteria. A physician, a doctor of internal medicine or an endocrinologist confirmed the disease. This diagnosis could be done in emergency or outpatient clinic[10]. The variable of interest was having diabetic foot, which was determined with the medical diagnosis recorded in the medical chart. The length of hospital stay was considered based on the number of hospitalization days (days in bed from admission to discharge). In addition, we included socio-educational variables: sex, age and education level, and clinical variables: length of time diagnosed with type 2 diabetes, and history of hypertension. We considered these variables because of their greatest relation to diabetic foot. As this was a secondary analysis of data, we could not access other variables that could have been involved in the main association.
Data analysis
The primary database was reviewed[9], and all variables described for this study were then selected. Data was then entered into a database in Microsoft Excel (version for Windows 2013), where information was organized. At this stage, the data quality control was performed.
To analyze the data, we used the statistical program Stata v.11.1 (StataCorp LP, College Station, TX, USA). We made a descriptive analysis of categorical variables using absolute and relative frequencies. To describe numerical variables, the median and the interquartile range were used according to the previous assessment of normality assumption using the Shapiro Wilk test. A bivariate analysis was applied to compare the groups of patients with and without diabetic foot (using the Chi square test for categorical variables and the rank sum test for quantitative variables) to determine if there were differences.
Analytical statistics were generated using the variable “hospitalization days” according to the variable of interest “having diabetic foot”. For this, we calculated the correlation coefficients and p-values by using generalized linear models with Gaussian family and identity link function (this is because the main variable was quantitative – number of hospitalization days). P - values < 0.05 were considered statistically significant.
Ethics
The primary study which database was used was reviewed and approved by the Ethics and Research Committee of the hospitals where this research was conducted: Red Asistencial (Healthcare Network) de EsSalud, Cusco (N° 016-CI-GRACU-ESSALUD-2017), “Antonio Lorena” Hospital of Cusco (N° 03-2017-UDPH-HAL-C), and Regional Hospital of Cusco (N° 029-2017-HRC-DE). In addition, we followed the recommendations and guidelines for Good Clinical Practice for Medical Research involving human subjects. We removed names from databases after collecting information from every patient. An anonymous list was used for the analysis.
Results
Of the 153 patients, 13.7% (21) of inpatients were diagnosed with diabetic foot; 16.7% of male patients had diabetic foot. The median age of patients with diabetic foot was 61 years (interquartile range 56 to 68), and 16.1% of patients suffered from hypertension and diabetic foot. The median length of time with diabetes, 13 years, was higher among patients with diabetic foot (interquartile range 7 to 20). Hospitals of the Ministry of Health: Regional (27.5%) and “Antonio Lorena” (11.5%) had the greatest number of patients with diabetic foot in comparison with “Adolfo Guevara Velasco” Hospital (2.0%) (Table 1)
The median number of hospitalization days among those with diabetic foot was 20 days (interquartile range: 14 to 31 days). For those without diabetic foot, the median was 9 days (interquartile range: 5 to 14 days) (Figure 1).
The average number of hospitalization days was 32 days. We found a significant association between having diabetic foot and the number of hospitalization days (17.0 days longer; 95% confidence interval: 5.7 to 28.3 days; p = 0.003); adjusted for six variables. Also, the number of hospitalization days for those who had a history of hypertension was higher (9.6 days longer, 95% confidence interval: 2.2 to 17.1 days; p = 0.011), and those at “Antonio Lorena” Hospital had a shorter length of hospital stay (9.6 days shorter, 95% confidence interval: 18.4 to -0.8 days; p = 0.032) (Table 2).
Discussion
According to the main finding of our research, there is a significant statistical difference in the length of hospital stay between patients with and without diabetic foot. Two systematic reviews conducted by the International Working Group on the Diabetic Foot confirm this finding[11],[12].
study in Singapore reported that the average length of hospital stays of patients with amputations due to diabetic foot was 6.5 times longer (53 days) than that of non-surgically treated diabetic patients[13]. In addition, a study in Korea reported that the average length of hospital stay was prolonged (37 days) for surgical drainage of ulcers8, and another study reported that wound severity is associated to a length of hospital stay longer than 5 weeks[14].
These studies confirm that treatment of diabetic foot involves a prolonged length of hospital stay. Therefore, it is considered a public health issue as it results in greater time and cost for a complication that can be preventable with proper education and monitoring. On the contrary, a study in the United States of America reported that the average length of hospital stay for this type of patients was 6 to 7 days in 2005-2010[15]. This may be due to the characteristics of the population itself, and better healthcare systems in the United States.
Another important finding was that the length of hospital stay was also associated with having hypertension, a concomitant disease closely linked to type 2 diabetes. According to a recent report in different Peruvian cities, hypertension is associated with type 2 diabetes, especially when it comes to drug treatment of both diseases. This report showing that there is an important number of patients who suffer from both diseases and do not receive proper treatment[16]. This has also been reported in hospitals in developed countries[17], where it has been shown that both diseases coexist in a great number of patients[18],[19]. There are reports of this association in countries such as China[20], where more than half of the patients with hypertension had also type 2 diabetes, which may be due to endothelial dysfunctions present in acute hyperglycemia[21],[22].
A study in Mexico reported an association of 47% between diabetes and hypertension[23]. Being a country with a similar context to ours, it shows the need to increase the efforts to prevent and treat non-transmissible chronic diseases in our population. As several studies state, and as shown by the Latin American consensus on hypertension in patients with type 2 diabetes and metabolic syndrome, these are the new epidemics of the 21st century[24].
The length of hospital stay was shorter in a hospital of the Ministry of Health (“Antonio Lorena”). This may be due to a lower severity of the disease of admitted patients or to a poorer management of this disease, which may show that a timely and proper management could greatly influence the outcome of many diseases[24]. We believe that it is important to promote primary prevention, especially if there are several reports in our setting showing that several groups of the economically active population are starting to have metabolic disorders[25],[26],[27], and that this may result in them being the new patients with chronic illnesses within some years.
A limitation of this study was information bias. Because this is a secondary data analysis, we couldn’t obtain additional information that could be used to adjust the association. However, most of the variables used were important for this association. In addition, we assessed different socio-economic populations (patients from hospitals of the Ministry of Health and the social security) of a province in Peru. A statistical limitation was using the variable of hospitalization days in its raw form when this should be normalized to be used with the identity link function. However, when trying to normalize it (logarithmic power), only tenths and hundredths of their values of association changed when performing the same analysis for all the variables. Thus, we decided not to normalize this variable, so it could be more easily interpreted (even though that would improve its use with the link function and residues). On the other hand, it is important to highlight that some confidence intervals were wide (for those having diabetic foot and hypertension). This may be due to a strong association between these variables and the hospitalization days, and due to the small sample size.
Conclusions
We concluded that in the study population there is a significant association between a longer length of hospital stay in Type 2 diabetic mellitus patients and having diabetic foot. In addition, that the number of hospitalization days was also associated to suffering from hypertension, and the population admitted to one of the hospitals under study.
We believe that Peruvian institutions engaged in health promotion and prevention should lead initiatives that promote better health styles, timely detection, and proper treatment of populations in risk of suffering these diseases as well as the development of financial investigations to determine health costs of this disease in our context[28],[29].
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Author contributions
CRM: conceptualization, data management, formal analysis, research, methodology, project administration, supervision, data submission, manuscript preparation (elaboration of original draft), writing (revision and editing). LP-T: conceptualization, data management, research, methodology, manuscript preparation (elaboration of original draft), writing (revision and editing). LM-C: conceptualization, data management, research, manuscript preparation (elaboration of original draft), writing (revision and editing). NA-A: research, methodology, project administration, supervision, data submission, manuscript preparation (elaboration of original draft), writing (revision and editing). EAR-A: research, project administration, writing (revision and editing). MEO-L: research, project administration, writing (revision and editing).
Competing interests
The authors have completed the ICMJE Conflict of Interest declaration form and declare that they have not received funding for the report, have no financial relationships with organizations that might have an interest in the published article in the last three years, and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the main author or the editorial management of the Journal.
Funding
The authors state that there were no external sources of funding.
Ethics statement
The primary study which database was used was reviewed and approved by the Ethics and Research Committee of the hospitals were this research was conducted: Red Asistencial (Healthcare Network) de EsSalud, Cusco (N° 016-CI-GRACU-ESSALUD-2017), “Antonio Lorena” Hospital of Cusco (N° 03-2017-UDPH-HAL-C), and Regional Hospital of Cusco (N° 029-2017-HRC-DE).
Data availability
This database is available in the Figshare data repository: https://doi.org/10.6084/m9.figshare.5606041.v1

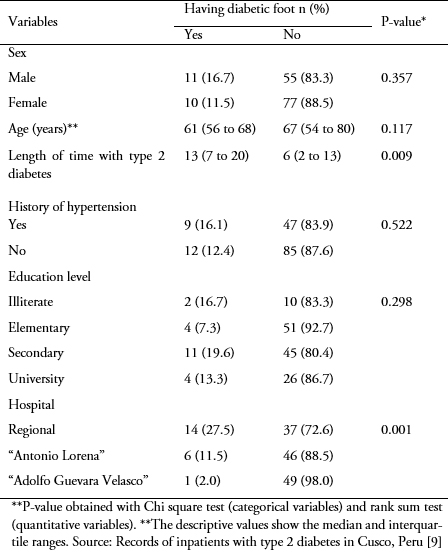 Table 1. Characteristics of patients with type 2 diabetes according to their diagnosis of diabetic foot.
Table 1. Characteristics of patients with type 2 diabetes according to their diagnosis of diabetic foot.

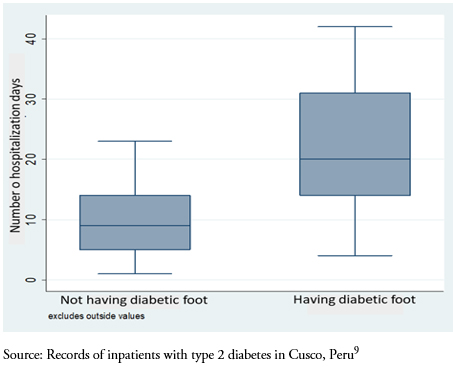 Figure 1. Number of hospitalization days of patients with type 2 diabetes having and not having diabetic foot.
Figure 1. Number of hospitalization days of patients with type 2 diabetes having and not having diabetic foot.

 Table 2. Multivariate analysis of hospitalization days of patients with type 2 diabetes having and not having diabetic foot.
Table 2. Multivariate analysis of hospitalization days of patients with type 2 diabetes having and not having diabetic foot.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introducción
El pie diabético es una de las principales complicaciones de la diabetes mellitus. Sin embargo, en hospitales de provincias en Perú no se ha calculado la relación de este padecimiento con la estancia hospitalaria.
Objetivos
Determinar la asociación entre el tiempo de hospitalización y el padecer pie diabético en tres hospitales de Cusco, Perú.
Métodos
Se realizó un estudio transversal analítico con estudio de datos secundarios. Se analizaron los datos de los pacientes con diabetes mellitus tipo 2 que ingresaron al servicio de medicina interna entre enero y diciembre del año 2016, en tres hospitales de tercer nivel de Cusco, Perú. Se calcularon los coeficientes de correlación y los valores p, mediante el uso de los modelos lineales generalizados, con familia Gaussian y función de enlace identity, ajustado por variables intervinientes. Se consideró estadísticamente significativos los valores p < 0,05.
Resultados
De los 153 pacientes, 14% (21) tuvo un diagnóstico de pie diabético y su mediana de edad fue 61 años (rango intercuartílico de 56 a 68). Aquellos que tenían pie diabético tuvieron en promedio 20 días de hospitalización. Se encontró una fuerte asociación entre el padecer pie diabético y la cantidad de días de hospitalización (17 días más, p = 0,003); ajustado por seis variables. Aquellos pacientes con antecedente de hipertensión arterial tuvieron más días de hospitalización (10 días más, p = 0,011) y los que se internaron en un hospital del Ministerio de Salud tuvieron menor cantidad de días hospitalizados (10 días menos, p = 0,032).
Conclusión
El grupo de pacientes con pie diabético tuvo un mayor tiempo de hospitalización. El mayor tiempo de hospitalización podría deberse a las complicaciones de la enfermedad o dificultades en el manejo.
 Authors:
Christian R. Mejia[1], Liz Paucar-Tito[2], Luz Morales-Concha[2], Noé Atamari-Anahui[3], Evelina Andrea Rondón-Abuhadba[4], Marco Edmundo Ordoñez-Linares[4]
Authors:
Christian R. Mejia[1], Liz Paucar-Tito[2], Luz Morales-Concha[2], Noé Atamari-Anahui[3], Evelina Andrea Rondón-Abuhadba[4], Marco Edmundo Ordoñez-Linares[4]
Affiliation:
[1] Coordinación de Investigación, Universidad Continental, Huancayo, Perú.
[2] Asociación Científica de Estudiantes de Medicina Humana del Cusco, Escuela de Medicina Humana, Facultad de Ciencias de la Salud, Universidad Nacional de San Antonio Abad del Cusco, Cusco, Perú.
[3] Unidad de Investigación para la Generación y Síntesis de Evidencias en Salud, Universidad San Ignacio de Loyola, Lima, Perú.
[4] Escuela de Medicina Humana, Facultad de Ciencias de la Salud, Universidad Nacional de San Antonio Abad del Cusco, Cusco, Perú.
E-mail: noe.atamari@gmail.com
Author address:
[1] Avenida La Fontana 550
La Molina
Lima
Perú

Citation: Mejia CR, Paucar-Tito L, Morales-Concha L, Atamari-Anahui N, Rondón-Abuhadba EA, Ordoñez-Linares ME. Association between hospitalization stay and diabetic foot: an analytical cross-sectional study in three Peruvian hospitals. Medwave 2018;18(7):e7336 doi: 10.5867/medwave.2018.07.7336
Submission date: 5/7/2018
Acceptance date: 19/10/2018
Publication date: 21/11/2018
Origin: not requested
Type of review: reviewed by five external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- García-Herrera AL. El pie diabético en cifras. Apuntes de una epidemia. Rev Médica Electrónica. 2016;38(4):514-6. | Link |
- Ramos W, López T, Revilla L, More L, Huamaní M, Pozo M. [Results of the epidemiological surveillance of diabetes mellitus in hospitals in Peru, 2012]. Rev Peru Med Exp Salud Publica. 2014;31(1):9-15. | PubMed |
- Atamari-Anahui N, Ccorahua-Rios MS, Taype-Rondan A, Mejia CR. Mortalidad atribuida a diabetes mellitus registrada en el Ministerio de Salud de Perú, 2005-2014. Rev Panam Salud Publica. 2018;42:e50. | Link |
- Colegio Médico del Perú. Tratamiento de pie diabético genera altos costos al sistema de salud. 2017 [on line]. | Link |
- Søndergaard LN, Christensen AB, Vinding AL, Kjær IL, Larsen P. Elevated costs and high one-year mortality in patients with diabetic foot ulcers after surgery. Dan Med J. 2015 Apr;62(4):A5050. | PubMed |
- Petrakis I, Kyriopoulos IJ, Ginis A, Athanasakis K. Losing a foot versus losing a dollar; a systematic review of cost studies in diabetic foot complications. Expert Rev Pharmacoecon Outcomes Res. 2017 Apr;17(2):165-180. | CrossRef | PubMed |
- Quilici MT, Del Fiol Fde S, Vieira AE, Toledo MI. Risk Factors for Foot Amputation in Patients Hospitalized for Diabetic Foot Infection. J Diabetes Res. 2016;2016:8931508. | CrossRef | PubMed |
- Kim TG, Moon SY, Park MS, Kwon SS, Jung KJ, Lee T, et al. Factors Affecting Length of Hospital Stay and Mortality in Infected Diabetic Foot Ulcers Undergoing Surgical Drainage without Major Amputation. J Korean Med Sci. 2016 Jan;31(1):120-4. | CrossRef | PubMed |
- Atamari-Anahui N, Martinez-Ninanqui FW, Paucar-Tito L, Morales-Concha L, Miranda-Chirau A, Gamarra-Contreras MA, et al. Factors associated to inpatient mortality rates in type-2-diabetic patients: a cross-sectional analytical study in three Peruvian hospitals. Medwave. 2017 Dec 5;17(9):e7097. | CrossRef | PubMed |
- American American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2017;40(Supplement 1):S11-24. | Link |
- Hinchliffe RJ, Valk GD, Apelqvist J, Armstrong DG, Bakker K, Game FL, et al. A systematic review of the effectiveness of interventions to enhance the healing of chronic ulcers of the foot in diabetes. Diabetes Metab Res Rev. 2008 May-Jun;24 Suppl 1:S119-44. | CrossRef | PubMed |
- Game FL, Hinchliffe RJ, Apelqvist J, Armstrong DG, Bakker K, Hartemann A, et al. A systematic review of interventions to enhance the healing of chronic ulcers of the foot in diabetes. Diabetes Metab Res Rev. 2012 Feb;28 Suppl 1:119-41. | CrossRef | PubMed |
- Tan JH, Hong CC, Shen L, Tay EY, Lee JK, Nather A. Costs of Patients Admitted for Diabetic Foot Problems. Ann Acad Med Singapore. 2015 Dec;44(12):567-70. | PubMed |
- Choi SK, Kim CK, Jo DI, Lee MC, Kim JN, Choi HG, et al. Factors Associated with a Prolonged Length of Hospital Stay in Patients with Diabetic Foot: A Single-Center Retrospective Study. Arch Plast Surg. 2017 Nov;44(6):539-544. | CrossRef | PubMed |
- Hicks CW, Selvarajah S, Mathioudakis N, Perler BA, Freischlag JA, Black JH 3rd, et al. Trends and determinants of costs associated with the inpatient care of diabetic foot ulcers. J Vasc Surg. 2014 Nov;60(5):1247-1254.e2. | CrossRef | PubMed |
- Mejia CR, Failoc-Rojas VE, So E, Cervantes C, Aspajo AJ, Leandro JG, et al. Characteristics and Factors Associated With Antihypertensive Medication Use in Patients Attending Peruvian Health Facilities. Cureus. 2017 Feb 3;9(2):e1011. | CrossRef | PubMed |
- Sanders JS, Skipworth JR, Cooper JA, Brull DJ, Humphries SE, Mythen M, et al. Duration of preceding hypertension is associated with prolonged length of ICU stay. Int J Cardiol. 2012 May 31;157(2):180-4. | CrossRef | PubMed |
- Lu K, Ding R, Wang L, Wu S, Chen J, Hu D. Association between prevalence of hypertension and components of metabolic syndrome: the data from Kailuan community. Clin Exp Hypertens. 2015;37(4):303-7. | CrossRef | PubMed |
- Weinstock RS, Drews KL, Caprio S, Leibel NI, McKay SV, Zeitler PS. Metabolic syndrome is common and persistent in youth-onset type 2 diabetes: Results from the TODAY clinical trial. Obesity (Silver Spring). 2015 Jul;23(7):1357-61. | CrossRef | PubMed |
- Loader J, Montero D, Lorenzen C, Watts R, Méziat C, Reboul C, et al. Acute Hyperglycemia Impairs Vascular Function in Healthy and Cardiometabolic Diseased Subjects: Systematic Review and Meta-Analysis. Arterioscler Thromb Vasc Biol. 2015 Sep;35(9):2060-72. | CrossRef | PubMed |
- Tie HT, Shi R, Li ZH, Zhang M, Zhang C, Wu QC. Risk of major adverse cardiovascular events in patients with metabolic syndrome after revascularization: A meta-analysis of eighteen cohorts with 18,457 patients. Metabolism. 2015 Oct;64(10):1224-34. | CrossRef | PubMed |
- Hernández-Ávila M, Gutiérrez JP, Reynoso-Noverón N. [Diabetes mellitus in Mexico. Status of the epidemic]. Salud Publica Mex. 2013;55 Suppl 2:S129-36. | PubMed |
- Lopez-Jaramillo P, Sánchez RA, Díaz M, Cobos L, Bryce A, Parra Carrillo JZ, et al. Consenso latinoamericano de hipertensión en pacientes con diabetes tipo 2 y síndrome metabólico. Clínica e Investig en Arterioscler. 2014;26(2):85-103. | Link |
- Montiel-Jarquín ÁJ, García Villaseñor A, Castillo Rodríguez C, Romero-Figueroa MS, Etchegaray-Morales I, García-Cano E, et al. Costes directos de atención médica del pie diabético en el segundo nivel de atención médica. Rev Chil Cir. 2017;69(2):118-23. | Link |
- Mejia CR, Espejo RP, Zevallos KR, Castro TA, Vargas AB, Millan GK. Factores asociados al riesgo cardiovascular según Framingham en taxistas de una empresa de Huancayo, Perú. Rev Asoc Esp Espec En Med Trab. 2016;25(1):19-25. | Link |
- Mejia CR, Quiñones-Laveriano DM, Cruzalegui-Solari CC, Arriola-Quiroz I, Perez-Perez L, Gomero R. Edad como factor de riesgo para desarrollar síndrome metabólico en trabajadores mineros a gran altura. Rev Argent Endocrinol Metab. 2016;53(1):29-35. | Link |
- Mejia CR, Chacón JI, Cavero M, Orihuela R, Orihuela E. Factores sociolaborales asociados al riesgo cardiovascular según el score de Framingham en trabajadores de Lima, 2015. Rev Argent Endocrinol Metab. 2016;53(3):84-9. | CrossRef |
- Cárdenas MK, Mirelman AJ, Galvin CJ, Lazo-Porras M, Pinto M, Miranda JJ, et al. The cost of illness attributable to diabetic foot and cost-effectiveness of secondary prevention in Peru. BMC Health Serv Res. 2015 Oct 26;15:483. | CrossRef | PubMed |
- Atamari-Anahui N, Sucasaca-Rodríguez C, Contreras-Sotomayor S, Aguilar-Muñiz A, Velásquez-Cuentas L, Mejía CR. Factores asociados a las prácticas de publicación de médicos que laboran en hospitales de Cusco, Perú. Rev Cuba Inf En Cienc Salud. 2016;27(4):531-44. | Link |
 García-Herrera AL. El pie diabético en cifras. Apuntes de una epidemia. Rev Médica Electrónica. 2016;38(4):514-6. | Link |
García-Herrera AL. El pie diabético en cifras. Apuntes de una epidemia. Rev Médica Electrónica. 2016;38(4):514-6. | Link | Ramos W, López T, Revilla L, More L, Huamaní M, Pozo M. [Results of the epidemiological surveillance of diabetes mellitus in hospitals in Peru, 2012]. Rev Peru Med Exp Salud Publica. 2014;31(1):9-15. | PubMed |
Ramos W, López T, Revilla L, More L, Huamaní M, Pozo M. [Results of the epidemiological surveillance of diabetes mellitus in hospitals in Peru, 2012]. Rev Peru Med Exp Salud Publica. 2014;31(1):9-15. | PubMed | Atamari-Anahui N, Ccorahua-Rios MS, Taype-Rondan A, Mejia CR. Mortalidad atribuida a diabetes mellitus registrada en el Ministerio de Salud de Perú, 2005-2014. Rev Panam Salud Publica. 2018;42:e50. | Link |
Atamari-Anahui N, Ccorahua-Rios MS, Taype-Rondan A, Mejia CR. Mortalidad atribuida a diabetes mellitus registrada en el Ministerio de Salud de Perú, 2005-2014. Rev Panam Salud Publica. 2018;42:e50. | Link | Colegio Médico del Perú. Tratamiento de pie diabético genera altos costos al sistema de salud. 2017 [on line]. | Link |
Colegio Médico del Perú. Tratamiento de pie diabético genera altos costos al sistema de salud. 2017 [on line]. | Link | Søndergaard LN, Christensen AB, Vinding AL, Kjær IL, Larsen P. Elevated costs and high one-year mortality in patients with diabetic foot ulcers after surgery. Dan Med J. 2015 Apr;62(4):A5050. | PubMed |
Søndergaard LN, Christensen AB, Vinding AL, Kjær IL, Larsen P. Elevated costs and high one-year mortality in patients with diabetic foot ulcers after surgery. Dan Med J. 2015 Apr;62(4):A5050. | PubMed | Petrakis I, Kyriopoulos IJ, Ginis A, Athanasakis K. Losing a foot versus losing a dollar; a systematic review of cost studies in diabetic foot complications. Expert Rev Pharmacoecon Outcomes Res. 2017 Apr;17(2):165-180. | CrossRef | PubMed |
Petrakis I, Kyriopoulos IJ, Ginis A, Athanasakis K. Losing a foot versus losing a dollar; a systematic review of cost studies in diabetic foot complications. Expert Rev Pharmacoecon Outcomes Res. 2017 Apr;17(2):165-180. | CrossRef | PubMed | Quilici MT, Del Fiol Fde S, Vieira AE, Toledo MI. Risk Factors for Foot Amputation in Patients Hospitalized for Diabetic Foot Infection. J Diabetes Res. 2016;2016:8931508. | CrossRef | PubMed |
Quilici MT, Del Fiol Fde S, Vieira AE, Toledo MI. Risk Factors for Foot Amputation in Patients Hospitalized for Diabetic Foot Infection. J Diabetes Res. 2016;2016:8931508. | CrossRef | PubMed | Kim TG, Moon SY, Park MS, Kwon SS, Jung KJ, Lee T, et al. Factors Affecting Length of Hospital Stay and Mortality in Infected Diabetic Foot Ulcers Undergoing Surgical Drainage without Major Amputation. J Korean Med Sci. 2016 Jan;31(1):120-4. | CrossRef | PubMed |
Kim TG, Moon SY, Park MS, Kwon SS, Jung KJ, Lee T, et al. Factors Affecting Length of Hospital Stay and Mortality in Infected Diabetic Foot Ulcers Undergoing Surgical Drainage without Major Amputation. J Korean Med Sci. 2016 Jan;31(1):120-4. | CrossRef | PubMed | Atamari-Anahui N, Martinez-Ninanqui FW, Paucar-Tito L, Morales-Concha L, Miranda-Chirau A, Gamarra-Contreras MA, et al. Factors associated to inpatient mortality rates in type-2-diabetic patients: a cross-sectional analytical study in three Peruvian hospitals. Medwave. 2017 Dec 5;17(9):e7097. | CrossRef | PubMed |
Atamari-Anahui N, Martinez-Ninanqui FW, Paucar-Tito L, Morales-Concha L, Miranda-Chirau A, Gamarra-Contreras MA, et al. Factors associated to inpatient mortality rates in type-2-diabetic patients: a cross-sectional analytical study in three Peruvian hospitals. Medwave. 2017 Dec 5;17(9):e7097. | CrossRef | PubMed | American American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2017;40(Supplement 1):S11-24. | Link |
American American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2017;40(Supplement 1):S11-24. | Link | Hinchliffe RJ, Valk GD, Apelqvist J, Armstrong DG, Bakker K, Game FL, et al. A systematic review of the effectiveness of interventions to enhance the healing of chronic ulcers of the foot in diabetes. Diabetes Metab Res Rev. 2008 May-Jun;24 Suppl 1:S119-44. | CrossRef | PubMed |
Hinchliffe RJ, Valk GD, Apelqvist J, Armstrong DG, Bakker K, Game FL, et al. A systematic review of the effectiveness of interventions to enhance the healing of chronic ulcers of the foot in diabetes. Diabetes Metab Res Rev. 2008 May-Jun;24 Suppl 1:S119-44. | CrossRef | PubMed | Game FL, Hinchliffe RJ, Apelqvist J, Armstrong DG, Bakker K, Hartemann A, et al. A systematic review of interventions to enhance the healing of chronic ulcers of the foot in diabetes. Diabetes Metab Res Rev. 2012 Feb;28 Suppl 1:119-41. | CrossRef | PubMed |
Game FL, Hinchliffe RJ, Apelqvist J, Armstrong DG, Bakker K, Hartemann A, et al. A systematic review of interventions to enhance the healing of chronic ulcers of the foot in diabetes. Diabetes Metab Res Rev. 2012 Feb;28 Suppl 1:119-41. | CrossRef | PubMed | Tan JH, Hong CC, Shen L, Tay EY, Lee JK, Nather A. Costs of Patients Admitted for Diabetic Foot Problems. Ann Acad Med Singapore. 2015 Dec;44(12):567-70. | PubMed |
Tan JH, Hong CC, Shen L, Tay EY, Lee JK, Nather A. Costs of Patients Admitted for Diabetic Foot Problems. Ann Acad Med Singapore. 2015 Dec;44(12):567-70. | PubMed | Choi SK, Kim CK, Jo DI, Lee MC, Kim JN, Choi HG, et al. Factors Associated with a Prolonged Length of Hospital Stay in Patients with Diabetic Foot: A Single-Center Retrospective Study. Arch Plast Surg. 2017 Nov;44(6):539-544. | CrossRef | PubMed |
Choi SK, Kim CK, Jo DI, Lee MC, Kim JN, Choi HG, et al. Factors Associated with a Prolonged Length of Hospital Stay in Patients with Diabetic Foot: A Single-Center Retrospective Study. Arch Plast Surg. 2017 Nov;44(6):539-544. | CrossRef | PubMed | Hicks CW, Selvarajah S, Mathioudakis N, Perler BA, Freischlag JA, Black JH 3rd, et al. Trends and determinants of costs associated with the inpatient care of diabetic foot ulcers. J Vasc Surg. 2014 Nov;60(5):1247-1254.e2. | CrossRef | PubMed |
Hicks CW, Selvarajah S, Mathioudakis N, Perler BA, Freischlag JA, Black JH 3rd, et al. Trends and determinants of costs associated with the inpatient care of diabetic foot ulcers. J Vasc Surg. 2014 Nov;60(5):1247-1254.e2. | CrossRef | PubMed | Mejia CR, Failoc-Rojas VE, So E, Cervantes C, Aspajo AJ, Leandro JG, et al. Characteristics and Factors Associated With Antihypertensive Medication Use in Patients Attending Peruvian Health Facilities. Cureus. 2017 Feb 3;9(2):e1011. | CrossRef | PubMed |
Mejia CR, Failoc-Rojas VE, So E, Cervantes C, Aspajo AJ, Leandro JG, et al. Characteristics and Factors Associated With Antihypertensive Medication Use in Patients Attending Peruvian Health Facilities. Cureus. 2017 Feb 3;9(2):e1011. | CrossRef | PubMed | Sanders JS, Skipworth JR, Cooper JA, Brull DJ, Humphries SE, Mythen M, et al. Duration of preceding hypertension is associated with prolonged length of ICU stay. Int J Cardiol. 2012 May 31;157(2):180-4. | CrossRef | PubMed |
Sanders JS, Skipworth JR, Cooper JA, Brull DJ, Humphries SE, Mythen M, et al. Duration of preceding hypertension is associated with prolonged length of ICU stay. Int J Cardiol. 2012 May 31;157(2):180-4. | CrossRef | PubMed | Lu K, Ding R, Wang L, Wu S, Chen J, Hu D. Association between prevalence of hypertension and components of metabolic syndrome: the data from Kailuan community. Clin Exp Hypertens. 2015;37(4):303-7. | CrossRef | PubMed |
Lu K, Ding R, Wang L, Wu S, Chen J, Hu D. Association between prevalence of hypertension and components of metabolic syndrome: the data from Kailuan community. Clin Exp Hypertens. 2015;37(4):303-7. | CrossRef | PubMed | Weinstock RS, Drews KL, Caprio S, Leibel NI, McKay SV, Zeitler PS. Metabolic syndrome is common and persistent in youth-onset type 2 diabetes: Results from the TODAY clinical trial. Obesity (Silver Spring). 2015 Jul;23(7):1357-61. | CrossRef | PubMed |
Weinstock RS, Drews KL, Caprio S, Leibel NI, McKay SV, Zeitler PS. Metabolic syndrome is common and persistent in youth-onset type 2 diabetes: Results from the TODAY clinical trial. Obesity (Silver Spring). 2015 Jul;23(7):1357-61. | CrossRef | PubMed | Loader J, Montero D, Lorenzen C, Watts R, Méziat C, Reboul C, et al. Acute Hyperglycemia Impairs Vascular Function in Healthy and Cardiometabolic Diseased Subjects: Systematic Review and Meta-Analysis. Arterioscler Thromb Vasc Biol. 2015 Sep;35(9):2060-72. | CrossRef | PubMed |
Loader J, Montero D, Lorenzen C, Watts R, Méziat C, Reboul C, et al. Acute Hyperglycemia Impairs Vascular Function in Healthy and Cardiometabolic Diseased Subjects: Systematic Review and Meta-Analysis. Arterioscler Thromb Vasc Biol. 2015 Sep;35(9):2060-72. | CrossRef | PubMed | Tie HT, Shi R, Li ZH, Zhang M, Zhang C, Wu QC. Risk of major adverse cardiovascular events in patients with metabolic syndrome after revascularization: A meta-analysis of eighteen cohorts with 18,457 patients. Metabolism. 2015 Oct;64(10):1224-34. | CrossRef | PubMed |
Tie HT, Shi R, Li ZH, Zhang M, Zhang C, Wu QC. Risk of major adverse cardiovascular events in patients with metabolic syndrome after revascularization: A meta-analysis of eighteen cohorts with 18,457 patients. Metabolism. 2015 Oct;64(10):1224-34. | CrossRef | PubMed | Hernández-Ávila M, Gutiérrez JP, Reynoso-Noverón N. [Diabetes mellitus in Mexico. Status of the epidemic]. Salud Publica Mex. 2013;55 Suppl 2:S129-36. | PubMed |
Hernández-Ávila M, Gutiérrez JP, Reynoso-Noverón N. [Diabetes mellitus in Mexico. Status of the epidemic]. Salud Publica Mex. 2013;55 Suppl 2:S129-36. | PubMed | Lopez-Jaramillo P, Sánchez RA, Díaz M, Cobos L, Bryce A, Parra Carrillo JZ, et al. Consenso latinoamericano de hipertensión en pacientes con diabetes tipo 2 y síndrome metabólico. Clínica e Investig en Arterioscler. 2014;26(2):85-103. | Link |
Lopez-Jaramillo P, Sánchez RA, Díaz M, Cobos L, Bryce A, Parra Carrillo JZ, et al. Consenso latinoamericano de hipertensión en pacientes con diabetes tipo 2 y síndrome metabólico. Clínica e Investig en Arterioscler. 2014;26(2):85-103. | Link | Montiel-Jarquín ÁJ, García Villaseñor A, Castillo Rodríguez C, Romero-Figueroa MS, Etchegaray-Morales I, García-Cano E, et al. Costes directos de atención médica del pie diabético en el segundo nivel de atención médica. Rev Chil Cir. 2017;69(2):118-23. | Link |
Montiel-Jarquín ÁJ, García Villaseñor A, Castillo Rodríguez C, Romero-Figueroa MS, Etchegaray-Morales I, García-Cano E, et al. Costes directos de atención médica del pie diabético en el segundo nivel de atención médica. Rev Chil Cir. 2017;69(2):118-23. | Link | Mejia CR, Espejo RP, Zevallos KR, Castro TA, Vargas AB, Millan GK. Factores asociados al riesgo cardiovascular según Framingham en taxistas de una empresa de Huancayo, Perú. Rev Asoc Esp Espec En Med Trab. 2016;25(1):19-25. | Link |
Mejia CR, Espejo RP, Zevallos KR, Castro TA, Vargas AB, Millan GK. Factores asociados al riesgo cardiovascular según Framingham en taxistas de una empresa de Huancayo, Perú. Rev Asoc Esp Espec En Med Trab. 2016;25(1):19-25. | Link | Mejia CR, Quiñones-Laveriano DM, Cruzalegui-Solari CC, Arriola-Quiroz I, Perez-Perez L, Gomero R. Edad como factor de riesgo para desarrollar síndrome metabólico en trabajadores mineros a gran altura. Rev Argent Endocrinol Metab. 2016;53(1):29-35. | Link |
Mejia CR, Quiñones-Laveriano DM, Cruzalegui-Solari CC, Arriola-Quiroz I, Perez-Perez L, Gomero R. Edad como factor de riesgo para desarrollar síndrome metabólico en trabajadores mineros a gran altura. Rev Argent Endocrinol Metab. 2016;53(1):29-35. | Link | Mejia CR, Chacón JI, Cavero M, Orihuela R, Orihuela E. Factores sociolaborales asociados al riesgo cardiovascular según el score de Framingham en trabajadores de Lima, 2015. Rev Argent Endocrinol Metab. 2016;53(3):84-9. | CrossRef |
Mejia CR, Chacón JI, Cavero M, Orihuela R, Orihuela E. Factores sociolaborales asociados al riesgo cardiovascular según el score de Framingham en trabajadores de Lima, 2015. Rev Argent Endocrinol Metab. 2016;53(3):84-9. | CrossRef | Cárdenas MK, Mirelman AJ, Galvin CJ, Lazo-Porras M, Pinto M, Miranda JJ, et al. The cost of illness attributable to diabetic foot and cost-effectiveness of secondary prevention in Peru. BMC Health Serv Res. 2015 Oct 26;15:483. | CrossRef | PubMed |
Cárdenas MK, Mirelman AJ, Galvin CJ, Lazo-Porras M, Pinto M, Miranda JJ, et al. The cost of illness attributable to diabetic foot and cost-effectiveness of secondary prevention in Peru. BMC Health Serv Res. 2015 Oct 26;15:483. | CrossRef | PubMed | Atamari-Anahui N, Sucasaca-Rodríguez C, Contreras-Sotomayor S, Aguilar-Muñiz A, Velásquez-Cuentas L, Mejía CR. Factores asociados a las prácticas de publicación de médicos que laboran en hospitales de Cusco, Perú. Rev Cuba Inf En Cienc Salud. 2016;27(4):531-44. | Link |
Atamari-Anahui N, Sucasaca-Rodríguez C, Contreras-Sotomayor S, Aguilar-Muñiz A, Velásquez-Cuentas L, Mejía CR. Factores asociados a las prácticas de publicación de médicos que laboran en hospitales de Cusco, Perú. Rev Cuba Inf En Cienc Salud. 2016;27(4):531-44. | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








