Key Words: type 2 diabetes mellitus, mortality, hospitals, Peru
Abstract
INTRODUCTION
Diabetes mortality has increased in recent years. In Peru, there are few studies on in-hospital mortality due to type 2 diabetes in the provinces.
OBJECTIVE
To determine factors associated to hospital mortality in patients with diabetes mellitus type 2 in three hospitals from Cusco-Peru.
METHODS
An analytical cross-sectional study was performed. All patients with diabetes mellitus type 2 hospitalized in the city of Cusco during the 2016 were included. Socio-educational and clinical characteristics were evaluated, with "death" as the variable of interest. The crude (cPR) and adjusted (aPR) prevalence ratios were estimated using generalized linear models with Poisson family and log link function, with their respective 95% confidence intervals (95% CI). The values p <0.05 were considered significant.
RESULTS
A total of 153 patients were studied; 33.3% (51) died in the hospital. The mortality rate increased when the following factors were associated: age of the patients increased the mortality rate by one-year increments (aPR: 1.02; CI95%: 1.01-1.03; p<0.001); to have been admitted by the emergency service (aPR: 1.93; CI95%: 1.34-2.77; p<0.001); being a patient who is readmitted to the hospital (aPR: 2.01; CI95%: 1.36-2.98; p<0.001); and patients who have had a metabolic in-hospital complication (aPR: 1.61; CI95%: 1.07-2.43; p=0.024) or renal in-hospital complications (aPR: 1.47; CI95%: 1.30-1.67; p<0.001). Conversely, the mortality rate was reduced when admission was due to a urinary tract infection (aPR: 0.50; CI95%: 0.35-0.72; p<0.001); adjusted by seven variables.
CONCLUSIONS
A third of hospitalized diabetes mellitus type 2 patients died during the study period. Mortality was increased as age rises, patients admitted through emergency rooms, patients who were readmitted to the hospital, and patients who had metabolic or renal complications. Patients admitted for a urinary tract infection had a lower mortality rate.
Introduction
According to the International Diabetes Federation, it was estimated that 415 million people had diabetes mellitus in the world in 2015 and approximately 5 million people died from this disease [1]. In Peru, more than one million people have diabetes, geographically distributed in each natural region: coast, mountain and forest with prevalence of 8.2%, 4.5% and 3.5%, respectively. The national prevalence is about 7% (among adults over 25 years) [2]. Diabetes mellitus and its complications are among the ten leading causes of death in the world [3]. It is a chronic disease that requires continuous medical checking, which is a problem in spite of having strategies that try to reduce complications endangering the patient's life [4].
Cerebral vascular accidents and acute myocardial infarction are the main causes of mortality in patients with diabetes in countries with high economic income; while infections in lower and middle-income countries [5],[6]. A study conducted in a hospital in India found that there is a greater probability of dying in patients with diabetes when they also have vascular or renal diseases, and infections. In Peru, a study conducted in a general hospital in Lima, described cerebral vascular accident, respiratory infection and acute renal injury as factors associated with mortality in these patients [7]. We have not found reports that describe factors which increase mortality in this type of patients in regional hospitals from Peru, where the resources of the health sector are deficient, medications are limited and the glycemic controls are inadequate [8].
Therefore, the objective of this study was to determine factors associated with intra hospital mortality in patients with diabetes mellitus type 2 in three hospitals located in the southern mountain range of Peru.
Methods
Design and population
An analytical cross-sectional study was conducted, using data from 153 patients with diabetes mellitus type 2 hospitalized during 2016 in the Internal Medicine services from three hospitals in the City of Cusco, located in the southern mountain range in Peru. The hospitals were: Hospital Regional del Cusco, Antonio Lorena Hospital both dependents of the Ministry of Health and the National Hospital Adolfo Guevara Velasco under the Ministry of Labor and Promotion of the Employment of Peru. The latter belongs to the Social Security, an institution for insured workers or their relatives, who receives monetary contributions from its policy holders and has a bigger budget for different activities compared with others health institution in Cusco. The hospitals are third level regional reference hospitals, which also serve patients from other regions of the southern mountain range in Peru and from different socioeconomic conditions. The entire data found in census sampling was used.
Selection of participants
Data from medical records of all patients with diabetes mellitus type 2 (according to the American Diabetes Association) [9] hospitalized in the internal medicine service were included. The disease must have been confirmed by a doctor of internal medicine or an endocrinologist. Patients hospitalized only for performing a diagnostic or therapeutic procedure (renal biopsy, peritoneal dialysis catheter placement, pulses with corticoids, etcetera), and pregnant patients were excluded.
Variables of study
The variable of interest was status at discharge (died or alive) during the study period. To characterize the study population socio educational variables such as sex, age, marital status, education level and place of residence were considered. The hospitalization cause, defined as diagnosis at the time of admission was also considered as a variable. This was subdivided into: infectious (urinary, respiratory, subcutaneous tissue, diabetic foot), metabolic (hypoglycemia, diabetic ketoacidosis, hyperosmotic condition), cardiovascular (cerebrovascular accident and acute myocardial infarction) and renal (acute kidney failure and chronic kidney disease). Finally, we considered comorbidities, intra hospital complications, admission route to the hospital (emergency or doctor's office), length of stay and glycemic control (appropriate if glycosylated hemoglobin was <7% and inappropriate if ≥7%).
Data analysis
A database was developed for each hospital using Microsoft Excel (version for Windows 2013) which later on was revised, depurate and analyzed. To analyze the data we used the statistical program Stata v.11.1 (Stata Corp LP, College Station, TX, USA). A descriptive analysis of categorical variables was made using absolute and relative frequencies, quantitative variables were described through the median and the interquartile range according to the previous evaluation of normality with the Shapiro Wilk test.
Bivariate and multivariate analytical statistics was applied, in which “death” was used as a dependent variable. This was individually combined with each independent variable (bivariate analysis) and afterwards, with all the variables that were statistically significant in the bivariate analysis (multivariate analysis). Both, the crude and adjusted prevalence ratios were calculated with 95% confidence intervals together with the p values. We used generalized linear models, with Poisson family (we used this family because the main variable was dichotomous and allows to obtain prevalence ratios when generalized linear models are applied in analytical cross-sectional studies), log link function, sturdy models and using each hospital as a cluster. The p values <0.05 were considered significant.
Ethical aspects
The study was reviewed and approved by the ethics and research committee of the mentioned hospitals. Names were eliminated from the database after collecting the data of each patient, and an anonymous list was used for the analysis.
Results
From the 153 patients, 56.9% (87) were female, the median age was 66 years (interquartile range 54 to 78 years old). The main socio-educational results are shown in Table 1.
Table 1. Socio-educational characteristics from hospitalized patients with type 2 diabetes mellitus.
Of all patients, 55.6% (85) were overweight and 27.5% (42) were obese. One hundred thirty one, (85.6%) were admitted from the emergency service and the median length of stay was nine days (interquartile range 6 to 17 days). Seventy four (48.4%) (74) were re-admitted; 14.4% (22) had a glycosylated hemoglobin test of which 95.5% (21) had inadequate glycemic control; 33.3% (51) died during hospitalization. The main cause of hospitalization was respiratory infection (21%), followed by gastrointestinal infection and diabetic foot (14% each) (Figure 1).
Figure 1. Causes of hospitalization in hospitalized patients with type 2 diabetes mellitus.
The main comorbidities were overweight (56%), hypertension (37%) and obesity (27%) (Figure 2).
Figure 2. Comorbidities of patients hospitalized with diabetes mellitus type 2.
The main complication during hospitalization was an infection (44%), followed by metabolic complications (31%) and cardiovascular complications (27%) (Figure 3).
In the bivariate analysis, we found that factors associated with a higher mortality were: age (p=0.005), being admitted through the emergency service (p<0.001), being a patient readmitted to the hospital (p=0.031), chronic kidney disease (p<0.001) or diabetic ketoacidosis (p<0.001) as admission cause and having an infectious (p<0.001), metabolic (p=0.002), cardiovascular (p=0.025) or renal (p<0.001) complication during hospitalization. On the other hand, the highest level of instruction (p=0.004), living in a rural area (p=0.019) and being admitted for a urinary tract infection (p<0.001) were related to decreased mortality (Table 2).
According to multivariate analysis, variables associated with a higher mortality were: age (adjusted prevalence ratio 1.02, 95% confidence interval 1.01 to 1.03, p value <0.001), admission through the emergency department (adjusted prevalence ratio 1.93, 95% confidence interval 1.34 to 2.77, p value <0.001), being a patient who re-enters to the hospital (adjusted prevalence ratio 2.01, 95% confidence interval 1.36 to 2.98, p value <0.001) and having an inhospital metabolic (adjusted prevalence ratio 1.61, 95% confidence interval 1.07 to 2.43, p value = 0.024) or renal (adjusted prevalence ratio 1.47, 95% confidence interval 1.30 a 1.67, p value <0.001) complication. Conversely, mortality decreased when the cause of hospitalization was urinary tract infection (adjusted prevalence ratio 0.50, 95% confidence interval 0.35 to 0.72, p value <0.001). All these variables were adjusted by educational level, place of residence, chronic kidney disease or diabetic ketoacidosis as cause of admission. Having an inhospital infectious or cardiovascular complication and for the hospital (table 3).
Discussion
During the study we observed that mortality increased with age, possibly due to the complications which older people are prone to. This is similar to what we found in other reports [10],[11], where being over 60 years old can be an independent factor associated with complications and mortality [11]. This should be reason to create programs for older people in order to provide more medical advice, diagnosis and support to this group of patients.
Entering through an emergency department increased mortality, a fact that demonstrates the importance of complications generated by this type of admission. Diabetic patients have more risk of dying when they are admitted for urgent reasons [12] particularly if complications are acute such as hyperglycemia, which is one of the most frequent reasons for emergency admission [13] that can even cause the patient´s entrance to the intensive care unit [14],[15]. It also may provoke an extended hospital stay thus increasing healthcare costs [13]. However, in a study made in a general hospital in Lima-Peru, such an association was not found, possibly because of the heterogeneous population compared with ours [7]. We recommend to carry out more studies about reasons for admission and their repercussions in diabetic patients.
Patients who had had previous admissions had a higher mortality rate, possibly for the higher severity and chronicity of complications; this is also reported by a study in Mexico [16], which attributes the most frequent intra hospital complications to infections, hypoglycemia and cardiovascular diseases. This is similar to other Peruvian reports [17],[18].
Patients who presented an inhospital complication of metabolic type had a higher mortality. This is similar to a hospital in India, which indicates that presenting metabolic complications increases the risk of death more than infectious complications [19]. This complication has increased in Peru over the years, especially in older people, raising the mortality rate [20]. Furthermore, an inadequate metabolic control would cause the development of late complications and thus a greater number of comorbidities [17].
Likewise, those with a renal inhospital complication had a higher mortality. This is possibly due to the complications of the kidney disease [21]. Kidney disease affects 20-40% of patients with diabetes, which is also the main cause of end-stage renal disease [22]. This complication is also reported in Peruvian hospitals [7],[18], considering it an important cause of mortality in this population [7],[17]. This pathology has a strong correlation with the condition of arterial hypertension (due to the kidney´s regulation function), for this reason we avoided to include this variable in the multivariate model, but it is known that it is also very important and should be studied separately.
Finally, those who were admitted for a urinary tract infection had a lower mortality, possibly due to an adequate handling in this type of pathology and for its lower complexity. However, there are reports that mention that diabetic patients have a higher risk to acquire complicated urinary tract infections [23], being a frequent reason for admission in Peru [7],[17] and in other countries [24],[25]. We suggest conducting research that shows the most frequent type of urinary infection and its impact on hospitalized diabetic patients that, despite not causing a higher mortality, can have other repercussions on the patient.
Limitations
The study has the limitation of being based on data from medical records and having a limited population. Despite this limitation, the results are important because it is the first study made in a hospital in this region of Peru which evaluates mortality in hospitals with socioeconomically different populations.
This fact presents us a general overview of the problem and allows us to open the field of research about this subject where there are few studies, especially in countries with medium and low income, and where the nutritional status and the epidemiology transition are different. This could cause that this reality changes in the coming years.
Conclusions
According to the results we concluded that: age, emergency admission and re-admission to hospitalization were factors associated with mortality in the study population as well as presenting intra hospital complications of metabolic or renal type. However, presenting urinary tract infection as a cause of hospitalization decreased the probability of mortality.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Of the authors
The authors make available the databases to serve the scientific community, this is done in the publication as an attachment in https://doi.org/10.6084/m9.figshare.5606041.v1 .
Ethical aspects
The Journal is aware that the study was reviewed and approved by the ethics and research committees of: Hospital Regional del Cusco, Hospital Nacional Adolfo Guevara Velasco and Hospital Antonio Lorena, in addition to removing the names from the database after collecting each patient's data and using an anonymous list for analysis.
Declaration of conflicts of interest
The authors have completed the ICMJE Conflict of Interest declaration form, and declare that they have not received funding for the report; have no financial relationships with organizations that might have an interest in the published article in the last three years; and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the author responsible or the editorial management of the Journal.
Financing
The authors state that there were no external sources of funding.
Editor's note
The principal or responsible author asserts that this manuscript is an honest, accurate and transparent transcription of the study being reported; that no important aspects of the study have been omitted; and that discrepancies between the study results and those anticipated (if relevant) have been recorded and explained.

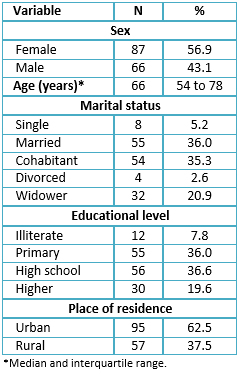 Table 1. Socio-educational characteristics from hospitalized patients with type 2 diabetes mellitus.
Table 1. Socio-educational characteristics from hospitalized patients with type 2 diabetes mellitus.

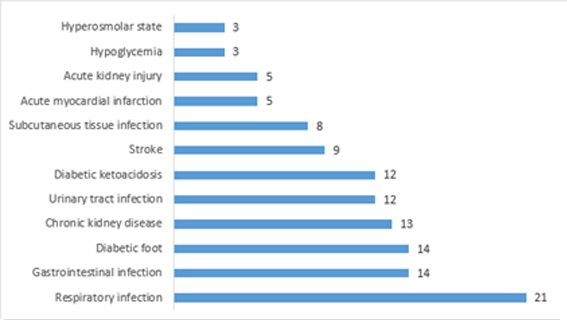 Figure 1. Causes of hospitalization in hospitalized patients with type 2 diabetes mellitus.
Figure 1. Causes of hospitalization in hospitalized patients with type 2 diabetes mellitus.

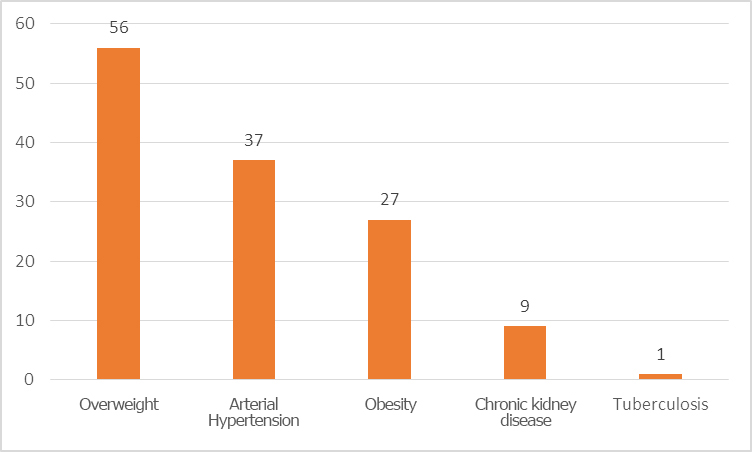 Figure 2. Comorbidities of patients hospitalized with diabetes mellitus type 2.
Figure 2. Comorbidities of patients hospitalized with diabetes mellitus type 2.

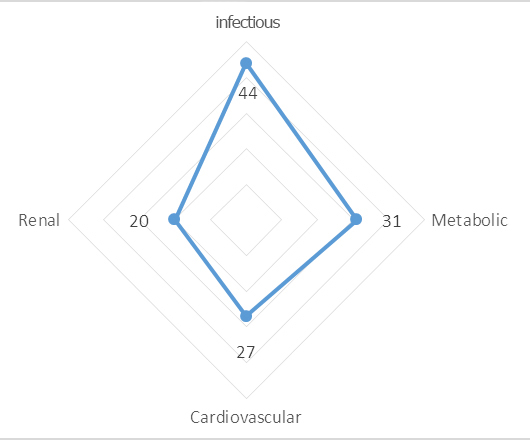 Figure 3. Complications during hospitalization of patients with diabetes mellitus type 2 in Cusco-Peru.
Figure 3. Complications during hospitalization of patients with diabetes mellitus type 2 in Cusco-Peru.

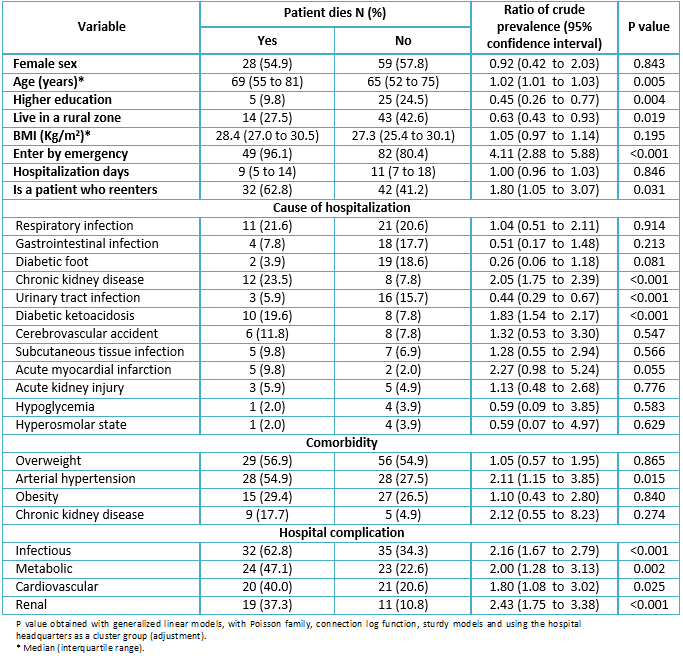 Table 2. Bivariate analysis of the associated factors with in-hospital mortality in patients with type 2 diabetes mellitus.
Table 2. Bivariate analysis of the associated factors with in-hospital mortality in patients with type 2 diabetes mellitus.

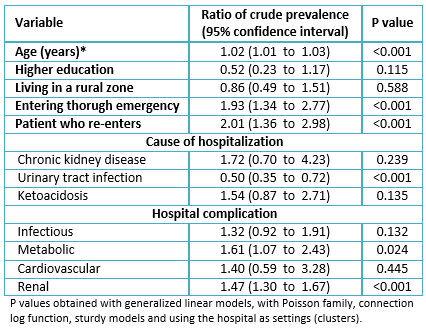 Table 3. Multivariate analysis of the associated factors with in-hospital mortality in patients with diabetes mellitus type 2 in Cusco-Peru.
Table 3. Multivariate analysis of the associated factors with in-hospital mortality in patients with diabetes mellitus type 2 in Cusco-Peru.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
La mortalidad por diabetes se ha incrementado en los últimos años. En Perú, existen escasos estudios acerca de la mortalidad intrahospitalaria por diabetes en provincias.
OBJETIVOS
Determinar los factores asociados a mortalidad intrahospitalaria en pacientes con diabetes mellitus tipo 2 en tres hospitales de la sierra sur del Perú.
MÉTODOS
Se realizó un estudio de corte transversal analítico. Se incluyó a todos los pacientes con diabetes mellitus tipo 2 hospitalizados en la ciudad del Cusco durante el año 2016. Se evaluó las características socioeducativas y clínicas, teniendo a la “defunción” como variable de interés. Se calculó las razones de prevalencias crudas y ajustadas, mediante los modelos lineales generalizados, con familia Poisson y función de enlace log, con sus respectivos intervalos de confianza al 95%. Se consideró significativos los valores p < 0,05.
RESULTADOS
De los 153 pacientes, el 33,3% (51) murió en la hospitalización. Incrementó la frecuencia de mortalidad: por cada año de edad del paciente (razón de prevalencias ajustada 1,02; intervalo de confianza 95%: 1,01 a 1,03; valor p < 0,001), por haber ingresado por el servicio de emergencia (razón de prevalencias ajustada 1,93; intervalo de confianza 95%: 1,34 a 2,77; valor p < 0,001), por ser un paciente que reingresa al hospital (razón de prevalencias ajustada 2,01; intervalo de confianza 95%: 1,36 a 2,98; valor p < 0,001) y por haber tenido una complicación hospitalaria metabólica (razón de prevalencias ajustada 1,61; intervalo de confianza 95%: 1,07 a 2,43; valor p = 0,024) o renal (razón de prevalencias ajustada 1,47; intervalo de confianza 95%: 1,30 a 1,67; valor p < 0,001). En cambio, disminuyó la frecuencia mortalidad el que su causa de hospitalización haya sido por una infección del tracto urinario (razón de prevalencia ajustada 0,50; intervalo de confianza 95%: 0,35 a 0,72; valor p < 0,001); ajustado por siete variables.
CONCLUSIONES
La edad, el ingresar por emergencia y el presentar reingresos a la hospitalización fueron factores asociados a mortalidad; así como el presentar complicaciones intrahospitalarias de tipo metabólica o renal.
 Authors:
Noé Atamari-Anahui[1], Franklin W. Martinez-Ninanqui[1], Liz Paucar-Tito[1,2], Luz Morales-Concha[1,2], Alejandra Miranda-Chirau[1,2], Marco Antonio Gamarra-Contreras[1,3], Carlos Antonio Zea-Nuñez[1,4], Christian R. Mejia[5,6]
Authors:
Noé Atamari-Anahui[1], Franklin W. Martinez-Ninanqui[1], Liz Paucar-Tito[1,2], Luz Morales-Concha[1,2], Alejandra Miranda-Chirau[1,2], Marco Antonio Gamarra-Contreras[1,3], Carlos Antonio Zea-Nuñez[1,4], Christian R. Mejia[5,6]
Affiliation:
[1] Escuela de Medicina, Universidad Nacional de San Antonio Abad del Cusco, Cusco, Perú
[2] Asociación científica de estudiantes de medicina (ASOCIEMH-CUSCO), Cusco, Perú
[3] Departamento de Endocrinología, Hospital Regional del Cusco, Cusco, Perú
[4] Departamento de Endocrinología, Hospital Nacional Adolfo Guevara Velasco – EsSalud, Cusco, Perú
[5] Escuela de Medicina Humana, Universidad Continental, Huancayo, Perú
[6] Asociación Médica de Investigación y Servicios en Salud, Lima, Perú
E-mail: noe.atamari@gmail.com
Author address:
[1] Calle Los Geranios B-2
San Sebastián
Cusco
Perú

Citation: Atamari-Anahui N, Martinez-Ninanqui FW, Paucar-Tito L, Morales-Concha L, Miranda-Chirau A, Gamarra-Contreras MA, et al. Factors associated to inpatient mortality rates in type-2-diabetic patients: a cross-sectional analytical study in three Peruvian hospitals. Medwave 2017 Nov-Dic;17(9):e7097 doi: 10.5867/medwave.2017.09.7097
Publication date: 5/12/2017
Origin: not requested
Type of review: reviewed by five external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- International Diabetes Federation. Atlas de la diabetes de la FID. 7ma ed. 2015; 51. | Link |
- Seclen SN, Rosas ME, Arias AJ, Huayta E, Medina CA. Prevalence of diabetes and impaired fasting glucose in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Res Care. 2015 Oct 19;3(1):e000110. | CrossRef | PubMed |
- World Health Organization. Las 10 principales causas de defunción. WHO. | Link |
- American Diabetes Association. Standard of Medical Care in Diabetes-2017. Diabetes Care. 2017;40(Supplement 1). | Link |
- Moss SE, Klein R, Klein BE. Cause-specific mortality in a population-based study of diabetes. Am J Public Health. 1991;81(9):1158-62. | PubMed |
- Vasan SK, Pittard AE, Abraham J, Samuel P, Seshadri MS, Thomas N. Cause-specific mortality in diabetes: retrospective hospital based data from south India. J Diabetes. 2012 Mar;4(1):47-54. | CrossRef | PubMed |
- Zelada H, Bernabe-Ortiz A, Manrique H. Inhospital Mortality in Patients with Type 2 Diabetes Mellitus: A Prospective Cohort Study in Lima, Peru.J Diabetes Res. 2016;2016:7287215. | CrossRef | PubMed |
- Taype-Rondan A, Lazo-Porras M, Moscoso-Porras M, Moreano-Sáenz M, Miranda JJ. Inadequate glycaemic control in LMIC: health system failures in Peru. Br J Gen Pract. 2016 Apr;66(645):197. | CrossRef | PubMed |
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2017;40 (Supplement 1):S11-24. | CrossRef |
- Al-Rubeaan K, Youssef AM, Ibrahim HM, Al-Sharqawi AH, AlQumaidi H, AlNaqeb D, et al. All-cause mortality and its risk factors among type 1 and type 2 diabetes mellitus in a country facing diabetes epidemic. Diabetes Res Clin Pract. 2016 Aug;118:130-9. | CrossRef | PubMed |
- Chew BH, Ghazali SS, Ismail M, Haniff J, Bujang MA. Age ≥ 60 years was an independent risk factor for diabetes-related complications despite good control of cardiovascular risk factors in patients with type 2 diabetes mellitus. Exp Gerontol. 2013 May;48(5):485-91. | CrossRef | PubMed |
- Holman N, Hillson R, Young RJ. Excess mortality during hospital stays among patients with recorded diabetes compared with those without diabetes. Diabet Med. 2013 Dec;30(12):1393-402. | CrossRef | PubMed |
- Álvarez-Rodríguez E, Laguna Morales I, Rosende Tuya A, Tapia Santamaría R, Martín Martínez A, López Riquelme P, et al. Frequency and management of diabetes and hyperglycemia at emergency departments: the GLUCE-URG Study. Endocrinol Diabetes Nutr. 2017 Feb;64(2):67-74. | CrossRef | PubMed |
- Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009 Jul;32(7):1335-43. | CrossRef | PubMed |
- Zelihic E, Poneleit B, Siegmund T, Haller B, Sayk F, Dodt C. Hyperglycemia in emergency patients--prevalence and consequences: results of the GLUCEMERGE analysis. Eur J Emerg Med. 2015 Jun;22(3):181-7. | CrossRef | PubMed |
- Membreño-Mann JP, Zonana-Nacach A. Hospitalización de pacientes con diabetes mellitus. Causas, complicaciones y mortalidad. Rev Médica Inst Mex Seguro Soc. 2005;43(2):97-101. | Link |
- Gonzales-Grández N, Rodríguez-Lay E, Manrique-Hurtado H. Características clínicas y factores asociados a morbilidad intrahospitalaria en los pacientes con diabetes mellitus tipo 2. Rev Soc Peru Med Interna. 2013;26(4):159-65. | Link |
- Zegarra T, Guillermo G, Cáceres C, Luis J, Zegarra T, Miriam L. Características sociodemográficas y clínicas de los pacientes diabéticos tipo 2 con infecciones adquiridas en la comunidad admitidos en los servicios de Medicina del Hospital Nacional Cayetano Heredia. Rev Medica Hered. 2000;11(3):89-96. | Link |
- Zargar AH, Wani AI, Masoodi SR, Bashir MI, Laway BA, Gupta VK, et al. Causes of mortality in diabetes mellitus: data from a tertiary teaching hospital in India. Postgrad Med J. 2009 May;85(1003):227-32. | CrossRef | PubMed |
- Ticse R, Alán-Peinado A, Baiocchi-Castro L. Características demográficas y epidemiológicas de pacientes con diabetes mellitus tipo 2 hospitalizados por cetoacidosis diabética en un hospital general de Lima-Perú. Rev Medica Hered. 2014;25(1):5. | Link |
- Gimeno-Orna JA, Blasco-Lamarca Y, Campos-Gutierrez B, Molinero-Herguedas E, Lou-Arnal LM, García-García B. Risk of mortality associated to chronic kidney disease in patients with type 2 diabetes mellitus: A 13-year follow-up. Nefrol Engl Ed. 2015;35(5):487-92. | Link |
- Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Am J Kidney Dis. 2014 Oct;64(4):510-33. | CrossRef | PubMed |
- Nitzan O, Elias M, Chazan B, Saliba W. Urinary tract infections in patients with type 2 diabetes mellitus: review of prevalence, diagnosis, and management. Diabetes Metab Syndr Obes. 2015 Feb 26;8:129-36. | CrossRef | PubMed |
- Osuna M, Rivera MC, Bocanegra C de J, Lancheros A, Tovar H, Hernández JI, et al. Caracterización de la diabetes mellitus tipo 2 y el control metabólico en el paciente hospitalizado. Acta Medica Colomb. 2014;39(4):344-51. | Link |
- Solís-Sanchez C, Villamar-Triviño R. Hospitalizaciones en pacientes con diabetes mellitus tipo 2: características clínicas. Rev ALAD. 2014;4(2):43-8. | Link |
 Seclen SN, Rosas ME, Arias AJ, Huayta E, Medina CA. Prevalence of diabetes and impaired fasting glucose in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Res Care. 2015 Oct 19;3(1):e000110. | CrossRef | PubMed |
Seclen SN, Rosas ME, Arias AJ, Huayta E, Medina CA. Prevalence of diabetes and impaired fasting glucose in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Res Care. 2015 Oct 19;3(1):e000110. | CrossRef | PubMed | American Diabetes Association. Standard of Medical Care in Diabetes-2017. Diabetes Care. 2017;40(Supplement 1). | Link |
American Diabetes Association. Standard of Medical Care in Diabetes-2017. Diabetes Care. 2017;40(Supplement 1). | Link | Moss SE, Klein R, Klein BE. Cause-specific mortality in a population-based study of diabetes. Am J Public Health. 1991;81(9):1158-62. | PubMed |
Moss SE, Klein R, Klein BE. Cause-specific mortality in a population-based study of diabetes. Am J Public Health. 1991;81(9):1158-62. | PubMed | Vasan SK, Pittard AE, Abraham J, Samuel P, Seshadri MS, Thomas N. Cause-specific mortality in diabetes: retrospective hospital based data from south India. J Diabetes. 2012 Mar;4(1):47-54. | CrossRef | PubMed |
Vasan SK, Pittard AE, Abraham J, Samuel P, Seshadri MS, Thomas N. Cause-specific mortality in diabetes: retrospective hospital based data from south India. J Diabetes. 2012 Mar;4(1):47-54. | CrossRef | PubMed | Zelada H, Bernabe-Ortiz A, Manrique H. Inhospital Mortality in Patients with Type 2 Diabetes Mellitus: A Prospective Cohort Study in Lima, Peru.J Diabetes Res. 2016;2016:7287215. | CrossRef | PubMed |
Zelada H, Bernabe-Ortiz A, Manrique H. Inhospital Mortality in Patients with Type 2 Diabetes Mellitus: A Prospective Cohort Study in Lima, Peru.J Diabetes Res. 2016;2016:7287215. | CrossRef | PubMed | Taype-Rondan A, Lazo-Porras M, Moscoso-Porras M, Moreano-Sáenz M, Miranda JJ. Inadequate glycaemic control in LMIC: health system failures in Peru. Br J Gen Pract. 2016 Apr;66(645):197. | CrossRef | PubMed |
Taype-Rondan A, Lazo-Porras M, Moscoso-Porras M, Moreano-Sáenz M, Miranda JJ. Inadequate glycaemic control in LMIC: health system failures in Peru. Br J Gen Pract. 2016 Apr;66(645):197. | CrossRef | PubMed | American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2017;40 (Supplement 1):S11-24. | CrossRef |
American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2017;40 (Supplement 1):S11-24. | CrossRef | Al-Rubeaan K, Youssef AM, Ibrahim HM, Al-Sharqawi AH, AlQumaidi H, AlNaqeb D, et al. All-cause mortality and its risk factors among type 1 and type 2 diabetes mellitus in a country facing diabetes epidemic. Diabetes Res Clin Pract. 2016 Aug;118:130-9. | CrossRef | PubMed |
Al-Rubeaan K, Youssef AM, Ibrahim HM, Al-Sharqawi AH, AlQumaidi H, AlNaqeb D, et al. All-cause mortality and its risk factors among type 1 and type 2 diabetes mellitus in a country facing diabetes epidemic. Diabetes Res Clin Pract. 2016 Aug;118:130-9. | CrossRef | PubMed | Chew BH, Ghazali SS, Ismail M, Haniff J, Bujang MA. Age ≥ 60 years was an independent risk factor for diabetes-related complications despite good control of cardiovascular risk factors in patients with type 2 diabetes mellitus. Exp Gerontol. 2013 May;48(5):485-91. | CrossRef | PubMed |
Chew BH, Ghazali SS, Ismail M, Haniff J, Bujang MA. Age ≥ 60 years was an independent risk factor for diabetes-related complications despite good control of cardiovascular risk factors in patients with type 2 diabetes mellitus. Exp Gerontol. 2013 May;48(5):485-91. | CrossRef | PubMed | Holman N, Hillson R, Young RJ. Excess mortality during hospital stays among patients with recorded diabetes compared with those without diabetes. Diabet Med. 2013 Dec;30(12):1393-402. | CrossRef | PubMed |
Holman N, Hillson R, Young RJ. Excess mortality during hospital stays among patients with recorded diabetes compared with those without diabetes. Diabet Med. 2013 Dec;30(12):1393-402. | CrossRef | PubMed | Álvarez-Rodríguez E, Laguna Morales I, Rosende Tuya A, Tapia Santamaría R, Martín Martínez A, López Riquelme P, et al. Frequency and management of diabetes and hyperglycemia at emergency departments: the GLUCE-URG Study. Endocrinol Diabetes Nutr. 2017 Feb;64(2):67-74. | CrossRef | PubMed |
Álvarez-Rodríguez E, Laguna Morales I, Rosende Tuya A, Tapia Santamaría R, Martín Martínez A, López Riquelme P, et al. Frequency and management of diabetes and hyperglycemia at emergency departments: the GLUCE-URG Study. Endocrinol Diabetes Nutr. 2017 Feb;64(2):67-74. | CrossRef | PubMed | Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009 Jul;32(7):1335-43. | CrossRef | PubMed |
Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009 Jul;32(7):1335-43. | CrossRef | PubMed | Zelihic E, Poneleit B, Siegmund T, Haller B, Sayk F, Dodt C. Hyperglycemia in emergency patients--prevalence and consequences: results of the GLUCEMERGE analysis. Eur J Emerg Med. 2015 Jun;22(3):181-7. | CrossRef | PubMed |
Zelihic E, Poneleit B, Siegmund T, Haller B, Sayk F, Dodt C. Hyperglycemia in emergency patients--prevalence and consequences: results of the GLUCEMERGE analysis. Eur J Emerg Med. 2015 Jun;22(3):181-7. | CrossRef | PubMed | Membreño-Mann JP, Zonana-Nacach A. Hospitalización de pacientes con diabetes mellitus. Causas, complicaciones y mortalidad. Rev Médica Inst Mex Seguro Soc. 2005;43(2):97-101. | Link |
Membreño-Mann JP, Zonana-Nacach A. Hospitalización de pacientes con diabetes mellitus. Causas, complicaciones y mortalidad. Rev Médica Inst Mex Seguro Soc. 2005;43(2):97-101. | Link | Gonzales-Grández N, Rodríguez-Lay E, Manrique-Hurtado H. Características clínicas y factores asociados a morbilidad intrahospitalaria en los pacientes con diabetes mellitus tipo 2. Rev Soc Peru Med Interna. 2013;26(4):159-65. | Link |
Gonzales-Grández N, Rodríguez-Lay E, Manrique-Hurtado H. Características clínicas y factores asociados a morbilidad intrahospitalaria en los pacientes con diabetes mellitus tipo 2. Rev Soc Peru Med Interna. 2013;26(4):159-65. | Link | Zegarra T, Guillermo G, Cáceres C, Luis J, Zegarra T, Miriam L. Características sociodemográficas y clínicas de los pacientes diabéticos tipo 2 con infecciones adquiridas en la comunidad admitidos en los servicios de Medicina del Hospital Nacional Cayetano Heredia. Rev Medica Hered. 2000;11(3):89-96. | Link |
Zegarra T, Guillermo G, Cáceres C, Luis J, Zegarra T, Miriam L. Características sociodemográficas y clínicas de los pacientes diabéticos tipo 2 con infecciones adquiridas en la comunidad admitidos en los servicios de Medicina del Hospital Nacional Cayetano Heredia. Rev Medica Hered. 2000;11(3):89-96. | Link | Zargar AH, Wani AI, Masoodi SR, Bashir MI, Laway BA, Gupta VK, et al. Causes of mortality in diabetes mellitus: data from a tertiary teaching hospital in India. Postgrad Med J. 2009 May;85(1003):227-32. | CrossRef | PubMed |
Zargar AH, Wani AI, Masoodi SR, Bashir MI, Laway BA, Gupta VK, et al. Causes of mortality in diabetes mellitus: data from a tertiary teaching hospital in India. Postgrad Med J. 2009 May;85(1003):227-32. | CrossRef | PubMed | Ticse R, Alán-Peinado A, Baiocchi-Castro L. Características demográficas y epidemiológicas de pacientes con diabetes mellitus tipo 2 hospitalizados por cetoacidosis diabética en un hospital general de Lima-Perú. Rev Medica Hered. 2014;25(1):5. | Link |
Ticse R, Alán-Peinado A, Baiocchi-Castro L. Características demográficas y epidemiológicas de pacientes con diabetes mellitus tipo 2 hospitalizados por cetoacidosis diabética en un hospital general de Lima-Perú. Rev Medica Hered. 2014;25(1):5. | Link | Gimeno-Orna JA, Blasco-Lamarca Y, Campos-Gutierrez B, Molinero-Herguedas E, Lou-Arnal LM, García-García B. Risk of mortality associated to chronic kidney disease in patients with type 2 diabetes mellitus: A 13-year follow-up. Nefrol Engl Ed. 2015;35(5):487-92. | Link |
Gimeno-Orna JA, Blasco-Lamarca Y, Campos-Gutierrez B, Molinero-Herguedas E, Lou-Arnal LM, García-García B. Risk of mortality associated to chronic kidney disease in patients with type 2 diabetes mellitus: A 13-year follow-up. Nefrol Engl Ed. 2015;35(5):487-92. | Link | Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Am J Kidney Dis. 2014 Oct;64(4):510-33. | CrossRef | PubMed |
Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Am J Kidney Dis. 2014 Oct;64(4):510-33. | CrossRef | PubMed | Nitzan O, Elias M, Chazan B, Saliba W. Urinary tract infections in patients with type 2 diabetes mellitus: review of prevalence, diagnosis, and management. Diabetes Metab Syndr Obes. 2015 Feb 26;8:129-36. | CrossRef | PubMed |
Nitzan O, Elias M, Chazan B, Saliba W. Urinary tract infections in patients with type 2 diabetes mellitus: review of prevalence, diagnosis, and management. Diabetes Metab Syndr Obes. 2015 Feb 26;8:129-36. | CrossRef | PubMed | Osuna M, Rivera MC, Bocanegra C de J, Lancheros A, Tovar H, Hernández JI, et al. Caracterización de la diabetes mellitus tipo 2 y el control metabólico en el paciente hospitalizado. Acta Medica Colomb. 2014;39(4):344-51. | Link |
Osuna M, Rivera MC, Bocanegra C de J, Lancheros A, Tovar H, Hernández JI, et al. Caracterización de la diabetes mellitus tipo 2 y el control metabólico en el paciente hospitalizado. Acta Medica Colomb. 2014;39(4):344-51. | Link | Solís-Sanchez C, Villamar-Triviño R. Hospitalizaciones en pacientes con diabetes mellitus tipo 2: características clínicas. Rev ALAD. 2014;4(2):43-8. | Link |
Solís-Sanchez C, Villamar-Triviño R. Hospitalizaciones en pacientes con diabetes mellitus tipo 2: características clínicas. Rev ALAD. 2014;4(2):43-8. | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








