Key Words: acute coronary syndrome, secondary prevention, evidence-based medicine, guideline adherence
Abstract
INTRODUCTION
Cardiovascular disease is the leading cause of mortality worldwide. When an acute myocardial infarction occurs, it is necessary to establish secondary prevention measures, which can reduce mortality by 50%. Clinical guidelines state that the optimal medical treatment is based upon four groups of drugs: antiplatelet drugs, statins, beta-blockers and angiotensin-converting-enzyme inhibitor or angiotensin II receptor antagonist.
OBJECTIVE
To determine physician compliance to evidence-based clinical practice guidelines on secondary prevention of coronary heart disease.
METHODS
Retrospective, observational study in Hospital Cayetano Heredia in Lima, Peru. The study included patients with confirmed acute coronary syndrome from February 2011 to February 2013. Medical records, laboratory results and medical therapy at discharge were collected and were compared to the American Heart Association type I, evidence level A recommendations. In addition, patient follow-up visits to the outpatient cardiology clinic at 1, 3 and 6 months after discharge were analyzed.
RESULTS
The study population included 143 patients. Eighty-nine (89) patients were admitted with the diagnosis of unstable angina and non-ST-segment elevation (62.2%) and 54 had ST-segment elevation myocardial infarction (37.8%). Forty patients (28%) received all four recommended medications at discharge, which decreased at 1, 3 and 6 months after discharge to 12.6%, 7% and 3.5% respectively. The results showed a significant reduction in patient compliance to follow-up visits with a 48% reduction at the first visit to 10% on the last visit.
CONCLUSION
Medical compliance to guidelines recommendations in secondary cardiovascular prevention is suboptimal with a compliance score under 50%.
Introduction
Cardiovascular disease constitutes the major cause of incapacity and death worldwide, with acute myocardial infarction being the most frequent clinical manifestation [1]. Cardiovascular risk factors initiate the atherosclerotic process which may lead to asymptomatic clinical manifestations that progressively evolve to the final stages of the disease [2]. Once complications such as acute myocardial infarction are present, measures directed at reducing the risk of recurrence and mortality must be initiated, which constitutes the objective of secondary prevention. It is estimated that these therapeutic measures may reduce mortality by 50% [3].
In 2011, the American Heart Association published the “AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and Other Atherosclerotic Vascular Disease: 2011 Update”, which gathers the principal recommendations about lifestyle changes, control of cardiovascular risk factors and the prescription of specific drugs with Class I Recommendation and Level of Evidence A due to their benefit in secondary prevention [4]. These drugs include: antiplatelet agents, statins, beta-blockers, and renin-angiotensin-aldosterone system modulators (angiotensin-converting-enzyme inhibitors or angiotensin II receptor antagonists) [4]. These four pharmacological groups constitute the optimal medical treatment which, despite having shown to significantly reduce recurrence and mortality [5],[6],[7],[8] are employed much less than expected. There are studies in Brazil, Korea and Australia reporting medical compliance to these recommendations between 50 and 70% [9],[10],[11].
Diverse studies recognize that physician’s knowledge and compliance with clinical practice guidelines is suboptimal [12]. Despite the healthcare system and the patient being generally held as responsible, the physician’s role is also determinant in the compliance with therapeutic practices established by clinical guidelines. The objectives of this study were to determine the adherence of physician’s prescriptions to the “AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and Other Atherosclerotic Vascular Disease” as indicated at discharge from hospitalization and in outpatient follow-up of patients diagnosed with coronary disease; and to evaluate if the adherence of the prescription’s varied with the type of myocardial infarction, age, comorbidities (such as diabetes and hypertension) and pharmacological group.
Methods
Study design
Observational, retrospective cohort study. The clinical histories of patients who were hospitalized and followed in outpatient visits due to established coronary disease at Hospital Cayetano Heredia in Lima, Peru were reviewed during the period comprised between February 1st, 2011 and February 28th, 2013.
Population
For the identification of cases, the registry of patients hospitalized and evaluated by the Cardiology Service with the initial diagnosis of Acute Coronary Syndrome was reviewed to verify compliance with one of the established definitions in the “Third Universal Definition of Myocardial Infarction” [13],[14]. Clinical histories of patients with definitive diagnosis of ST-elevation acute myocardial infarction, non-ST-elevation acute myocardial infarction or unstable angina were consigned. Patients were catalogued with acute myocardial infarction if they met two of the following criteria: clinical, biochemical (troponin elevation) and electrocardiographic (ST segment alteration, T wave and/or new left bundle branch block), as established by the AHA Clinical Practice Guidelines [15].
Procedure
After verifying the inclusion criteria, data concerning to clinical and demographical characteristics (age, gender, blood pressure at discharge and cardiovascular risk factors such as hypertension, diabetes mellitus, obesity and smoking) were registered. Pharmacological prescriptions indicated at discharge by the hospitalization team were registered from the non-electronic health record. Pharmacological prescriptions indicated by the cardiology team during outpatient follow-up visits at the first, third and sixth month after discharge, were likewise registered. In regard to pharmacological treatment for secondary prevention, the standard considered was the recommendations in the American Heart Association’s clinical practice guidelines with recommendations type I, level of evidence A. Data from the clinical histories was blindly extracted by two investigators and the data was then verified with a cardiologist for the final registry.
Study variables
The primary study variable was the “adherence to guidelines” defined as the compliance with recommendations or protocols considered as official, recognized or elaborated by the institution [16]. In our study, this was evaluated by the percentage of discharge indications that complied with the recommendations of the “AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and Other Atherosclerotic Vascular Disease”, which contains the recommendations with level of evidence IA pertaining to the use of antiplatelet agents, statins, beta-blockers and renin-angiotensin-aldosterone system modulators (angiotensin-converting-enzyme inhibitors or angiotensin II receptor antagonists).
In order to evaluate if some clinical or demographical characteristics of the study population werer related to the adherence to medical prescriptions, data was recollected on gender, age, diagnosis (ST-elevation myocardial infarction, non-ST-elevation myocardial infarction, unstable angina) and cardiovascular risk factors such as, hypertension, type 2 diabetes mellitus, smoking, dyslipidemia and obesity.
Statistical analysis
The data was analyzed with the statistical package STATA version 13. Descriptive statistics were calculated as proportions and 95% confidence intervals, means and standard deviations for quantitative data. For categorical variables, the percentage of agreement between the pharmacological prescription for coronary disease and the AHA’s 2011 Clinical Guidelines recommendations. For the comparison of proportions, the exact Chi2 test was employed. Continuous variables were compared with Student’s t Test and the Wilcoxon’s sum of ranges test depending on their type of distribution. A p value ≤ 0.05 was considered for statistical significance.
Ethical considerations
This study was approved by the Ethics Committee of both, Hospital Cayetano Heredia and Universidad Peruana Cayetano Heredia; from Lima, Peru.
Results
A total of 206 patients with acute coronary syndrome were identified according to the clinical histories registry kept by the Cardiology Service, out of which 23 histories did not fulfill the diagnostic criteria, 25 were not found in the archive and 10 did not match the patient’s name in the registry. One hundred and forty-three histories remained that did comply with the inclusion criteria. Sixty nine patients had records for the first follow-up visit, 33 patients for the 3rd -month visit and 15 patients for the 6th -month visit.
Patient characteristics
The demographical and clinical characteristics of the patients are described in Table 1.
Pharmacological treatment prescribed at discharge and at follow-up
The four therapeutic strategies selected for secondary prevention by the reference guideline were only indicated in 40 (28%, 95% CI: 20.8-36.1%) patients at discharge, and only in 12.6% (95% CI: 7.1-18.4%), 7% (95% CI: 3.4-12.5%) and 3.5% (95% CI: 1.1-8%) at the first, second and third follow-up outpatient visits, respectively. The proportion of patients who received the Class I Evidence Level A recommendations stipulated in the AHA’s clinical practice guidelines were as follows: antiplatelet agents (as monotherapy or combined) were the most prescribed, in 125 (87.4%, 95% CI: 80-92.5%) patients. Statins were prescribed in 109 (76.2%, 95% CI: 67-83.7%), renin-angiotensin system modulators were prescribed in 82 (57.5%, 95% CI: 45.9-68.1%). Beta-blockers were prescribed in 72 (50%, 95% CI: 37.9-62%) (Table 2).
The patients with ST-elevation myocardial infarction had a higher percentage of complete therapeutic prescription at discharge in comparison with non-ST-elevation myocardial infarction (46.3% vs 21.4%, p = 0.002). No statistically significant differences were found between the groups classified by hypertension and diabetes regarding the percentage of complete prescriptions at discharge. The patients who received antiplatelet agents and statins were younger than those who did not receive this indication (for antiplatelet agents: 63.1 ± 12.7 vs 68.5 ± 14.1 years, p = 0.02; for statins: 63.9 ± 13.1 vs 68.4 ± 13.7 years, p = 0.02). Association for other pharmacologic drugs was not significant.
Pharmacological treatment prescribed only in follow-up
An important reduction in the patients’ adherence to outpatient follow-up visits with the Cardiology Service was observed from the first to the sixth month after discharge, from 48% (IC 9%: 39.8-56.8%) at the first visit down to 10% (95% CI: 5.9-16.7%) at the last visit (Figure 1). Aspirin and statins were the drugs most prescribed while renin-angiotensin system modulators and beta-blockers were the least prescribed at all follow-up visits (Table 3).
Discussion
The adherence of medical prescriptions to the recommendations of the American Heart Association’s clinical practice guidelines at discharge in our study was 28%, one of the lowest reported in the literature. Similar studies have been carried out in various countries which show an adherence greater than 50%. One study carried out in New Zealand and Australia reported an adherence of 71% both in patients with a diagnosis of ST-elevation myocardial infarction and non-ST-elevation myocardial infarction; other associated factors identified were having had a cardiac catheterization during hospital admission, having had a catheterization or surgical myocardial revascularization prior to hospitalization and a past medical history of hypertension [11]. On the other hand, in Korea a study (n = 9294) found that 50.4% of patients were discharged with a prescription including the four pharmacological groups previously mentioned while the patients who had been submitted to catheterization had the highest rate of prescription and those who had been submitted to surgical myocardial revascularization, the lowest [9]. In Latin America, a study in Brazil (n = 1150) found that the proportion of patients who received the four pharmacological groups was close to 60% [10]. Thus, we can observe that compliance with the recommendations was lower in our study. This is a relevant finding for public health as measures can be taken to improve this parameter since it is known that these actions reduce mortality and the number of hospitalizations in patients with established coronary disease [3],[4].
Regarding the drugs indicated, antiplatelet agents constitute the principal pharmacological group prescribed upon discharge from hospitalization (87% of patients) with the greater percentage corresponding to double therapy (66%). These findings agree with some described in the Southeast of Asia and Malaysia where double therapy was indicated in 70% and 81.5% of patients, respectively [17],[18]. Regardless, differences about the administration of aspirin as monotherapy have been observed. In Spain, prescription of aspirin alone reaches 74% [6] and in Brazil 92% [10], showing that aspirin monotherapy is still greater that double therapy in other regions. It may be postulated that double therapy is still not prescribed in a routinely due to some physicians not taking into consideration the evidence presented in the last years or not having had access to this information [19]. On the other hand, there is still a percentage of patients that do not receive even one antiplatelet drug.
The prescription of statins in our study reaches 76%, in spite of the conclusive evidence in regard to their importance in high risk patients [16],[20], similarly to other studies [18],[21]. Beta-blockers were prescribed in 50.3% of patients upon discharge, while in Brazil and Korea the percentage of patients who receive this indication was greater [9],[10]. Our study did not register data regarding the presence of medical conditions that may contraindicate the use of these drugs, such as bradycardia, systolic hypotension, asthma or allergic reaction to this drug [22]. Angiotensin converting enzyme inhibitors and Angiotensin II receptor blockers were indicated in 57.3% of patients; a lower level than in other countries such as Brazil and Australia [10],[23]. The indication of these classes of drugs is based on the benefit for patients with diminished ventricular function, parameter which could not be evaluated in our study [16],[20].
The poor adherence of patients to outpatient follow-up visits with the Cardiology Service is notorious, with 48% of patients at the first visit and only 10% at the 6-month visit. This may be impacted by an inadequate communication between the patient and the hospitalization team at the time of discharge [24] or patients having sought an outpatient consult with other specialists such as Internists due to not having had an opportune appointment with the Cardiologist. Some studies have evaluated programs to improve adherence after discharge such as systems with text messaging or electronic reminders and a greater diffusion of investigation occurring inside the hospital [25],[26],[27]. Some of these programs may be applied in our setting. It is necessary to keep in mind that this study was carried out in an area where the majority of the population belongs to a low socioeconomic status which may have an influence on the patients’ access to health education.
Diverse factors have been identified in the literature that may have an influence on the low adherence physicians have towards clinical practice guidelines. In the first place, some studies report a lack of knowledge or familiarity with the guidelines, it could be due the quantity of information, the time one must invest in being informed or the guideline’s accessibility. Other factors must be considered, such as not agreeing with the clinical guidelines due to not considering them applicable to their patients due to cost-benefit considerations or lack of trust in the authors of the guidelines [21]. This is surprising since the hospital where this study was carried out is university affiliated which would lead one to expect a higher compliance with guidelines. Likewise, there are external factors, such as a patient’s lack of tolerance for the medication and lack of coverage of the medications by the public health insurance [21],[28].
Other factors that must be considered are the limitations of this study, including its retrospective design which does not permit determining causality in the relationship established between the variables. Another limitation is the fact that variables such as ejection fraction and clinical contraindications to specific drugs, which may have altered the number of patients who could receive a certain drug, were not included in the study registry. Likewise, 12% of patients’ clinical histories were lost which did not allow consideration of the entire sample. Lastly, the study was performed at a National Hospital in Lima, Peru which limits its external validity and the value of generalizing its findings to other realities, which is why it would be ideal to perform similar studies in other regions.
Regarding this study’s strengths, it is the first one to consider the physician’s adherence to prescription guidelines for established coronary disease in our region. Also, it constitutes an important aspect that will contribute to improvements in the follow-up of patients with coronary disease so as to diminish their risks.
Conclusions
There is a low physician compliance to clinical guidelines; 28% at discharge and 12% at first outpatient follow-up, according to our study carried out in a hospital in Lima, Peru. Secondly, antiplatelet agents (as monotherapy or combined therapy) were the most commonly prescribed pharmacological group. Thirdly, there was a 51.7% reduction in patient adherence to outpatient follow-up visits at the first visit. Since there are consequences in morbidity and mortality to the low adherence to clinical practice guidelines, studies are needed to evaluate the barriers preventing an adequate prescription and interventions that may improve physicians’ adherence to these guidelines’ recommendations.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The Journal is aware that the ethics committee of the Cayetano Heredia Hospital and the ethics committee of the Peruvian University Cayetano Heredia of Lima, Peru, was aware of this study and its possible publication in a biomedical dissemination journal.
Declaration of conflicts of interest
The authors have completed the ICMJE declaration of conflicts of interest form, and declare that they have not received funding for the report; Not having financial relationships with organizations that may have interests in the published article in the past three years; And not having other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.
Financing
The authors state that there were no external sources of funding.

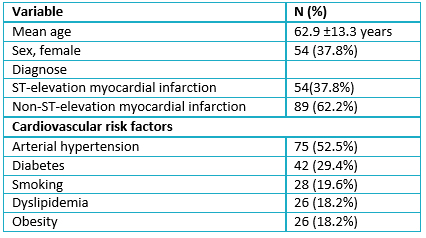 Table 1. Demographical and clinical characteristics of the patients selected with established coronary disease, Hospital Cayetano Heredia 2011-2013.
Table 1. Demographical and clinical characteristics of the patients selected with established coronary disease, Hospital Cayetano Heredia 2011-2013.

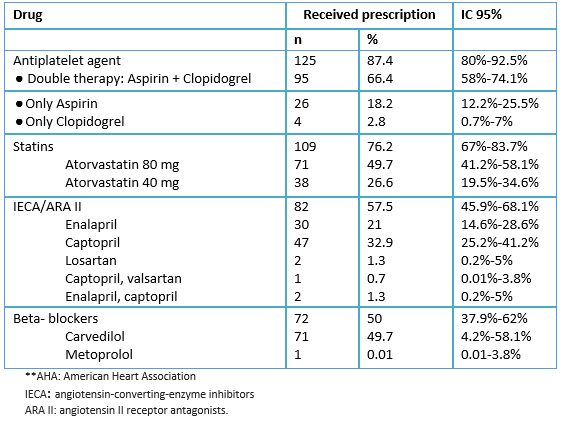 Proportion of patients with established coronary disease who received the Class I Level of Evidence A recommendations at discharge according to the AHA’s clinical practice guidelines.
Proportion of patients with established coronary disease who received the Class I Level of Evidence A recommendations at discharge according to the AHA’s clinical practice guidelines.

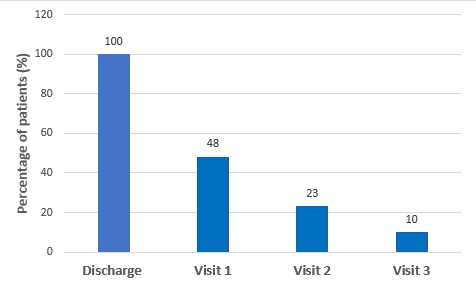 Figure 1. Percentage of patients with established coronary disease at discharge, and at first, second and third outpatient follow-up visit with the Cardiology Service.
Figure 1. Percentage of patients with established coronary disease at discharge, and at first, second and third outpatient follow-up visit with the Cardiology Service.

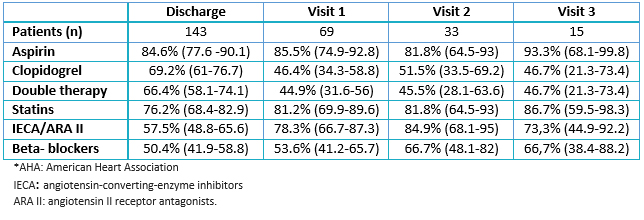 Table 3. Proportion of patients with established coronary disease who received the Class I Level of Evidence A recommendations from discharge until the third follow-up outpatient visit according to the AHA’s clinical practice guidelines.
Table 3. Proportion of patients with established coronary disease who received the Class I Level of Evidence A recommendations from discharge until the third follow-up outpatient visit according to the AHA’s clinical practice guidelines.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
La enfermedad cardiovascular constituye la principal causa de mortalidad a nivel mundial. Cuando se presenta un infarto agudo de miocardio se deben instaurar medidas en prevención secundaria, las cuales pueden disminuir la mortalidad en 50%. Las guías de práctica clínica establecen que un tratamiento médico óptimo se basa en cuatro grupos de fármacos: antiagregantes plaquetarios, estatinas, β-bloqueadores e inhibidores de la enzima convertidora de angiotensina o antagonistas de los receptores de la angiotensina II.
OBJETIVO
Determinar la adherencia a las recomendaciones de las guías de práctica clínica basadas en evidencia, sobre prevención secundaria en enfermedad coronaria establecida.
MÉTODOS
Se realizó un estudio observacional, tipo cohorte retrospectiva, en el Hospital Cayetano Heredia en Lima, Perú. Se incluyeron pacientes con diagnóstico confirmado de síndrome coronario agudo desde el 1 de febrero de 2011 hasta el 28 de febrero de 2013. Los datos que se recolectaron incluyeron anamnesis, examen físico, exámenes auxiliares y terapia médica al alta. Además, las prescripciones médicas fueron seguidas al primer, tercer y sexto mes posterior al alta. Se compararon las prescripciones médicas con las recomendaciones tipo I, nivel de evidencia A, de la guía de práctica clínica de la American Heart Association.
RESULTADOS
Se estudiaron 143 pacientes. De estos, 54 (37,8%) tuvieron infarto de miocardio con ST elevado y 89 (62,2%) pacientes tuvieron un infarto de miocardio con ST no elevado o angina inestable. Las cuatro estrategias terapéuticas seleccionadas para la prevención secundaria en enfermedad coronaria fueron indicadas en 40 (28%) pacientes al alta y solo en 12,6%, 7% y 3,5% en el primer, tercer y sexto mes de seguimiento, respectivamente. Además, se describió la adherencia del paciente a asistir a la consulta en el servicio de cardiología al primer, tercer y sexto mes, observándose una reducción importante desde 48% en la primera visita, hasta 10% en la última.
CONCLUSIONES
La adherencia médica a las guías clínicas sobre prevención secundaria en enfermedad coronaria es subóptima, alcanzando un porcentaje menor al 50%.
 Authors:
Zaira Castañeda-Amado [1,2 ], Lesly Calixto-Aguilar[1,2], César Loza Munarriz[2], Félix A Medina Palomino[3]
Authors:
Zaira Castañeda-Amado [1,2 ], Lesly Calixto-Aguilar[1,2], César Loza Munarriz[2], Félix A Medina Palomino[3]
Affiliation:
[1] Facultad de Medicina, Universidad Peruana Cayetano Heredia, Lima, Perú
[2] Unidad de Epidemiología Clínica, Facultad de Medicina, Universidad Peruana Cayetano Heredia, Lima, Perú
[3] Unidad de Bienestar y Desarrollo del Recurso Humano y Docente, Facultad de Medicina, Universidad Peruana Cayetano Heredia, Lima, Perú
E-mail: lesly.calixto.a@upch.pe
Author address:
[1] Avenida Honoro Delgado 430
Urbanización Ingeniería
Lima
Perú

Citation: Castañeda-Amado Z , Calixto-Aguilar L, Loza Munarriz C, Medina Palomino FA. Medical compliance to evidence-based clinical guidelines on secondary prevention of coronary heart disease in a hospital from Lima, Peru: a retrospective study. Medwave 2017 Jun;17(5):e6989 doi: 10.5867/medwave.2017.05.6989
Submission date: 10/2/2017
Acceptance date: 18/6/2017
Publication date: 29/6/2017
Origin: not requested
Type of review: reviewed by four external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- World Health Organization. Global status report on noncommunicable diseases. WHO; 2010. [on line]. | Link |
- Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005 Apr 21;352(16):1685-95. | PubMed |
- Institute of Medicine [Internet]. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Washington (DC); US: National Academies Press; 2010. | Link |
- Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011 Nov 29;124(22):2458-73. | CrossRef | PubMed |
- Sanfélix-Gimeno G, Peiró S, Ferreros I, Pérez-Vicente R, Librero J, Catalá-López F, et al. Adherence to evidence-based therapies after acute coronary syndrome: a retrospective population-based cohort study linking hospital, outpatient, and pharmacy health information systems in Valencia, Spain. J Manag Care Pharm. 2013 Apr;19(3):247-57. | PubMed |
- Flores-Mateo G, Grau M, O'Flaherty M, Ramos R, Elosua R, Violan-Fors C, et al. [Analyzing the coronary heart disease mortality decline in a Mediterranean population: Spain 1988-2005]. Rev Esp Cardiol. 2011 Nov;64(11):988-96. | CrossRef | PubMed |
- Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL, Brindis RG, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006 Apr 26;295(16):1912-20. | PubMed |
- Christopher G, McMurray J. Using Measures of Disease Progression to Determine Therapeutic Effect. JACC. 2006; 48(3):434–7. | Link |
- Lee JH, Yang DH, Park HS, Cho Y, Jeong MH, Kim YJ, et al. Suboptimal use of evidence-based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J. 2010 Jun;159(6):1012-9. | CrossRef | PubMed |
- Berwanger O, Guimarães HP, Laranjeira LN, Cavalcanti AB, Kodama AA, Zazula AD, et al. Effect of a multifaceted intervention on use of evidence-based therapies in patients with acute coronary syndromes in Brazil: the BRIDGE-ACS randomized trial. JAMA. 2012 May 16;307(19):2041-9. | CrossRef | PubMed |
- Redfern J, Hyun K, Chew DP, Astley C, Chow C, Aliprandi-Costa B, et al. Prescription of secondary prevention medications, lifestyle advice, and referral to rehabilitation among acute coronary syndrome inpatients: results from a large prospective audit in Australia and New Zealand. Heart. 2014 Aug;100(16):1281-8. | CrossRef | PubMed |
- Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005 Feb 1;111(4):499-510. | PubMed |
- Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228. | CrossRef | PubMed |
- O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29;127(4):529-55. | CrossRef | PubMed |
- Thygesen K, Alpert J, Jaffe A, Simoons M, Chaitman B, White H, et al. Third universal definition of myocardial infarction. Circulation. 2012 Oct 16;126(16):2020-35. | CrossRef | PubMed |
- National Library of Medicine. Estados Unidos. MeSH Descriptor Data: Guideline Adherence; 2016
- Kassab YW, Hassan Y, Aziz NA, Akram H, Ismail O. Use of evidence-based therapy for the secondary prevention of acute coronary syndromes in Malaysian practice. J Eval Clin Pract. 2013 Aug;19(4):658-63. | CrossRef | PubMed |
- Al-Zakwani I, Sulaiman K, Al Za'abi M, Panduranga P, Al-Habib K, Asaad N, et al. Impact of evidence-based cardiac medication on short-and long-term mortality in 7,567 acute coronary syndrome patients in the Gulf RACE-II registry. Int J Clin Pharmacol Ther. 2012 Jun;50(6):418-25. | CrossRef | PubMed |
- Atar D, Bode C, Stuerzenbecher A, Verheugt FW. Anticoagulants for secondary prevention after acute myocardial infarction: lessons from the past decade. Fundam Clin Pharmacol. 2014 Aug;28(4):353-63. | CrossRef | PubMed |
- Mancini GB, Gosselin G, Chow B, Kostuk W, Stone J, Yvorchuk KJ, et al. Canadian Cardiovascular Society guidelines for the diagnosis and management of stable ischemic heart disease. Can J Cardiol. 2014 Aug;30(8):837-49. | CrossRef | PubMed |
- Arnold SV, Spertus JA, Masoudi FA, Daugherty SL, Maddox TM, Li Y, et al. Beyond medication prescription as performance measures: optimal secondary prevention medication dosing after acute myocardial infarction. J Am Coll Cardiol. 2013 Nov 5;62(19):1791-801. | CrossRef | PubMed |
- Sposito AC, Caramelli B, Fonseca FA, Bertolami MC, Afiune NA, Souza AD, et al. Sociedade Brasileira de Cardiologia. IV Diretrizes brasileiras para dislipidemias e prevenção da aterosclerose. Arq Bras Cardiol. 2013; 101(4):supl.1. | CrossRef |
- Vermeer NS, Bajorek BV. Utilization of evidence-based therapy for the secondary prevention of acute coronary syndromes in Australian practice. J Clin Pharm Ther. 2008 Dec;33(6):591-601. | CrossRef | PubMed |
- Thakkar JB, Chow CK. Adherence to secondary prevention therapies in acute coronary syndrome. Med J Aust. 2014 Nov 17;201(10):S106-9. | PubMed |
- Branch W, Higgins S. Inercia clínica: la dificultad de superarla Rev Esp Cardiol. 2010;63(12):1399-401. | Link |
- Khonsari S, Subramanian P, Chinna K, Latif LA, Ling LW, Gholami O. Effect of a reminder system using an automated short message service on medication adherence following acute coronary syndrome. Eur J Cardiovasc Nurs. 2015 Apr;14(2):170-9. | CrossRef | PubMed |
- Ho PM, Lambert-Kerzner A, Carey EP, Fahdi IE, Bryson CL, Melnyk SD, et al. Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med. 2014 Feb 1;174(2):186-93. | CrossRef | PubMed |
- Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999 Oct 20;282(15):1458-65. | PubMed |
 World Health Organization. Global status report on noncommunicable diseases. WHO; 2010. [on line]. | Link |
World Health Organization. Global status report on noncommunicable diseases. WHO; 2010. [on line]. | Link | Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005 Apr 21;352(16):1685-95. | PubMed |
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005 Apr 21;352(16):1685-95. | PubMed | Institute of Medicine [Internet]. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Washington (DC); US: National Academies Press; 2010. | Link |
Institute of Medicine [Internet]. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Washington (DC); US: National Academies Press; 2010. | Link | Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011 Nov 29;124(22):2458-73. | CrossRef | PubMed |
Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011 Nov 29;124(22):2458-73. | CrossRef | PubMed | Sanfélix-Gimeno G, Peiró S, Ferreros I, Pérez-Vicente R, Librero J, Catalá-López F, et al. Adherence to evidence-based therapies after acute coronary syndrome: a retrospective population-based cohort study linking hospital, outpatient, and pharmacy health information systems in Valencia, Spain. J Manag Care Pharm. 2013 Apr;19(3):247-57. | PubMed |
Sanfélix-Gimeno G, Peiró S, Ferreros I, Pérez-Vicente R, Librero J, Catalá-López F, et al. Adherence to evidence-based therapies after acute coronary syndrome: a retrospective population-based cohort study linking hospital, outpatient, and pharmacy health information systems in Valencia, Spain. J Manag Care Pharm. 2013 Apr;19(3):247-57. | PubMed | Flores-Mateo G, Grau M, O'Flaherty M, Ramos R, Elosua R, Violan-Fors C, et al. [Analyzing the coronary heart disease mortality decline in a Mediterranean population: Spain 1988-2005]. Rev Esp Cardiol. 2011 Nov;64(11):988-96. | CrossRef | PubMed |
Flores-Mateo G, Grau M, O'Flaherty M, Ramos R, Elosua R, Violan-Fors C, et al. [Analyzing the coronary heart disease mortality decline in a Mediterranean population: Spain 1988-2005]. Rev Esp Cardiol. 2011 Nov;64(11):988-96. | CrossRef | PubMed | Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL, Brindis RG, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006 Apr 26;295(16):1912-20. | PubMed |
Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL, Brindis RG, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006 Apr 26;295(16):1912-20. | PubMed | Christopher G, McMurray J. Using Measures of Disease Progression to Determine Therapeutic Effect. JACC. 2006; 48(3):434–7. | Link |
Christopher G, McMurray J. Using Measures of Disease Progression to Determine Therapeutic Effect. JACC. 2006; 48(3):434–7. | Link | Lee JH, Yang DH, Park HS, Cho Y, Jeong MH, Kim YJ, et al. Suboptimal use of evidence-based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J. 2010 Jun;159(6):1012-9. | CrossRef | PubMed |
Lee JH, Yang DH, Park HS, Cho Y, Jeong MH, Kim YJ, et al. Suboptimal use of evidence-based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J. 2010 Jun;159(6):1012-9. | CrossRef | PubMed | Berwanger O, Guimarães HP, Laranjeira LN, Cavalcanti AB, Kodama AA, Zazula AD, et al. Effect of a multifaceted intervention on use of evidence-based therapies in patients with acute coronary syndromes in Brazil: the BRIDGE-ACS randomized trial. JAMA. 2012 May 16;307(19):2041-9. | CrossRef | PubMed |
Berwanger O, Guimarães HP, Laranjeira LN, Cavalcanti AB, Kodama AA, Zazula AD, et al. Effect of a multifaceted intervention on use of evidence-based therapies in patients with acute coronary syndromes in Brazil: the BRIDGE-ACS randomized trial. JAMA. 2012 May 16;307(19):2041-9. | CrossRef | PubMed | Redfern J, Hyun K, Chew DP, Astley C, Chow C, Aliprandi-Costa B, et al. Prescription of secondary prevention medications, lifestyle advice, and referral to rehabilitation among acute coronary syndrome inpatients: results from a large prospective audit in Australia and New Zealand. Heart. 2014 Aug;100(16):1281-8. | CrossRef | PubMed |
Redfern J, Hyun K, Chew DP, Astley C, Chow C, Aliprandi-Costa B, et al. Prescription of secondary prevention medications, lifestyle advice, and referral to rehabilitation among acute coronary syndrome inpatients: results from a large prospective audit in Australia and New Zealand. Heart. 2014 Aug;100(16):1281-8. | CrossRef | PubMed | Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005 Feb 1;111(4):499-510. | PubMed |
Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005 Feb 1;111(4):499-510. | PubMed | Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228. | CrossRef | PubMed |
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228. | CrossRef | PubMed | O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29;127(4):529-55. | CrossRef | PubMed |
O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29;127(4):529-55. | CrossRef | PubMed | Thygesen K, Alpert J, Jaffe A, Simoons M, Chaitman B, White H, et al. Third universal definition of myocardial infarction. Circulation. 2012 Oct 16;126(16):2020-35. | CrossRef | PubMed |
Thygesen K, Alpert J, Jaffe A, Simoons M, Chaitman B, White H, et al. Third universal definition of myocardial infarction. Circulation. 2012 Oct 16;126(16):2020-35. | CrossRef | PubMed | National Library of Medicine. Estados Unidos. MeSH Descriptor Data: Guideline Adherence; 2016
National Library of Medicine. Estados Unidos. MeSH Descriptor Data: Guideline Adherence; 2016  Kassab YW, Hassan Y, Aziz NA, Akram H, Ismail O. Use of evidence-based therapy for the secondary prevention of acute coronary syndromes in Malaysian practice. J Eval Clin Pract. 2013 Aug;19(4):658-63. | CrossRef | PubMed |
Kassab YW, Hassan Y, Aziz NA, Akram H, Ismail O. Use of evidence-based therapy for the secondary prevention of acute coronary syndromes in Malaysian practice. J Eval Clin Pract. 2013 Aug;19(4):658-63. | CrossRef | PubMed | Al-Zakwani I, Sulaiman K, Al Za'abi M, Panduranga P, Al-Habib K, Asaad N, et al. Impact of evidence-based cardiac medication on short-and long-term mortality in 7,567 acute coronary syndrome patients in the Gulf RACE-II registry. Int J Clin Pharmacol Ther. 2012 Jun;50(6):418-25. | CrossRef | PubMed |
Al-Zakwani I, Sulaiman K, Al Za'abi M, Panduranga P, Al-Habib K, Asaad N, et al. Impact of evidence-based cardiac medication on short-and long-term mortality in 7,567 acute coronary syndrome patients in the Gulf RACE-II registry. Int J Clin Pharmacol Ther. 2012 Jun;50(6):418-25. | CrossRef | PubMed | Atar D, Bode C, Stuerzenbecher A, Verheugt FW. Anticoagulants for secondary prevention after acute myocardial infarction: lessons from the past decade. Fundam Clin Pharmacol. 2014 Aug;28(4):353-63. | CrossRef | PubMed |
Atar D, Bode C, Stuerzenbecher A, Verheugt FW. Anticoagulants for secondary prevention after acute myocardial infarction: lessons from the past decade. Fundam Clin Pharmacol. 2014 Aug;28(4):353-63. | CrossRef | PubMed | Mancini GB, Gosselin G, Chow B, Kostuk W, Stone J, Yvorchuk KJ, et al. Canadian Cardiovascular Society guidelines for the diagnosis and management of stable ischemic heart disease. Can J Cardiol. 2014 Aug;30(8):837-49. | CrossRef | PubMed |
Mancini GB, Gosselin G, Chow B, Kostuk W, Stone J, Yvorchuk KJ, et al. Canadian Cardiovascular Society guidelines for the diagnosis and management of stable ischemic heart disease. Can J Cardiol. 2014 Aug;30(8):837-49. | CrossRef | PubMed | Arnold SV, Spertus JA, Masoudi FA, Daugherty SL, Maddox TM, Li Y, et al. Beyond medication prescription as performance measures: optimal secondary prevention medication dosing after acute myocardial infarction. J Am Coll Cardiol. 2013 Nov 5;62(19):1791-801. | CrossRef | PubMed |
Arnold SV, Spertus JA, Masoudi FA, Daugherty SL, Maddox TM, Li Y, et al. Beyond medication prescription as performance measures: optimal secondary prevention medication dosing after acute myocardial infarction. J Am Coll Cardiol. 2013 Nov 5;62(19):1791-801. | CrossRef | PubMed | Sposito AC, Caramelli B, Fonseca FA, Bertolami MC, Afiune NA, Souza AD, et al. Sociedade Brasileira de Cardiologia. IV Diretrizes brasileiras para dislipidemias e prevenção da aterosclerose. Arq Bras Cardiol. 2013; 101(4):supl.1. | CrossRef |
Sposito AC, Caramelli B, Fonseca FA, Bertolami MC, Afiune NA, Souza AD, et al. Sociedade Brasileira de Cardiologia. IV Diretrizes brasileiras para dislipidemias e prevenção da aterosclerose. Arq Bras Cardiol. 2013; 101(4):supl.1. | CrossRef | Vermeer NS, Bajorek BV. Utilization of evidence-based therapy for the secondary prevention of acute coronary syndromes in Australian practice. J Clin Pharm Ther. 2008 Dec;33(6):591-601. | CrossRef | PubMed |
Vermeer NS, Bajorek BV. Utilization of evidence-based therapy for the secondary prevention of acute coronary syndromes in Australian practice. J Clin Pharm Ther. 2008 Dec;33(6):591-601. | CrossRef | PubMed | Thakkar JB, Chow CK. Adherence to secondary prevention therapies in acute coronary syndrome. Med J Aust. 2014 Nov 17;201(10):S106-9. | PubMed |
Thakkar JB, Chow CK. Adherence to secondary prevention therapies in acute coronary syndrome. Med J Aust. 2014 Nov 17;201(10):S106-9. | PubMed | Branch W, Higgins S. Inercia clínica: la dificultad de superarla Rev Esp Cardiol. 2010;63(12):1399-401. | Link |
Branch W, Higgins S. Inercia clínica: la dificultad de superarla Rev Esp Cardiol. 2010;63(12):1399-401. | Link | Khonsari S, Subramanian P, Chinna K, Latif LA, Ling LW, Gholami O. Effect of a reminder system using an automated short message service on medication adherence following acute coronary syndrome. Eur J Cardiovasc Nurs. 2015 Apr;14(2):170-9. | CrossRef | PubMed |
Khonsari S, Subramanian P, Chinna K, Latif LA, Ling LW, Gholami O. Effect of a reminder system using an automated short message service on medication adherence following acute coronary syndrome. Eur J Cardiovasc Nurs. 2015 Apr;14(2):170-9. | CrossRef | PubMed | Ho PM, Lambert-Kerzner A, Carey EP, Fahdi IE, Bryson CL, Melnyk SD, et al. Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med. 2014 Feb 1;174(2):186-93. | CrossRef | PubMed |
Ho PM, Lambert-Kerzner A, Carey EP, Fahdi IE, Bryson CL, Melnyk SD, et al. Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med. 2014 Feb 1;174(2):186-93. | CrossRef | PubMed | Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999 Oct 20;282(15):1458-65. | PubMed |
Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999 Oct 20;282(15):1458-65. | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








