Key Words: hip, hip congenital dislocation, arthroscopy, osteotomy
Abstract
Purpose
To describe patient-reported outcomes, radiological results, and revision to total hip replacement in patients with hip dysplasia that underwent periacetabular osteotomy as isolated treatment or concomitant with hip arthroscopy.
Methods
Case series study. Between 2014 and 2017, patients were included if they complained of hip pain and had a lateral center-edge angle ≤ of 20°. Exclusion criteria included an in-maturate skeleton, age of 40 or older, previous hip surgery, concomitant connective tissue related disease, and Tönnis osteoarthritis grade ≥ 1. All patients were studied before surgery with an anteroposterior pelvis radiograph, false-profile radiograph, and magnetic resonance imaging. Magnetic resonance imaging was used to assess intraarticular lesions, and if a labral or chondral injury was found, concomitant hip arthroscopy was performed. The non-parametric median test for paired data was used to compare radiological measures (anterior and lateral center-edge angle, Tönnis angle, and extrusion index) after and before surgery. Survival analysis was performed using revision to total hip arthroplasty as a failure. Kaplan Meier curve was estimated. The data were processed using Stata.
Results
A total of 15 consecutive patients were included; 14 (93%) were female patients. The median follow-up was 3.5 years (range, 2 to 8 years). The median age was 20 (range 13 to 32). Lateral center-edge angle, Tönnis angle, and extrusion index correction achieved statistical significance. Seven patients (47%) underwent concomitant hip arthroscopy; three of them (47%) were bilateral (10 hips). The labrum was repaired in six cases (60%). Three patients (15%) required revision with hip arthroplasty, and no hip arthroscopy-related complications are reported in this series.
Conclusion
To perform a hip arthroscopy concomitant with periacetabular osteotomy did not affect the acetabular correction. Nowadays, due to a lack of conclusive evidence, a case by case decision seems more appropriate to design a comprehensive treatment.
Main messages
|
Introduction
Developmental dysplasia of the hip—also known as congenital hip dysplasia—is a multifactorial disease characterized by an alteration in the development of the acetabulum or the proximal femur[1]. Risk factors like female gender, breech positioning in the third trimester, and family history are poor predictors, so surveillance is mandatory for early diagnosis and treatment to prevent impairing the quality of life[2].
Different screening programs in newborns for congenital hip dysplasia have been proposed. For example, in Chile, congenital hip dysplasia surveillance is performed using a hip radiograph at three months of age for all newborns. It is included in the Explicit Health Guarantees—a set of benefits guaranteed by law allowing access, opportunity, financial protection, and quality of care in a limited list of diseases[3]. Nevertheless, a recent meta-analysis shows insufficient evidence to recommend one strategy over another[4].
Despite efforts, many patients with congenital hip dysplasia are underdiagnosed or remain with residual deformities after physeal closure, so they require medical evaluation for hip pain[5]. The deformities lead to hip instability, increased joint-loading pressures, labral lesion, and osteochondral damage. These patients are at an increased risk to develop osteoarthritis than the general population and patients with other hip pathologies like femoroacetabular impingement[1],[6]. Congenital hip dysplasia is estimated to cause secondary osteoarthrosis by age fifty in 25 percent to 50 percent of patients[7].
Congenital hip dysplasia in patients with a mature skeleton is classified according to the acetabular coverage degree in an anteroposterior pelvic radiograph. The most common angle used is the lateral center-edge angle, also known as the Wiberg angle (Figure 1). The angle is normal between 25° and 40°, being 20-25° a borderline congenital hip dysplasia and less than 20° a true congenital hip dysplasia[8].
Figure 1. A 24-year-old woman with severe hip dysplasia.
The treatment for young adults who have symptomatic joint disease aims to prevent or delay osteoarthritis. Non-surgical measurements and joint preservations procedures are treatment options; the last option includes acetabular or femoral osteotomies and hip arthroscopy[9].
The Bernese periacetabular osteotomy is a crucial procedure to restore hip mechanics in patients with true hip dysplasia[10]. This procedure aims to correct the acetabular deformity through a series of bone cuts, which allows the acetabulum to be reoriented in a more medial position and with greater anterior and lateral coverage of the femoral head[11]. The advantages of periacetabular osteotomy compared with other osteotomies are that the posterior hemipelvis remains intact, making the osteotomy more intrinsically stable and allowing for early mobilization weight-bearing. Also, it can be done by a single incision[6].
The ideal patient to undergo periacetabular osteotomy is under 30, without or with slight preoperative osteoarthritis. A survival rate between 60 percent and 90 percent at 20 years after surgery could be expected[12]. However, residual impingement, labrum tears, and chondral injury are potential causes for recurrent symptoms, diminishing quality of life, and revision after periacetabular osteotomy[13],[14]. Patients with hip dysplasia and intraarticular injuries could benefit from performing a concomitant hip arthroscopy along with periacetabular osteotomy[15].
Intraarticular pathology has been reported in association with hip dysplasia[16]. Ross et al.[14] reported the result of 74 periacetabular osteotomies associated with hip arthroscopy performed in one stage. They described 65.8% of a labral lesion, 68.5% of cartilage lesion, and 59.8% of combined lesions. Matheney et al.[13] report a cohort of 135 periacetabular osteotomies, where 11% has to be revised with hip arthroscopy for a labral lesion. This subgroup of patients could benefit from a hip arthroscopy when there is a repairable intraarticular injury.
There is no consensus if intra-articular pathology should be addressed before, simultaneously, or after periacetabular osteotomy[16]. Several studies report improvement and good clinical results for isolated arthroscopy for mild dysplasia and good results after periacetabular osteotomy for severe hip dysplasia. Still, few studies report the results of both procedures concomitantly[17],[18].
The purpose of this study is to describe patient-reported outcomes, radiological results, and revision to total hip replacement in patients with hip dysplasia that underwent periacetabular osteotomy as isolated treatment or concomitant with hip arthroscopy.
Methods
We performed a case series of consecutive patients that required periacetabular osteotomy for hip dysplasia between 2014 and 2017. Patients were included if they complained of hip pain that compromised their quality of life without response to medical treatment and if an anteroposterior pelvis radiograph demonstrates a Wiberg angle less than 20°. Exclusion criteria were an in-maturate skeleton, age 40 or older, previous hip surgery, concomitant connective tissue disease, and Tönnis osteoarthritis grade 1 or more. The local ethics committee board approved this study. All patients gave written consent prior to surgery and at the final follow-up when they completed the patient-reported outcome survey.
Before surgery, all patients underwent anteroposterior pelvis and false-profile radiographs and hip magnetic resonance imaging. In the anteroposterior pelvis view, the Wiberg angle, Tönnis Angle, and extrusion index were measured; in the false-profile view, the anterior center-edge angle was measured[19],[20]. Both radiographic views performed were retaken after surgery, and the same angles were recorded (Figure 1). Magnetic resonance imaging was used to assess intraarticular lesions, and if a labral tear or focal chondral lesion was found, concomitant hip arthroscopy was performed.
A senior hip surgeon performed all procedures. If a hip arthroscopy was performed, the patient was positioned supine in a traction table with a well-padded perineal post[21]. Under fluoroscopy, the hip seal was broken, and traction was applied. Anterolateral and mid-anterior portals were created[22]. An in-between portal capsulotomy is performed, then a systematic diagnostic arthroscopic is done with a 70° four millimeters arthroscope. The labrum and cartilage status are carefully assessed, and if present, chondral acetabular lesions are described according to the Beck et al. classification[23]. Only minimal acetabuloplasty is carried-out in cases that require labrum repair with anchors; otherwise, no acetabuloplasty is performed. In all cases, the capsule was closed.
After hip arthroscopy, and in the same anesthesia, the patient is placed supine in the radiolucent table. Periacetabular osteotomy is performed as described by Ganz et al.[11] and modified by Maldonado et al.[24]. An anterior hip approach is used; superficial dissection is performed with caution to minimize injury to the lateral femoral cutaneous nerve. The ischium and pubis are identified by developing an interval between the medial joint capsule and psoas muscle. After that, an incomplete osteotomy of the ischium, followed by a complete osteotomy of the pubis, is performed. The Iliac bone is then exposed, and an incomplete osteotomy from just below the anterior superior iliac spine to the pelvic brim is performed. The final bone cut is done to connect the third cut with the ischium osteotomy (first cut), allowing for the fragment mobilization to perform the desired correction under fluoroscopy guidance. Once the desired correction is achieved, the fragment is temporarily fixed, and the hip is bent up to 90 degrees to assess the presence of impingement. Finally, the fragment is held with at least three 4.5-millimeter fully threaded screws. If any impingement is noted with a flexion adduction internal rotation maneuvers, an open femoral osteochrondroplasty is performed.
Rehabilitation begins the first day after surgery, guided by a physiotherapist. Partial weight-bearing with two canes and a range of motion between zero to 90 degrees of hip flexion is allowed. After four weeks, full weight-bearing is encouraged. Patients can resume running between six to nine months depending on the degree of consolidation and muscle status.
The patient functional reported outcome was evaluated with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)[25] and the Hip disability and Osteoarthritis Outcome Score (HOOS)[26]. Patients were contacted by telephone in-between the 12 to 18 months after surgery by a hip fellow resident. The minimum follow-up in the clinical record was 24 months.
Continuous variables are summarized in median, range, and interquartile range (p25 to p75), and absolute frequency and percent was used for discrete variables. Non-parametric median test for paired data was used to compare radiological measurements after and before surgery. Radiological measurements and functional outcomes are compared between periacetabular osteotomy alone and a mix of periacetabular osteotomy and hip arthroscopy, using a non-parametric median test for unpaired data. Survival analysis was performed using revision to total hip arthroplasty as a failure. The Kaplan Meier curve was estimated. The data were processed using Stata version 15 (StataCorp LP, College Station, Texas, USA).
Results
A total of fifteen consecutive patients were included, fourteen of which (93%) were female patients, and one was male (0.7%). The median age was 20 (range, 13 to 32). Four patients (27%) underwent bilateral surgery, and the waiting time for the second procedure was three months in one case and 12 months for the other three patients. Seven patients (47%) underwent concomitant hip arthroscopy; three of them (47%) were bilateral (10 hips). Demographic data between periacetabular osteotomy plus hip arthroscopy group and isolated periacetabular osteotomy is compared in Table 1.
Preoperative median Wiberg angle was 12° (range, -29° to 19°) and a median correction of 16° (range, 7° to 53°) was achieved after periacetabular osteotomy, which was significant (p = 0.001) (see Table 2). The postoperative median Wiberg angle was 25° (range, 8° to 34°). In the anterior center-edge angle, the median correction was lower than in the Wiberg angle, reaching 8° (range, 0° to 20°) without statical significance (Table 2). Median Tönnis angle and extrusion index correction was 14° (range, 1° to 32°) and 19% (range, 4% to 32%) respectively; both measurements reached significant statistical difference (Table 2). The comparison between periacetabular osteotomy and periacetabular osteotomy plus hip arthroscopy is summarized in Table 3, and only the anterior center-edge angle correction reached statistical difference.
Table 3. Radiological measurement before and after surgery by the group of treatment.
In the hip arthroscopy group, nine out of the ten hips had a labrum tear; in six cases (60%), it was detached and required labrum repair with anchors. In seven cases, the labrum was hyperplastic, and in three cases, it was degenerative. Also, a cartilage lesion was identified in seven (70%) cases. Five of them (50%) had a carpet phenomenon (also known as "wave sign") and were classified as a Beck type two lesion. In one case, the acetabular cartilage was rough and fibrillated (Beck type one lesion), and one case had a Beck type 3 lesion with a deep and extended flap. This last patient was the only one of this group that required revision to a total hip replacement. No femoral osteochrondroplasty, acetabuloplasty, or psoas release was performed in any case. No hip arthroscopy-related complications are reported in this series.
Patients reported a median of 130 points (range, 93 to 151) in the HOOS scale and of 86 points (range, 62 to 96) in the WOMAC scale. In Table 4, both functional scales are summarized by groups of treatment, and no significant difference was found.
The total cohort time at risk was 75 years. The median follow-up was 3.5 years (range, 2 to 8 years), which reached a survival of 0.85 (95% confidence interval: 0.51 to 0.96) (Figure 2). A total of three hips (16%) were revised to total hip arthroplasty (3 patients, 20%), two of which from the periacetabular osteotomy alone group. The incidence rate of failure was 0.039 per year.
Figure 2. Kaplan Meier survival estimate of the total cohort.
Discussion
This case series shows a significant correction of Wiberg angle, Tönnis angle, and extrusion index after periacetabular osteotomy, adding to the vast literature on good to excellent results in periacetabular osteotomy for hip dysplasia. Remarkably, this study shows that the amount of correction and the functional outcome is not significantly different between periacetabular osteotomy alone and periacetabular osteotomy plus hip arthroscopy. Also, no significant increase in complications or failure rate in the hip arthroscopy plus periacetabular osteotomy is reported.
A recent meta-analysis showed a paucity in reports of outcomes after periacetabular osteotomy plus hip arthroscopy so that no reliable conclusions could be made[18]. Nevertheless, it seems logical to include hip arthroscopy in the setting of periacetabular osteotomy if any intraarticular lesion is suspected or confirmed by imaging, as no study had shown an increase of complication compared to periacetabular osteotomy alone. Nowadays, a case by case decision basis seems more appropriate to design a comprehensive treatment strategy in the dysplastic population[17].
Intraarticular lesions are frequent in dysplastic patients[27], and hip arthroscopy is a powerful minimally invasive technique to address these lesions. Two main questions remain unclear to recommend hip arthroscopy concomitant with periacetabular osteotomy. First, is a failure after periacetabular osteotomy due to inadequate correction leading to impingement (overcorrection) or instability (under-correction)? Alternatively, failure is due to leave-alone intraarticular lesions like a labrum tear? The second question is, which intraarticular lesion and intraarticular procedure improve clinical outcomes after periacetabular osteotomy? Overcorrection should always be avoided, but under correction could occur unintentionally due to low volume acetabulum. Hip arthroscopy alone has demonstrated good mid-term functional results for borderline dysplasia[28], and special attention in this type of patients must be made to the capsular management to avoid instability[29]. Labrum and capsule have a crucial role in hip stability[30]; specifically, biomechanical studies have shown that iliofemoral ligament is a primary restrictor and labrum a secondary restrictor to external rotation and anterior translation of the femur[31]. Since the acetabular volume in dysplasia is lower than in normal patients, a perfect correction of acetabular coverage is not always possible, putting at risk of micro instability to the hip. If unintended under coverage, a labral tear or poor management of the capsule is added to this, the instability may increase, causing the osteotomy's early failure. Therefore, acetabular volume and under-correction could play a crucial to decide if intraarticular lesions should be addressed.
Chondral lesions are frequent in hip dysplasia, and even it has been described that a particular type of injury called "Outside-In Flap" is characteristic of chondral damage in hip dysplasia[32]. The presence of cartilage lesion jeopardizes the outcome of periacetabular osteotomy[13]; nevertheless, articular procedures like microfracture or chondroplasty when a high-grade chondral lesion is present have not achieved good outcome[33],[34],[35],[36], so it makes it difficult to perform a reliable conclusion about indication concomitant with periacetabular osteotomy.
Our comprehensive treatment strategy is always to perform a hip arthroscopy when a labral tear is shown in the magnetic resonance imaging. The first option is to repair the tear, as consistent better long-term results are achieved compared to labral resection[37]. If repair is not possible, labral reconstruction with iliotibial band graft is performed[38].
This study's limitations are that it is a low volume cohort and has no control group. Nevertheless, it contributes to the increasing trend to address intraarticular lesions seeking improvement in periacetabular osteotomy functional outcome and survival. Another limitation of this study is that the preoperative WOMAC and HOOS were not available. Finally, due to the design of the study, it is no possible to compare the functional outcomes between groups as the patients were intentionally selected according to the presence of an intraarticular lesion. However, considering that patients with intraarticular lesions are in a more advanced stage of hip dysplasia, to obtain similar functional results adding hip arthroscopy is a remarkable finding.
Conclusions
To perform a hip arthroscopy concomitant with periacetabular osteotomy does not increase the complication rate and did not affect the acetabular correction or clinical result. We recommend adding hip arthroscopy to periacetabular osteotomy when magnetic resonance imaging shows an intraarticular lesion as hip arthroscopy does not affect periacetabular osteotomy results outcomes of complications, alignment, and clinical outcome.
Meta-analyses and systematic reviews have not given a final recommendation on adding hip arthroscopy to periacetabular osteotomy due to the lack of evidence at present. Therefore, a case by case decision basis seems more appropriate to design a comprehensive treatment strategy in hip dysplasia. Particular attention should be taken when there is a high risk of low correction due to a low volume acetabulum, and magnetic resonance imaging shows a lesion of the labrum, given the high risk of instability if the labrum is not repaired.
Notes
Roles and contributions of authorship
CB: Conceptualization, formal analysis, writing (review and editing), supervision and project administration. JB: Conceptualization, formal analysis. RO, RW: Investigation and writing (original draft preparation). AM: Investigation, formal analysis, writing (review and editing), supervision.
JH: Writing (original draft preparation) and visualization. MB: Methodology, formal analysis, writing (original draft preparation, review and editing).
Conflicts of interest
The authors declare that they have no competing interests.
Funding
There was no funding for this research.
Ethics approval
This study was approved by the Hospital Clínico Universidad de Chile ethics research board, as stated in certificate number 18, issued on May 6, 2020.
Availability of data
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.

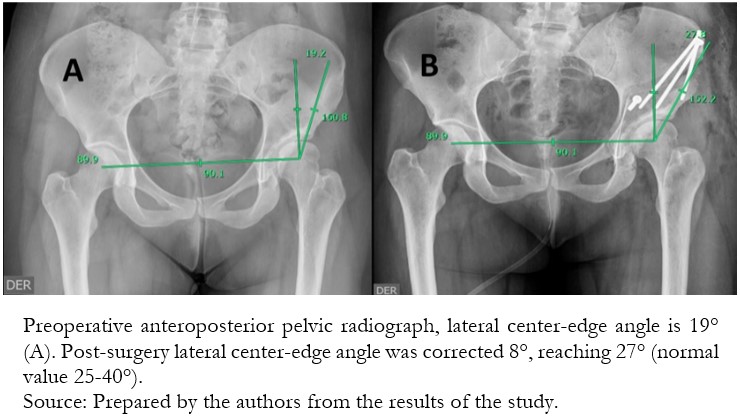 Figure 1. A 24-year-old woman with severe hip dysplasia.
Figure 1. A 24-year-old woman with severe hip dysplasia.

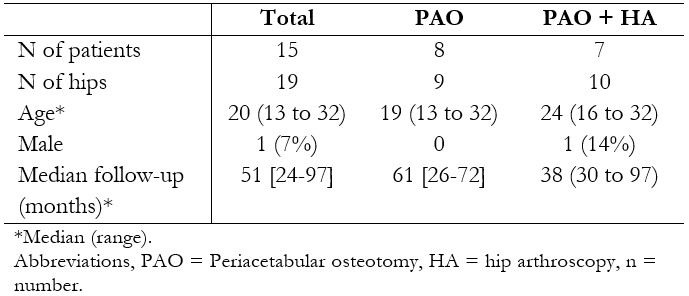 Table 1. Demographic data.
Table 1. Demographic data.

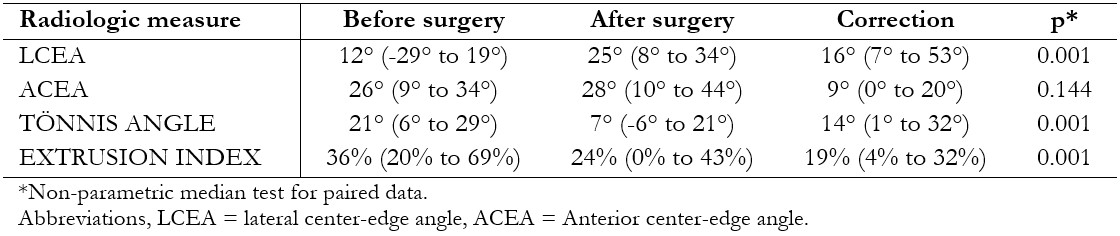 Table 2. Radiological measurement before and after surgery. LCEA, ACEA, Tönnis angle, and extrusion index reached a significant difference after surgery.
Table 2. Radiological measurement before and after surgery. LCEA, ACEA, Tönnis angle, and extrusion index reached a significant difference after surgery.

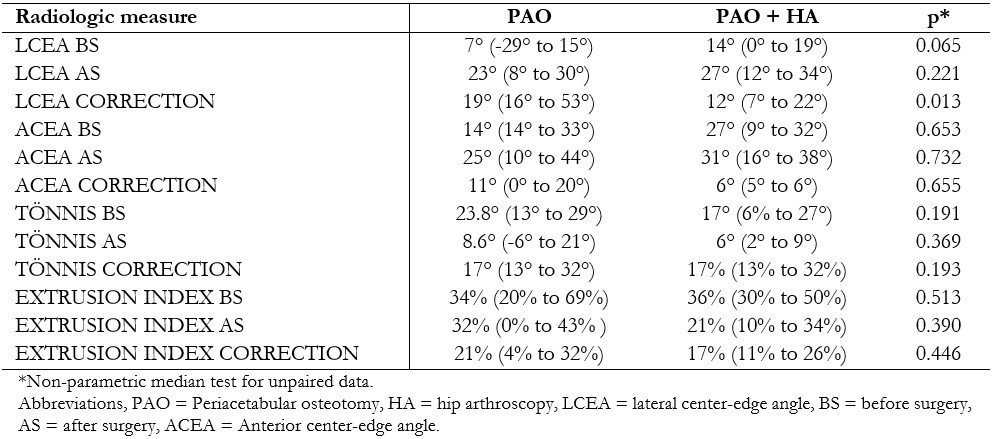 Table 3. Radiological measurement before and after surgery by the group of treatment.
Table 3. Radiological measurement before and after surgery by the group of treatment.

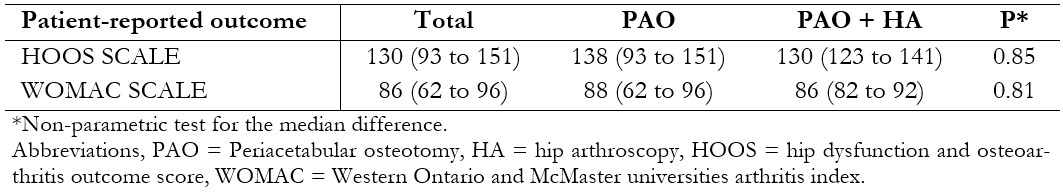 Table 4. Functional scores 12 to 18 months after surgery are shown. No statically difference was found between the groups of treatment.
Table 4. Functional scores 12 to 18 months after surgery are shown. No statically difference was found between the groups of treatment.

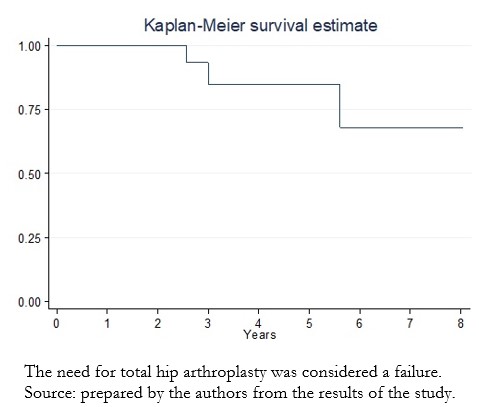 Figure 2. Kaplan Meier survival estimate of the total cohort.
Figure 2. Kaplan Meier survival estimate of the total cohort.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Objetivo
Describir los resultados funcionales, radiológicos y la tasa revisión a artroplastia total de cadera en una cohorte de pacientes con displasia de cadera que requirió osteotomía periacetabular como tratamiento aislado o concomitante con artroscopia de cadera.
Método
Estudio de series de casos. Fueron incluidos pacientes intervenidos quirúrgicamente entre 2014 y 2017. Los criterios de inclusión fueron dolor en la cadera y un ángulo lateral de centro borde ≤ 20°. Los criterios de exclusión fueron esqueleto maduro, edad de 40 años o más, cirugía previa de cadera, enfermedad concomitante relacionada con el tejido conectivo y coxartrosis grado ≥ 1 de Tönnis. Todos los pacientes fueron estudiados antes de la cirugía con una radiografía anteroposterior de pelvis, radiografía de falso perfil y resonancia magnética. En caso de pesquisar una lesión intrarticular en resonancia magnética se realizó una artroscopia concomitante a osteotomía periacetabular. La prueba mediana no paramétrica para datos no pareados se utilizó para comparar medidas radiológicas (ángulo del borde central anterior y lateral, ángulo de Tönnis e índice de extrusión) antes y después de la cirugía. El análisis de sobrevida se realizó utilizando la revisión de la artroplastia total de cadera como fracaso. Se estimó la curva de Kaplan Meier. Los datos se procesaron con Stata.
Resultados
Fueron incluidos un total de 15 pacientes consecutivos; Siete pacientes (47%) se sometieron a artroscopia de cadera concomitante, tres de ellos (47%) fueron bilaterales (10 caderas). La mediana de seguimiento fue de 3.5 años (rango, 2 a 8 años). La mediana de edad fue de 20 (rango 13 a 32). El ángulo de cobertura lateral preoperatorio era de 12° (rango, -29° a 19°) y posterior a la cirugía fue de 25° (rango, 8° a 34°), logrando una mediana de corrección de 16° (rango, 7° a 53°). El labrum fue reparado en seis casos (60%). Tres pacientes (15%) requirieron revisión con artroplastia de cadera, y no se informan complicaciones relacionadas con la artroscopia en esta serie.
Conclusión
Realizar una artroscopia concomitante con osteotomía periacetabular no afectó la corrección acetabular, ni el resultado clínico. Hoy en día, debido a la falta de evidencia concluyente, el realizar una artroscopía es una decisión que debe ser tomada caso a caso para un tratamiento integral.
 Authors:
Cristian Barrientos[1,2], Julián Brañes[1,2], Rodrigo Olivares[2], Rodrigo Wulf[1], Álvaro Martinez[2], Jaime Hinzpeter[1], Maximiliano Barahona[1]
Authors:
Cristian Barrientos[1,2], Julián Brañes[1,2], Rodrigo Olivares[2], Rodrigo Wulf[1], Álvaro Martinez[2], Jaime Hinzpeter[1], Maximiliano Barahona[1]
Affiliation:
[1] Departamento de Ortopedia y Traumatología en Hospital Clínico Universidad de Chile, Santiago, Chile
[2] Departamento de Ortopedia y Traumatología en Hospital San José, Santiago, Chile
E-mail: maxbarahonavasquez@gmail.com
Author address:
[1] Santos Dumont 999, 3rd Floor, office 351 Independencia, Santiago, Chile Postal code: 8380456

Citation: Barrientos C, Brañes J, Olivares R, Wulf R, Martinez A, Hinzpeter J, et al. Periacetabular osteotomy with concomitant hip arthroscopy: A case series with 24 months minimum follow-up. Medwave 2020;20(11):e8082 doi: 10.5867/medwave.2020.11.8082
Submission date: 16/5/2020
Acceptance date: 19/10/2020
Publication date: 23/12/2020
Origin: Not commissioned
Type of review: Externally peer-reviewed by three reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Breidel KE, Coobs BR. Evaluating and managing acetabular dysplasia in adolescents and young adults. JAAPA. 2019 Aug;32(8):32-37. | CrossRef | PubMed |
- Blankespoor M, Ferrell K, Reuter A, Reuter S. Developmental Dysplasia of the Hip in Infants - A Review for Providers. S D Med. 2020 May;73(5):223-227. | PubMed |
- Gobierno de Chile, Ministerio de Salud. Guía Clínica displasia luxante de cadera: diagnóstico y tratamiento precoz. Santiago: Minsal, 2010. [On line]. | Link |
- Shorter D, Hong T, Osborn DA. Cochrane Review: Screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health. 2013 Jan;8(1):11-54. | CrossRef | PubMed |
- Schmitz MR, Murtha AS, Clohisy JC; ANCHOR Study Group. Developmental Dysplasia of the Hip in Adolescents and Young Adults. J Am Acad Orthop Surg. 2020 Feb 1;28(3):91-101. | CrossRef | PubMed |
- Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005 Feb;87(2):254-9. | CrossRef | PubMed |
- Jakobsen SS, Overgaard S, Søballe K, Ovesen O, Mygind-Klavsen B, Dippmann CA, et al. The interface between periacetabular osteotomy, hip arthroscopy and total hip arthroplasty in the young adult hip. EFORT Open Rev. 2018 Jul 11;3(7):408-417. | CrossRef | PubMed |
- Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009 Aug;467(8):2041-52. | CrossRef | PubMed |
- Nunley RM, Prather H, Hunt D, Schoenecker PL, Clohisy JC. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Joint Surg Am. 2011 May;93 Suppl 2:17-21. | CrossRef | PubMed |
- Pascual-Garrido C, Harris MD, Clohisy JC. Innovations in Joint Preservation Procedures for the Dysplastic Hip "The Periacetabular Osteotomy". J Arthroplasty. 2017 Sep;32(9S):S32-S37. | CrossRef | PubMed |
- Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. 1988. Clin Orthop Relat Res. 2004 Jan;(418):3-8. | PubMed |
- Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008 Jul;466(7):1633-44. | CrossRef | PubMed |
- Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009 Sep;91(9):2113-23. | CrossRef | PubMed |
- Ross JR, Zaltz I, Nepple JJ, Schoenecker PL, Clohisy JC. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011 Jul;39 Suppl:72S-8S. | CrossRef | PubMed |
- Redmond JM, Gupta A, Stake CE, Domb BG. The prevalence of hip labral and chondral lesions identified by method of detection during periacetabular osteotomy: arthroscopy versus arthrotomy. Arthroscopy. 2014 Mar;30(3):382-8. | CrossRef | PubMed |
- Hartig-Andreasen C, Søballe K, Troelsen A. The role of the acetabular labrum in hip dysplasia. A literature overview. Acta Orthop. 2013 Feb;84(1):60-4. | CrossRef | PubMed |
- Adler KL, Giordano BD. The Utility of Hip Arthroscopy in the Setting of Acetabular Dysplasia: A Systematic Review. Arthroscopy. 2019 Jan;35(1):237-248. | CrossRef | PubMed |
- Lodhia P, Chandrasekaran S, Gui C, Darwish N, Suarez-Ahedo C, Domb BG. Open and Arthroscopic Treatment of Adult Hip Dysplasia: A Systematic Review. Arthroscopy. 2016 Feb;32(2):374-83. | CrossRef | PubMed |
- Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008 Nov;90 Suppl 4(Suppl 4):47-66. | CrossRef | PubMed |
- Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007 Jun;188(6):1540-52. | CrossRef | PubMed |
- Ilizaliturri VM. Arthroscopic treatment of FAI: Position, portals, and instrumentation. In: Femoroacetabular Impingement. Springer-Verlag Berlin Heidelberg; 2012:99–111. | CrossRef |
- Matsuda DK, Villamor A. The modified mid-anterior portal for hip arthroscopy. Arthrosc Tech. 2014 Jul 28;3(4):e469-74. | CrossRef | PubMed |
- Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004 Jan;(418):67-73. | PubMed |
- Maldonado DR, LaReau JM, Lall AC, Battaglia MR, Mohr MR, Domb BG. Concomitant Arthroscopy With Labral Reconstruction and Periacetabular Osteotomy for Hip Dysplasia. Arthrosc Tech. 2018 Oct 15;7(11):e1141-e1147. | CrossRef | PubMed |
- Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988 Dec;15(12):1833-40. | PubMed |
- Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003 May 30;4:10. | CrossRef | PubMed |
- Domb BG, Lareau JM, Baydoun H, Botser I, Millis MB, Yen YM. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res. 2014 Feb;472(2):674-80. | CrossRef | PubMed |
- Fukui K, Briggs KK, Trindade CA, Philippon MJ. Outcomes After Labral Repair in Patients With Femoroacetabular Impingement and Borderline Dysplasia. Arthroscopy. 2015 Dec;31(12):2371-9. | CrossRef | PubMed |
- Kuhns BD, Weber AE, Levy DM, Bedi A, Mather RC 3rd, Salata MJ, et al. Capsular Management in Hip Arthroscopy: An Anatomic, Biomechanical, and Technical Review. Front Surg. 2016 Mar 4;3:13. | CrossRef | PubMed |
- Bayne CO, Stanley R, Simon P, Espinoza-Orias A, Salata MJ, Bush-Joseph CA, et al. Effect of capsulotomy on hip stability-a consideration during hip arthroscopy. Am J Orthop (Belle Mead NJ). 2014 Apr;43(4):160-5. | PubMed |
- Myers CA, Register BC, Lertwanich P, Ejnisman L, Pennington WW, Giphart JE, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011 Jul;39 Suppl:85S-91S. | CrossRef | PubMed |
- Kraeutler MJ, Goodrich JA, Fioravanti MJ, Garabekyan T, Mei-Dan O. The "Outside-In" Lesion of Hip Impingement and the "Inside-Out" Lesion of Hip Dysplasia: Two Distinct Patterns of Acetabular Chondral Injury. Am J Sports Med. 2019 Oct;47(12):2978-2984. | CrossRef | PubMed |
- Domb BG, El Bitar YF, Lindner D, Jackson TJ, Stake CE. Arthroscopic hip surgery with a microfracture procedure of the hip: clinical outcomes with two-year follow-up. Hip Int. 2014 Sep-Oct;24(5):448-56. | CrossRef | PubMed |
- Domb BG, Redmond JM, Dunne KF, Stake CE, Gupta A. A matched-pair controlled study of microfracture of the hip with average 2-year follow-up: do full-thickness chondral defects portend an inferior prognosis in hip arthroscopy? Arthroscopy. 2015 Apr;31(4):628-34. | CrossRef | PubMed |
- Sansone M, Ahldén M, Jonasson P, Thomeé C, Swärd L, Collin D, et al. Outcome of hip arthroscopy in patients with mild to moderate osteoarthritis-A prospective study. J Hip Preserv Surg. 2015 Dec 26;3(1):61-7. | CrossRef | PubMed |
- Más Martínez J, Sanz-Reig J, Verdú Román CM, Bustamante Suárez de Puga D, Morales Santías M, Martínez Giménez E. Arthroscopic hip surgery with a microfracture procedure of acetabular full-thickness chondral damage. Cohort study with a 3-year follow-up. Rev Esp Cir Ortop Traumatol. 2018 Mar 10:S1888-4415(18)30018-3. | CrossRef | PubMed |
- Anwander H, Siebenrock KA, Tannast M, Steppacher SD. Labral Reattachment in Femoroacetabular Impingement Surgery Results in Increased 10-year Survivorship Compared With Resection. Clin Orthop Relat Res. 2017 Apr;475(4):1178-1188. | CrossRef | PubMed |
- Ejnisman L, Philippon MJ, Lertwanich P. Acetabular labral tears: diagnosis, repair, and a method for labral reconstruction. Clin Sports Med. 2011 Apr;30(2):317-29. | CrossRef | PubMed |
 Breidel KE, Coobs BR. Evaluating and managing acetabular dysplasia in adolescents and young adults. JAAPA. 2019 Aug;32(8):32-37. | CrossRef | PubMed |
Breidel KE, Coobs BR. Evaluating and managing acetabular dysplasia in adolescents and young adults. JAAPA. 2019 Aug;32(8):32-37. | CrossRef | PubMed | Blankespoor M, Ferrell K, Reuter A, Reuter S. Developmental Dysplasia of the Hip in Infants - A Review for Providers. S D Med. 2020 May;73(5):223-227. | PubMed |
Blankespoor M, Ferrell K, Reuter A, Reuter S. Developmental Dysplasia of the Hip in Infants - A Review for Providers. S D Med. 2020 May;73(5):223-227. | PubMed | Gobierno de Chile, Ministerio de Salud. Guía Clínica displasia luxante de cadera: diagnóstico y tratamiento precoz. Santiago: Minsal, 2010. [On line]. | Link |
Gobierno de Chile, Ministerio de Salud. Guía Clínica displasia luxante de cadera: diagnóstico y tratamiento precoz. Santiago: Minsal, 2010. [On line]. | Link | Shorter D, Hong T, Osborn DA. Cochrane Review: Screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health. 2013 Jan;8(1):11-54. | CrossRef | PubMed |
Shorter D, Hong T, Osborn DA. Cochrane Review: Screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health. 2013 Jan;8(1):11-54. | CrossRef | PubMed | Schmitz MR, Murtha AS, Clohisy JC; ANCHOR Study Group. Developmental Dysplasia of the Hip in Adolescents and Young Adults. J Am Acad Orthop Surg. 2020 Feb 1;28(3):91-101. | CrossRef | PubMed |
Schmitz MR, Murtha AS, Clohisy JC; ANCHOR Study Group. Developmental Dysplasia of the Hip in Adolescents and Young Adults. J Am Acad Orthop Surg. 2020 Feb 1;28(3):91-101. | CrossRef | PubMed | Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005 Feb;87(2):254-9. | CrossRef | PubMed |
Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005 Feb;87(2):254-9. | CrossRef | PubMed | Jakobsen SS, Overgaard S, Søballe K, Ovesen O, Mygind-Klavsen B, Dippmann CA, et al. The interface between periacetabular osteotomy, hip arthroscopy and total hip arthroplasty in the young adult hip. EFORT Open Rev. 2018 Jul 11;3(7):408-417. | CrossRef | PubMed |
Jakobsen SS, Overgaard S, Søballe K, Ovesen O, Mygind-Klavsen B, Dippmann CA, et al. The interface between periacetabular osteotomy, hip arthroscopy and total hip arthroplasty in the young adult hip. EFORT Open Rev. 2018 Jul 11;3(7):408-417. | CrossRef | PubMed | Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009 Aug;467(8):2041-52. | CrossRef | PubMed |
Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009 Aug;467(8):2041-52. | CrossRef | PubMed | Nunley RM, Prather H, Hunt D, Schoenecker PL, Clohisy JC. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Joint Surg Am. 2011 May;93 Suppl 2:17-21. | CrossRef | PubMed |
Nunley RM, Prather H, Hunt D, Schoenecker PL, Clohisy JC. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Joint Surg Am. 2011 May;93 Suppl 2:17-21. | CrossRef | PubMed | Pascual-Garrido C, Harris MD, Clohisy JC. Innovations in Joint Preservation Procedures for the Dysplastic Hip "The Periacetabular Osteotomy". J Arthroplasty. 2017 Sep;32(9S):S32-S37. | CrossRef | PubMed |
Pascual-Garrido C, Harris MD, Clohisy JC. Innovations in Joint Preservation Procedures for the Dysplastic Hip "The Periacetabular Osteotomy". J Arthroplasty. 2017 Sep;32(9S):S32-S37. | CrossRef | PubMed | Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. 1988. Clin Orthop Relat Res. 2004 Jan;(418):3-8. | PubMed |
Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. 1988. Clin Orthop Relat Res. 2004 Jan;(418):3-8. | PubMed | Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008 Jul;466(7):1633-44. | CrossRef | PubMed |
Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008 Jul;466(7):1633-44. | CrossRef | PubMed | Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009 Sep;91(9):2113-23. | CrossRef | PubMed |
Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009 Sep;91(9):2113-23. | CrossRef | PubMed | Ross JR, Zaltz I, Nepple JJ, Schoenecker PL, Clohisy JC. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011 Jul;39 Suppl:72S-8S. | CrossRef | PubMed |
Ross JR, Zaltz I, Nepple JJ, Schoenecker PL, Clohisy JC. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011 Jul;39 Suppl:72S-8S. | CrossRef | PubMed | Redmond JM, Gupta A, Stake CE, Domb BG. The prevalence of hip labral and chondral lesions identified by method of detection during periacetabular osteotomy: arthroscopy versus arthrotomy. Arthroscopy. 2014 Mar;30(3):382-8. | CrossRef | PubMed |
Redmond JM, Gupta A, Stake CE, Domb BG. The prevalence of hip labral and chondral lesions identified by method of detection during periacetabular osteotomy: arthroscopy versus arthrotomy. Arthroscopy. 2014 Mar;30(3):382-8. | CrossRef | PubMed | Hartig-Andreasen C, Søballe K, Troelsen A. The role of the acetabular labrum in hip dysplasia. A literature overview. Acta Orthop. 2013 Feb;84(1):60-4. | CrossRef | PubMed |
Hartig-Andreasen C, Søballe K, Troelsen A. The role of the acetabular labrum in hip dysplasia. A literature overview. Acta Orthop. 2013 Feb;84(1):60-4. | CrossRef | PubMed | Adler KL, Giordano BD. The Utility of Hip Arthroscopy in the Setting of Acetabular Dysplasia: A Systematic Review. Arthroscopy. 2019 Jan;35(1):237-248. | CrossRef | PubMed |
Adler KL, Giordano BD. The Utility of Hip Arthroscopy in the Setting of Acetabular Dysplasia: A Systematic Review. Arthroscopy. 2019 Jan;35(1):237-248. | CrossRef | PubMed | Lodhia P, Chandrasekaran S, Gui C, Darwish N, Suarez-Ahedo C, Domb BG. Open and Arthroscopic Treatment of Adult Hip Dysplasia: A Systematic Review. Arthroscopy. 2016 Feb;32(2):374-83. | CrossRef | PubMed |
Lodhia P, Chandrasekaran S, Gui C, Darwish N, Suarez-Ahedo C, Domb BG. Open and Arthroscopic Treatment of Adult Hip Dysplasia: A Systematic Review. Arthroscopy. 2016 Feb;32(2):374-83. | CrossRef | PubMed | Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008 Nov;90 Suppl 4(Suppl 4):47-66. | CrossRef | PubMed |
Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008 Nov;90 Suppl 4(Suppl 4):47-66. | CrossRef | PubMed | Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007 Jun;188(6):1540-52. | CrossRef | PubMed |
Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007 Jun;188(6):1540-52. | CrossRef | PubMed | Ilizaliturri VM. Arthroscopic treatment of FAI: Position, portals, and instrumentation. In: Femoroacetabular Impingement. Springer-Verlag Berlin Heidelberg; 2012:99–111. | CrossRef |
Ilizaliturri VM. Arthroscopic treatment of FAI: Position, portals, and instrumentation. In: Femoroacetabular Impingement. Springer-Verlag Berlin Heidelberg; 2012:99–111. | CrossRef | Matsuda DK, Villamor A. The modified mid-anterior portal for hip arthroscopy. Arthrosc Tech. 2014 Jul 28;3(4):e469-74. | CrossRef | PubMed |
Matsuda DK, Villamor A. The modified mid-anterior portal for hip arthroscopy. Arthrosc Tech. 2014 Jul 28;3(4):e469-74. | CrossRef | PubMed | Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004 Jan;(418):67-73. | PubMed |
Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004 Jan;(418):67-73. | PubMed | Maldonado DR, LaReau JM, Lall AC, Battaglia MR, Mohr MR, Domb BG. Concomitant Arthroscopy With Labral Reconstruction and Periacetabular Osteotomy for Hip Dysplasia. Arthrosc Tech. 2018 Oct 15;7(11):e1141-e1147. | CrossRef | PubMed |
Maldonado DR, LaReau JM, Lall AC, Battaglia MR, Mohr MR, Domb BG. Concomitant Arthroscopy With Labral Reconstruction and Periacetabular Osteotomy for Hip Dysplasia. Arthrosc Tech. 2018 Oct 15;7(11):e1141-e1147. | CrossRef | PubMed | Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988 Dec;15(12):1833-40. | PubMed |
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988 Dec;15(12):1833-40. | PubMed | Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003 May 30;4:10. | CrossRef | PubMed |
Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003 May 30;4:10. | CrossRef | PubMed | Domb BG, Lareau JM, Baydoun H, Botser I, Millis MB, Yen YM. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res. 2014 Feb;472(2):674-80. | CrossRef | PubMed |
Domb BG, Lareau JM, Baydoun H, Botser I, Millis MB, Yen YM. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res. 2014 Feb;472(2):674-80. | CrossRef | PubMed | Fukui K, Briggs KK, Trindade CA, Philippon MJ. Outcomes After Labral Repair in Patients With Femoroacetabular Impingement and Borderline Dysplasia. Arthroscopy. 2015 Dec;31(12):2371-9. | CrossRef | PubMed |
Fukui K, Briggs KK, Trindade CA, Philippon MJ. Outcomes After Labral Repair in Patients With Femoroacetabular Impingement and Borderline Dysplasia. Arthroscopy. 2015 Dec;31(12):2371-9. | CrossRef | PubMed | Kuhns BD, Weber AE, Levy DM, Bedi A, Mather RC 3rd, Salata MJ, et al. Capsular Management in Hip Arthroscopy: An Anatomic, Biomechanical, and Technical Review. Front Surg. 2016 Mar 4;3:13. | CrossRef | PubMed |
Kuhns BD, Weber AE, Levy DM, Bedi A, Mather RC 3rd, Salata MJ, et al. Capsular Management in Hip Arthroscopy: An Anatomic, Biomechanical, and Technical Review. Front Surg. 2016 Mar 4;3:13. | CrossRef | PubMed | Bayne CO, Stanley R, Simon P, Espinoza-Orias A, Salata MJ, Bush-Joseph CA, et al. Effect of capsulotomy on hip stability-a consideration during hip arthroscopy. Am J Orthop (Belle Mead NJ). 2014 Apr;43(4):160-5. | PubMed |
Bayne CO, Stanley R, Simon P, Espinoza-Orias A, Salata MJ, Bush-Joseph CA, et al. Effect of capsulotomy on hip stability-a consideration during hip arthroscopy. Am J Orthop (Belle Mead NJ). 2014 Apr;43(4):160-5. | PubMed | Myers CA, Register BC, Lertwanich P, Ejnisman L, Pennington WW, Giphart JE, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011 Jul;39 Suppl:85S-91S. | CrossRef | PubMed |
Myers CA, Register BC, Lertwanich P, Ejnisman L, Pennington WW, Giphart JE, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011 Jul;39 Suppl:85S-91S. | CrossRef | PubMed | Kraeutler MJ, Goodrich JA, Fioravanti MJ, Garabekyan T, Mei-Dan O. The "Outside-In" Lesion of Hip Impingement and the "Inside-Out" Lesion of Hip Dysplasia: Two Distinct Patterns of Acetabular Chondral Injury. Am J Sports Med. 2019 Oct;47(12):2978-2984. | CrossRef | PubMed |
Kraeutler MJ, Goodrich JA, Fioravanti MJ, Garabekyan T, Mei-Dan O. The "Outside-In" Lesion of Hip Impingement and the "Inside-Out" Lesion of Hip Dysplasia: Two Distinct Patterns of Acetabular Chondral Injury. Am J Sports Med. 2019 Oct;47(12):2978-2984. | CrossRef | PubMed | Domb BG, El Bitar YF, Lindner D, Jackson TJ, Stake CE. Arthroscopic hip surgery with a microfracture procedure of the hip: clinical outcomes with two-year follow-up. Hip Int. 2014 Sep-Oct;24(5):448-56. | CrossRef | PubMed |
Domb BG, El Bitar YF, Lindner D, Jackson TJ, Stake CE. Arthroscopic hip surgery with a microfracture procedure of the hip: clinical outcomes with two-year follow-up. Hip Int. 2014 Sep-Oct;24(5):448-56. | CrossRef | PubMed | Domb BG, Redmond JM, Dunne KF, Stake CE, Gupta A. A matched-pair controlled study of microfracture of the hip with average 2-year follow-up: do full-thickness chondral defects portend an inferior prognosis in hip arthroscopy? Arthroscopy. 2015 Apr;31(4):628-34. | CrossRef | PubMed |
Domb BG, Redmond JM, Dunne KF, Stake CE, Gupta A. A matched-pair controlled study of microfracture of the hip with average 2-year follow-up: do full-thickness chondral defects portend an inferior prognosis in hip arthroscopy? Arthroscopy. 2015 Apr;31(4):628-34. | CrossRef | PubMed | Sansone M, Ahldén M, Jonasson P, Thomeé C, Swärd L, Collin D, et al. Outcome of hip arthroscopy in patients with mild to moderate osteoarthritis-A prospective study. J Hip Preserv Surg. 2015 Dec 26;3(1):61-7. | CrossRef | PubMed |
Sansone M, Ahldén M, Jonasson P, Thomeé C, Swärd L, Collin D, et al. Outcome of hip arthroscopy in patients with mild to moderate osteoarthritis-A prospective study. J Hip Preserv Surg. 2015 Dec 26;3(1):61-7. | CrossRef | PubMed | Más Martínez J, Sanz-Reig J, Verdú Román CM, Bustamante Suárez de Puga D, Morales Santías M, Martínez Giménez E. Arthroscopic hip surgery with a microfracture procedure of acetabular full-thickness chondral damage. Cohort study with a 3-year follow-up. Rev Esp Cir Ortop Traumatol. 2018 Mar 10:S1888-4415(18)30018-3. | CrossRef | PubMed |
Más Martínez J, Sanz-Reig J, Verdú Román CM, Bustamante Suárez de Puga D, Morales Santías M, Martínez Giménez E. Arthroscopic hip surgery with a microfracture procedure of acetabular full-thickness chondral damage. Cohort study with a 3-year follow-up. Rev Esp Cir Ortop Traumatol. 2018 Mar 10:S1888-4415(18)30018-3. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








