Key Words: Penetrating Eye Injuries, Eye Foreign Bodies, diagnostic imaging, tomography, Ultrasonography
Abstract
Background
Determining the precise location of intraocular foreign bodies is crucial for the management of patients with open-globe injury. Computed tomography is the most common method for detecting intraocular foreign bodies in the posterior segment. In this article, we describe three cases of open-globe injury with different types of intraocular foreign bodies in the posterior segment that were accurately located using computed tomography scans and B-scan ultrasonography.
Case presentation
Each of the three cases of open-globe injury described in this report had different types of ocular trauma, clinical symptoms, and intraocular foreign bodies. Computed tomography scans showed the exact location of the intraocular foreign bodies in the posterior segment in two of the three cases. A B-scan ultrasound was used to determine the location of a non-metallic intraocular foreign body in the third case. All three patients had intraocular foreign bodies, and one of them had an additional orbital foreign body. Case 1 had a perforating eye injury with the additional intraorbital foreign body; Cases 2 and Case 3 had different types of intraocular foreign bodies and prognoses. Various treatment approaches were used, ranging from observation to surgery, depending on the location of the intraocular foreign bodies, and all cases were successfully managed. These three cases show that proper use of various types of imaging tests is indispensable in the context of an intraocular foreign body related to open-globe injury.
Conclusion
Imaging techniques are crucial for the detection of an intraocular foreign body, and computed tomography is one of the simplest and most useful, especially in cases of open-globe injury.
Main message
|
Introduction
Open-globe injury usually results in serious visual loss and imposes a significant economic burden on the patient and society[1]. Intraocular foreign bodies are present in 18% to 40%[2] of all penetrating ocular injuries and often occur in the workplace, especially where hammers, chisels, or other tools are used, and in any context with metal striking metal. Most intraocular foreign bodies (88%) are found in the posterior segment of the eye[3]. The extent of ocular injury and visual prognosis depends on the size of the intraocular foreign body, the zone of the injury, and the ensuing complications; therefore, accurate localization of intraocular foreign bodies is essential for evaluating the severity of an ocular lesion and determining the best course of management[4],[5].
When the history of the mechanism of open-globe injury is typical, suspicion for an intraocular foreign body is high, even with lack of diagnostic evidence[6]. However, in some cases, despite meticulous examination, discovery of an intraocular foreign body may be difficult, because scleral manipulation and depression cannot be performed in an open globe. There are, however, many indirect signs of an intraocular foreign body, such as the presence of a scleral or corneal laceration with an iris defect, a focal cataract, or a vitreous track[7]. Use of imaging procedures can facilitate the diagnosis of the presence of an intraocular foreign body[8]. The most commonly used procedures for determining the location of intraocular foreign bodies are computed tomography, ultrasound biomicroscopy, and B-scan ultrasonography; the first method is considered the first-line imaging tool and the most sensitive one for characterizing ocular trauma in patients with a suspected intraocular foreign body[9]. Ultrasound biomicroscopy is also a valuable tool when the location is suspected to be in the anterior segment[10].
In this report, we present three cases with different mechanisms of open-globe injury and different types of intraocular foreign bodies in the posterior segment. Computed tomography scanning and B-scan ultrasonography were used to identify the exact location of the intraocular foreign bodies and determine the status of the posterior segment as well as the best approaches for further management.
Case 1
An 18-year-old male victim of a firearms attack presented at our clinic with a history of ocular trauma 5 weeks prior; he had experienced what he described as a gunshot assault in which a fired bullet apparently ricocheted off a rock nearby and struck his face and right eye. After the impact, he noted severe vision loss and went to a nearby hospital where he received topical and systemic treatment for his facial injuries. He denied having systemic disease or ocular surgery. At the time of our examination (five weeks later), he had a nonreactive left pupil, and his visual acuity was light perception. Intraocular pressure was 10 mm Hg in both eyes. Movement of both eyes was full and free. Slit-lamp examination showed subconjunctival fibrosis in the right eye on the superior nasal side (suspected scleral entrance wound) 3 mm from the limbus (zone II) and about 1 mm in length. The cornea was clear and there was no cell or flare in the anterior chamber. The lens was also clear but with some hematic impregnation of the posterior capsule. During indirect ophthalmoscopic examination, a dense vitreous hemorrhage that obscured fundus details was noted. B-scan ultrasonography (Figures 1A and 1B) revealed diffuse medium- to high-reflective opacities in the vitreous cavity of the right eye suggestive of an old vitreous hemorrhage, with an apparently flat retinal detachment near the optic disc and some high-reflective opacities with a mild acoustic shadow. An irregular area of the posterior wall suggesting a scleral rupture near the disc was also detected (Figures 1A and 1B). A perforating ocular injury with a retained intraocular foreign body in the right eye was diagnosed and immediate vitrectomy with phacoemulsification, intraocular lens implantation, and a 360° buckling procedure was performed. Intraoperatively, the entrance scleral wound was found at the 1 o’clock position (3 mm from the limbus, with a length of 2 mm). There was dense vitreous and preretinal hemorrhage. The full-thickness scleral exit wound was fibrotic, and there was an area of subretinal fibrosis next to it; both the exit wound and the fibrotic area were located on the nasal margin of the optic disc. The exit wound was at the corresponding location of the entrance wound, supporting the diagnosis of perforating globe injury. During vitrectomy, posterior vitreous detachment that was already present was completed, starting from the optic disc margin (the adherent cortical vitreous was carefully separated from the exit wound). Intraocular laser photocoagulation was performed around the exit wound and the subretinal fibrosis (Figure 1C). Cryopexy was applied over the entrance wound and silicone oil was used as a tamponade during the last phase of the procedure. An orbital computed tomography scan showed a high-density rounded foreign body (Figures 1D and 1E) next to the optic nerve of the right orbit and a small high-density lesion in the posterior wall of the globe (exit wound) that indicated the presence of an intrascleral foreign body. The intraorbital foreign body was managed conservatively due to its posterior location and the high risk of orbital and neurological complications from surgical removal. The patient's best-corrected visual acuity was 20/200 one week after the procedure and 20/100 at three-month follow-up.
Figure 1. Registry of open ocular trauma images case 1.
Case 2
A 33-year-old male presented at our clinic complaining of progressively blurred vision of the left eye, with stinging pain, after he had hammered an iron plate 2 hours earlier. He denied having systemic disease or ocular surgery. The initial best-corrected visual acuity in his left eye was 20/40. Intraocular pressure was 11 mm Hg in both eyes. Movement of both eyes was normal. Slit-lamp examination revealed a self-sealed corneal perforation (between the 12 and 2 o’clock positions; zone I) with an iris transillumination defect, and a lens opacity with posterior capsular involvement at that level (Figure 2A). During indirect ophthalmoscopic examination, central vitreous hemorrhage with a metallic intraocular foreign body (approximate length, 4.5 mm) in the temporal retina associated with a localized retinal detachment was noted (Figure 2B). An orbital computed tomography scan showed one high-density image on the temporal site of the globe with an approximate length of 4 mm (Figures 2D and 2E). A skull X-ray also confirmed the metallic foreign body on the temporal site of the orbit (Figure 2F). B-scan ultrasonography was not performed because the globe was open. A penetrating ocular injury with a retained metallic intraocular foreign body and a traumatic cataract in the left eye was diagnosed and immediate combined phaco-vitrectomy was performed. The cornea was repaired and a combined surgery with phacoemulsification, intraocular lens sulcus implantation, and 25-gauge pars plana vitrectomy with intraocular foreign body removal was performed. After cataract extraction with phacoemulsification, and sulcus implantation of a three-piece intraocular lens, the vitrectomy was performed and we found a central vitreous hemorrhage. Posterior vitreous detachment was not present and was therefore carried out starting from the optic disc margin (the adherent cortical vitreous was carefully separated from the site of the intraocular foreign body). The intraocular foreign body was located in the temporal retina (between the 2 and 5 o’clock positions) with a localized retinal detachment sparing the macula. Perfluorocarbon liquids were used to protect the macula and the metallic intraocular foreign body (Figure 2G) was successfully removed with forceps through the 4.0-mm corneal wound. Intraocular laser photocoagulation around the site where the intraocular foreign body was located (Figure 2C) and vitreous base shaving were performed. A silicone oil tamponade was used during the last phase of the surgery. The postoperative course with topical corticosteroid and antibiotic treatment was uneventful. The patient’s best-corrected visual acuity was 20/40 1 month after surgery, but 2 weeks later an inferior retinal detachment appeared; the detachment was successfully managed and a visual acuity of 20/200 was achieved at four-week follow-up.
Figure 2. Registry of open ocular trauma images case 2.
Case 3
A 32-year-old male presented at our clinic after a facial and eye injury caused by an explosion while handling a powder cartridge. He denied having systemic or ocular diseases. The initial best-corrected visual acuity was 20/20 in his left eye. His pupils were reactive and intraocular pressure was normal in both eyes. Movements of both eyes were normal. External examination showed multiple foreign bodies embedded in the facial skin, most densely on the left side. Slit-lamp examination of the left eye showed superficial and deep stromal foreign bodies all over the cornea. The anterior chamber was unaffected, and the lens was clear. The temporal conjunctiva showed multiples foreign bodies with some tissue scarring (Figure 3A). A dilated funduscopic examination showed a small and mobile foreign body in the vitreous cavity and no signs of inflammation, trauma to the optic disc, macula, or retinal periphery (Figures 3B and 3E). Computed tomography scanning did not reveal the intraocular foreign body clearly (Figure 3D) but B-scan ultrasonography showed a free-floating intraocular foreign body in the vitreous cavity (Figure 3C). Due to the fact that we didn’t see any signs of inflammation or infection, the suspected entrance (temporal site; zone II) wound was sealed, and the patient had excellent visual acuity (20/20), we did not perform any other procedures but maintained close observation of this patient in follow-up (Figure 3E).
Figure 3. Registry of open ocular trauma images case 3.
Discussion
This report describes three cases with different mechanisms of ocular trauma, times of presentation, types of foreign bodies, prognoses, and management. All three patients had intraocular foreign bodies, and one of them had an additional orbital foreign body. The three different types of ocular trauma were firearm injury (Case 1); metal projectile injury (from hammering) (Case 2); and blast injury (from a small powder explosive) (Case 3). Each case had a different prognosis and required a different management approach. Case 1, who presented more than one month after the ocular trauma, had minimal ocular involvement with a small amount of scar tissue in the sclera (zone II), no corneal laceration, and vitreous hemorrhage, with poor initial visual acuity (light perception), and ended up with very good vision (20/100). This patient also had a foreign body located in the posterior orbit next to the optic nerve, clearly demarcated by computed tomography scans, that was conservatively managed due to high risk of orbital and neurological complications from surgical removal[11]. Case 2 presented immediately after the ocular trauma, and had a self-sealed corneal laceration (zone I) with a metallic intraocular foreign body, central vitreous hemorrhage, and good vision (20/40), but eventually had a retinal detachment, which was managed with a second surgery. This patient ended up with 20/100 vision. Case 3 had a different type of intraocular foreign body (non-metallic) with a different evolution and prognosis, with minimal ocular involvement (small amount of scleral scar tissue, zone II) and good visual acuity that remained stable through follow-up. None of the three patients presented endophthalmitis (Tables 1 and 2).
Table 1. Summary of three cases with intraocular foreign bodies in the posterior segment.
Table 2. Comparative images of three cases with intraocular foreign bodies in the posterior segment.
The three cases reported above illustrate a variety of open-globe injury presentations and prognoses. In the section below, we provide an overview of various types of intraocular foreign bodies related to open-globe injury, including characteristics, composition, and frequency; available imaging tests and strategies for identifying, locating and managing them, by type and composition; and important aspects to consider with regard to surgical intervention, including timing and approach.
Various types of intraocular foreign bodies, imaging tests, and management strategies
The presence of intraocular foreign bodies following penetrating globe injury is very common and can cause severe complications, including cataract, glaucoma, uveitis, retinal detachment, and endophthalmitis[12]. Although the nature of the injury and the foreign object can often be elicited from a detailed patient history, the severity of the injury could be underestimated[13]. Therefore, a meticulous examination and radiological investigation should be performed. Traditionally, open-globe injuries were subdivided into penetrating injuries (presence of an entrance wound), perforating injuries (presence of an entrance and exit wound), lacerations, and blunt ruptures, with or without a retained intraocular foreign body. According to the Ocular Trauma Classification Group[14], entry sites of open-globe injuries should be categorized according to the location of the most posterior wound (zone I, for cornea; zone II, for sclera, up to 5 mm posterior to the corneoscleral limbus; and zone III, for sclera, more than 5 mm posterior to the corneoscleral limbus)[14]. The presence of an intraocular foreign body does not always entail significant intraocular damage outside of its entry site in the eye, but it is usually associated with massive internal damage in any or all compartments of the globe. Intraocular foreign bodies have been classified according to their location (anterior or posterior segment), material characteristics (metallic, magnetic, wood), size, mechanism of injury, setting (work-related, battlefield), and duration (acute, longstanding)[14]. Injuries related to intraocular foreign bodies can be the result of direct trauma through a mechanism of penetration/perforation through the cornea, in the majority of cases (65%), the sclera (25%), or the limbus (10%)[5],[15]. In most cases the foreign bodies enter the posterior segment (5% to 88%), with 10% to 15% remaining in the anterior chamber and 2% to 8% remaining in the lens[7],[16]. These data are compatible with our three cases, which all had foreign bodies in the posterior segment and a scleral entrance site (zone II); only one case also had entry of the foreign body in the peripheral cornea (zone I).
Kuhn et al. showed that, in penetrating injuries, multiple intraocular foreign bodies can be found in 8% to 25% of all cases, with an average size of 3.5 mm (0.5 to 25 mm)[17].
Intraocular foreign body composition varies from organic material (e.g., insect parts and animal hairs) to glass, plastic, or metal, such as zinc, nickel, aluminum, mercury, iron, and copper[3]. Broadly speaking, intraocular foreign bodies can be divided into metallic or non-metallic material, with different implications for each in terms of the modality of diagnosis, risk of infection, and long-term visual prognosis. Metallic intraocular foreign bodies comprise 55% to 91% of all foreign bodies[3],[18],[19] and are associated with less risk for endophthalmitis compared to organic material[20] but may cause complications related to intraocular toxicity that can lead to acute and chronic visual loss (from copper and iron foreign bodies respectively)[21].
Common types of non-metallic foreign bodies include wood, stone, concrete, glass, and plastic. Glass and plastic are considered inert and are therefore generally well-tolerated in the eye, but because both materials (and many other non-metallic organic foreign bodies) are commonly found in an outdoor setting, such as landscaping or gardening (e.g., wood), they carry a higher risk of infection[3],[7],[20]. Glass intraocular foreign bodies are less common than other types of intraocular foreign bodies, representing only 2.8% to 17.6 %[3],[18],[22]; the most common cause of this type of ocular trauma is a motor vehicle accident[5].
In the management of all types of intraocular foreign bodies, ocular imaging is crucial. B-scan ultrasonography, plain X-ray, computed tomography, and magnetic resonance imaging are the methods most commonly used in clinical practice. Selection of the most appropriate imaging test depends on the suspected composition of the foreign body and its location in the eye.
Plain X-rays have been used as a screening test for the presence of foreign bodies in the eye and orbit for a long time; this method has 70% to 90% sensitivity for radiopaque fragments[23] but only 0% to 40% sensitivity for radiolucent particles (plastic, wood)[24],[25]; therefore, some foreign bodies can be missed with the use of this method. On the other hand, in some cases, X-rays can reveal the presence of multiple intraocular foreign bodies better than computed tomography scans as thin cuts used in the latter method may miss small foreign bodies (< 0.5 mm)[23],[26]. Nonetheless, the inaccuracy of X-rays in detecting some intraocular foreign bodies makes this detection method debatable as an initial approach despite its wide availability and simplicity of use.
Computed tomography scanning of the orbits without contrast is the preferred method for cases of open-globe injury because it allows for examination of orbital and facial bones, the retrobulbar space, and both globes at the same time[6],[9]. Thin axial and coronal views of 1.0- to 1.5-mm cuts of the orbit are very useful for delineating the shape and composition of the foreign body[27]. The composition of the foreign bodies can be determined by measuring their Hounsfield unit[28]. This noninvasive test is preferred because it can detect up to 100% of metallic intraocular foreign bodies greater than 0.05 mm3[6],[29], requires little patient cooperation, and does not lead to globe manipulation[21]. The minimum detectable size varies by the composition of the foreign body (0.06 mm3 for steel and copper and 1.5 to 1.8 mm3 for aluminum/car window glass; wood in small pieces will most likely not be detectable unless it is coated with lead-containing paint)[30],[31].
Conventional and helical/spiral scanning are the types of computed tomography used most frequently in open-globe injury cases. Conventional scanning is more common due to its widespread availability. Helical computed tomography allows for better evaluation of intraocular metallic, stone, and glass foreign bodies[32]; other benefits of this method compared to conventional tomography are decreased examination time, less radiation exposure, better multiplanar reconstruction, and reduced motion artifacts[21],[33]. Helical tomography is more sensitive than axial computed tomography, magnetic resonance, and B-scan ultrasonography in detecting glass foreign bodies[34]. Nevertheless, some intraocular foreign bodies, such as ceramic, plastic, and wood, may be missed using computed tomography[35]. In Case 3 reported above, for example, due to the nature of the foreign body, computed tomography was not very useful.
B-scan ultrasonography should be used when a foreign body cannot be visualized directly, or with a computed tomography scan (e.g., glass, plastic), and can be up to 98% sensitive detecting foreign bodies with concurrent vitreous hemorrhage or retinal detachment[21],[36],[37]. Use of a B-scan has several advantages, including its high resolution (0.01 to 0.1 mm), quick generation of multiple cross-sections, and low cost, making it one of the most commonly used tests, but it must be performed extremely carefully in eyes with open-globe injury because the pressure of the probe on the eye poses a risk of contamination or extrusion of globe material[35],[38]. In Case 2, for example, we decided not to carry out the ultrasound study because of the risk of doing so in an open globe. In addition, an expert operator (someone who can distinguish artifacts from foreign bodies) is required for use of this method[39]. The inherent challenges with regard to visibility are illustrated in Case 1, in which the presence of the dense vitreous hemorrhage did not allow for identification of the foreign body. In Case 3, however, ultrasound showed a greater utility than other methods in identifying the non-metallic composition of the foreign body.
Magnetic resonance imaging is not routinely used to detect intraocular foreign bodies, despite its greater sensitivity and soft tissue resolution, but may be useful for detecting radiolucent foreign bodies[40]. When the type of foreign body is unknown, magnetic resonance as the initial imaging test is contradicted due to the potential danger of further tissue damage from possible movement of a metallic foreign body within the magnetic field, and is therefore utilized only when the presence of a metallic foreign body is ruled out. However, some metals, such as platinum, titanium, and tantalum, are compatible with this technology[41],[42],[43]. In addition, some tiny (< 0.5 mm) ferromagnetic bodies can only be detected by magnetic resonance without causing ocular damage[44]. Moisseiev et al.[45], who developed an algorithm, reported that magnetic resonance was superior to computed tomography for accurate detection of type of foreign body; these and other results strongly suggest the use of magnetic resonance imaging once the presence of a metallic foreign body has been ruled out by computed tomography[8],[45],[46].
Metallic intraocular foreign bodies are usually identified and located using computed tomography scanning. This method can detect small metal foreign bodies (> 0.07 mm3), which appear as hyperdense images in up to 100% of cases[21]. In B-scans they appear as echo-dense signals with marked shadowing posterior to the foreign body and may be surrounded by fibrous tissue[8],[47]. The reported sensitivity of B-scans for detecting metallic foreign bodies is up to 87%[21],[48]. The composition of metallic foreign bodies is difficult to determine using ultrasound; however, it has been observed that type of artifact was related to type of metal, with aluminum corresponding to a localized and narrow artifact ("lantern") and lead corresponding to a broad and dense one ("lighthouse")[21]. Computed tomography is usually preferred when the nature of the intraocular foreign body is unknown, regardless of whether the latter is metallic or not. If the result of computed tomography is not conclusive or appears to be negative despite high clinical suspicion of an intraocular foreign body, magnetic resonance and B-scan ultrasound imaging may be useful in ruling out a foreign body[45].
Non-metallic intraocular foreign bodies such as wood can be seen as areas of either hypodensity or linear/cylindrical hyperdensity in computed tomography[21]; this inconsistency is related to the water content in the wood fragments[31]. In addition, in both computed tomography and magnetic resonance, wood may resemble air, appearing hypodense and hypointense in CT scans and T2-weighted MRIs respectively[13],[46]. The geometric shape of the foreign body (e.g., oblong or elongated) may aid in the diagnosis and distinguish wood from air[31]. It has been reported that computed tomography has up to 90% sensitivity in detecting wood[48]. In magnetic resonance imaging, dry wood has low intensity (using both T1- and T2-weighted MRIs) due to its high air content, but as it hydrates in the globe (7 to 10 days) it appears as a hyperintense ring (in T1-weighted MRI sequences)[21]. In B-scan ultrasound, organic foreign bodies (sensitivity of 91%) appear highly reflective / hyperechogenic compared to surrounding tissue[39],[46],[49]. Images of wood material can present with echoes of medium echogenicity and may resemble blood or vitritis[8]. Sharp edges, as seen in Case 2 reported above, can also suggest the presence of a non-metallic foreign body, such as wood, in the vitreous cavity[38]. Some studies recommend the use of magnetic resonance and ultrasound to detect non-metallic foreign bodies, such as wood, once any metallic nature has been ruled out[21],[45]. Drywall is another non-metallic foreign body that has been reported to appear as a hyperdense image in computed tomography because of its calcium content[50].
Glass foreign bodies are best viewed with computed tomography (which has 96% sensitivity) and appear as hyperdense images without artifacts[22],[34]; however, this type of foreign body can produce different attenuation signals, depending on the type of glass. For example, green beer bottle glass is easier to detect than spectacle glass material, probably due to the different composition of these two types of glass[34]. In magnetic resonance imaging, glass appears as a hypointense image (in T2-weighted MRIs)[8],[31] with low detection rates (11.1% and 4.8% using T1 and T2-weighted MRIs respectively)[34], depending on the size of the fragments and the composition of the glass. Reported sensitivity of B-scan ultrasound in detecting glass ranges from 24% to 90%, with glass foreign bodies appearing as hyperechogenic images; however, due to the double-reflective and refractive nature of glass, it can generate an acoustic shadow, or a reverberance artifact, with the characteristics of the latter effect depending on the type of glass; for example, bottle glass tends to have “hard” (well-defined) reverberations, similar to steel, and windshield glass[21],[37]. Rong et al. recommend the use of helical tomography as the first-line modality for detecting glass foreign bodies[21].
Plastic intraocular foreign bodies, in computed tomography, can have a wide range of features depending on the material, with some types showing up as hyperdense (e.g., polyvinyl chloride), or isodense (plastic spectacle glass); in magnetic resonance, on the other hand, plastic appears as a significant signal void, without artifacts (in both T1- and T2-weighted MRIs)[21]. B-scan ultrasound shows these foreign bodies as images with low echogenicity with reverberations and has 90% of sensitivity in detecting them[37],[48]. Information about plastic foreign bodies is limited by the lack of data. Plastic is difficult to detect using computed tomography, but helical tomography, along with ultrasound, are the most recommended for these types of foreign bodies[21].
Of all of the imaging methods described above, computed tomography is generally accepted as the standard procedure and is recommended as the initial diagnostic test for the detection of metallic, glass, or plastic intraocular foreign bodies. If it is suspected that the foreign body is made of wood, and any metallic nature has been ruled out, magnetic resonance imaging and/or ultrasound should be considered.
Aspects to consider regarding surgery: timing and approach
As shown in the three cases reported above, which differed in time between ocular trauma and patient presentation for care, there are several different aspects to consider with regard to surgical intervention in managing an open-globe injury. The timing of the surgery is crucial and depends on several factors: the patient’s general health status (e.g., the presence or absence of life-threatening injuries), the nature of the injury (e.g., heat-sterilized projectiles are probably less likely to induce infection than farm injuries), and the composition of the foreign body (e.g., copper material can induce a severe inflammatory response, whereas glass tends to be inert and therefore well-tolerated)[5],[51].
The reported incidence of endophthalmitis related to intraocular foreign bodies is 16.7%, which explains the standard recommendation of immediate globe repair with administration of intravitreal antibiotics and intraocular foreign body removal[7],[52]. However, delayed intraocular foreign body removal may be performed in some circumstances (e.g., unavailability of a retinal surgeon)[52]. Immediate foreign body removal decreases the risk of endophthalmitis and the rate of proliferative vitreoretinopathy[29]. Some studies indicate that delayed repair of the globe (> 24 hours) and intraocular foreign body removal were a predictive factor for developing endophthalmitis[16],[53]. On the other hand, some researchers found that the timing of intraocular foreign body removal was not a significant factor in the development of endophthalmitis; they attribute this finding to several factors like : immediate closure of the globe (within hours of the injury), prompt administration of broad-spectrum antibiotics, and the type of foreign body (high-speed metallic objects are most likely self-sterilized, versus non-metallic foreign bodies such as stone that may not be self-sterilized and therefore could have posed a higher risk of infection)[5],[54].
The advantages of delaying intraocular foreign body removal include improved control of inflammation and better manipulation of intraocular structures; it also allows for the development of spontaneous posterior vitreous detachment, which facilitates posterior hyaloid removal[6]. However, leaving a potentially contaminated foreign body in the eye increases the risk of infection[7].
Intraorbital foreign bodies located posteriorly have an increased risk of motility alterations and/or optic neuropathy after surgical removal; anteriorly located foreign bodies are more easily removed[11].
When the foreign body causes an ocular complication, or has an organic composition, surgery is indicated; if is not or is anteriorly located, surgical options and decisions about whether or not to remove the foreign body can be discussed with the patient[55]. In Case 1 reported above, the intraorbital foreign body was posteriorly located and did not interfere with extraocular muscles but was near the optic nerve and was therefore managed conservatively. Surgical removal is indicated when a foreign body causes orbital complications (mechanical restriction of ocular movements, neurological compromise, inflammation) or infection[56].
Conclusion
Accurate and timely determination of an intraocular foreign body is important in all cases of open-globe injuries. The type of foreign body, mechanism of trauma, and time between trauma and patient presentation at a health facility are very important factors in the prognosis, given the potential for good visual recovery with an adequate surgical treatment. Understanding the limits in the detection of each type of foreign body and the respective imaging modality that is used, as well as the characteristics of the different intraocular foreign bodies, is of utmost importance to optimize the management of patients with ocular trauma.
The general guidelines below could be used to identify intraocular foreign bodies in a patient with open-globe injury. We believe the most practical first step in the evaluation of an intraocular foreign body, in addition to obtaining an adequate medical history, is a computed tomography scan; magnetic resonance imaging and B-scan ocular ultrasonography could be reserved for use as complementary tests.
It is reasonable to suggest B-scan ocular ultrasonography as an initial imaging method in some cases due to its low cost and excellent sensitivity, as well as the lack of radiation exposure, taking into account the added risk from manipulating an open globe with this method. Due to this risk, it is usually recommended that use of a B-scan be delayed until after the globe closure. Computed tomography scanning is the most practical initial imaging strategy in a open globe injury scenario.
The use of magnetic resonance imaging could be considered in cases with high clinical suspicion of an intraocular foreign body that is not detected by computed tomography, even in patients with a complicated postoperative course after the closure of the eyeball.
Plain X-rays have little value in the detection of intraocular foreign bodies because negative results from this method are not reliable and positive results often require a more detailed examination.
Our current understanding of the various imaging modalities available for detecting intraocular foreign bodies, summarized here, allows for the detection and effective characterization of the different types of intraocular foreign bodies we see in our clinical practice.
Notes
Authorship contributions
DV, MG, PR, YV, VR, RG: Conceptualization, methodology, formal analysis, research, writing (proofreading and edition), visualization, supervision, project management. All authors attest that they meet the current ICMJE criteria for authorship.
Conflicts of interests
The authors declare that they have no conflicts of interest involving this work.
Funding
The authors declare that there were no external sources of funding.
Ethics
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for the diagnostic images and other clinical information to be reported in this journal article. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity but anonymity cannot be guaranteed.
Acknowledgments
We gratefully thank the patients for their participation in this study.
Note from the editors
The original version of this manuscript was submitted in Spanish. The English translation was copyedited by the journal.

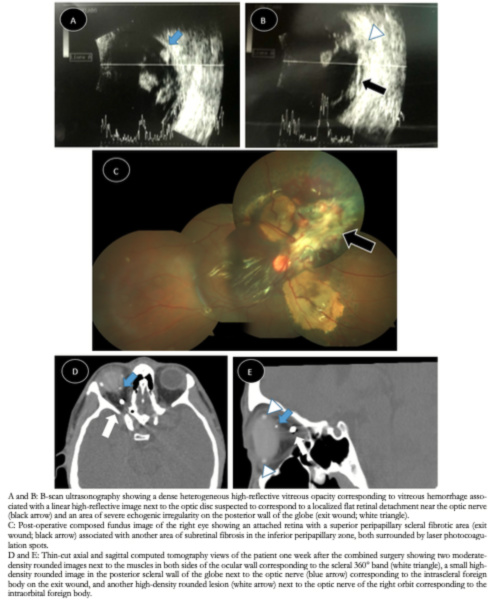 Figure 1. Registry of open ocular trauma images case 1.
Figure 1. Registry of open ocular trauma images case 1.

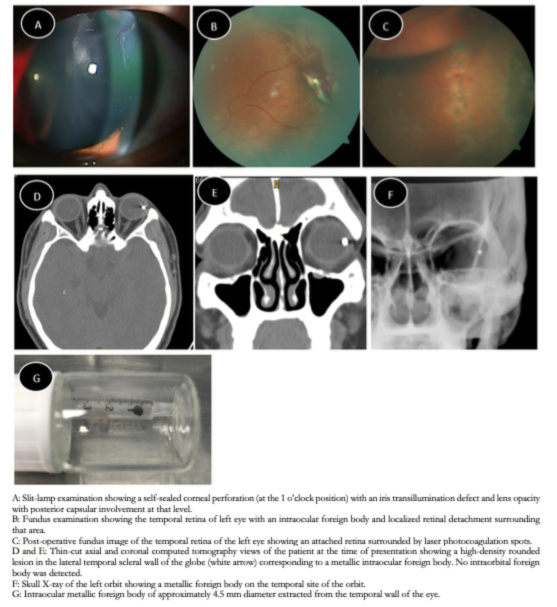 Figure 2. Registry of open ocular trauma images case 2.
Figure 2. Registry of open ocular trauma images case 2.

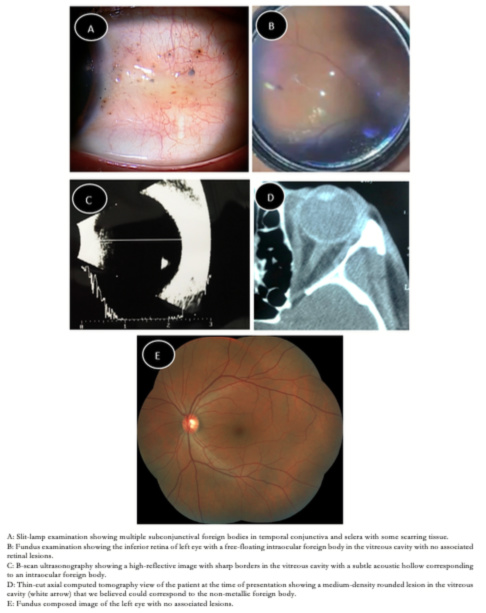 Figure 3. Registry of open ocular trauma images case 3.
Figure 3. Registry of open ocular trauma images case 3.

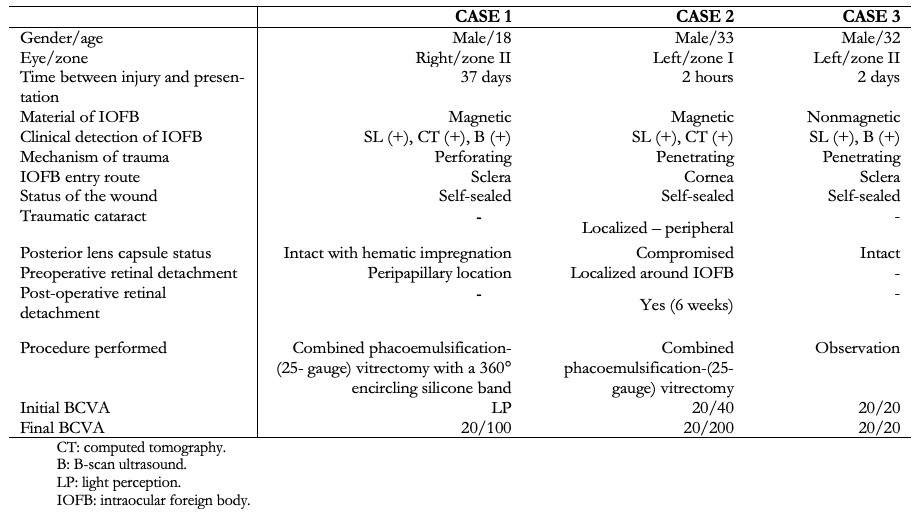 Table 1. Summary of three cases with intraocular foreign bodies in the posterior segment.
Table 1. Summary of three cases with intraocular foreign bodies in the posterior segment.

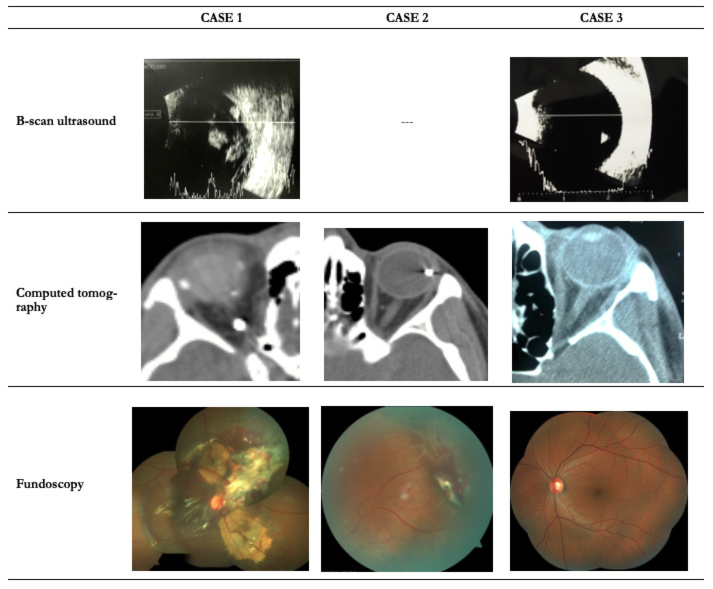 Table 2. Comparative images of three cases with intraocular foreign bodies in the posterior segment.
Table 2. Comparative images of three cases with intraocular foreign bodies in the posterior segment.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Background
Determining the precise location of intraocular foreign bodies is crucial for the management of patients with open-globe injury. Computed tomography is the most common method for detecting intraocular foreign bodies in the posterior segment. In this article, we describe three cases of open-globe injury with different types of intraocular foreign bodies in the posterior segment that were accurately located using computed tomography scans and B-scan ultrasonography.
Case presentation
Each of the three cases of open-globe injury described in this report had different types of ocular trauma, clinical symptoms, and intraocular foreign bodies. Computed tomography scans showed the exact location of the intraocular foreign bodies in the posterior segment in two of the three cases. A B-scan ultrasound was used to determine the location of a non-metallic intraocular foreign body in the third case. All three patients had intraocular foreign bodies, and one of them had an additional orbital foreign body. Case 1 had a perforating eye injury with the additional intraorbital foreign body; Cases 2 and Case 3 had different types of intraocular foreign bodies and prognoses. Various treatment approaches were used, ranging from observation to surgery, depending on the location of the intraocular foreign bodies, and all cases were successfully managed. These three cases show that proper use of various types of imaging tests is indispensable in the context of an intraocular foreign body related to open-globe injury.
Conclusion
Imaging techniques are crucial for the detection of an intraocular foreign body, and computed tomography is one of the simplest and most useful, especially in cases of open-globe injury.
 Authors:
Diego Valera-Cornejo[1,2], Marlon García-Roa[1,2], Paulina Ramírez-Neria[1,2], Yolanda Villalpando-Gómez[1,2], Verónica Romero-Morales[1,2], Renata García-Franco[1,2]
Authors:
Diego Valera-Cornejo[1,2], Marlon García-Roa[1,2], Paulina Ramírez-Neria[1,2], Yolanda Villalpando-Gómez[1,2], Verónica Romero-Morales[1,2], Renata García-Franco[1,2]
Affiliation:
[1] Servicio de Retina del Instituto Mexicano de Oftalmología I.A.P, Querétaro, México
[2] Universidad Nacional Autónoma de México, Ciudad de México, México
E-mail: drmgroa@hotmail.com
Author address:
[1] Instituto Mexicano de Oftalmología I.A.P. Colinas de Cimatario Avenida Estadio Sn Centro Sur 76090 Santiago de Querétaro Qro.

Citation: Valera-Cornejo D, García-Roa M, Ramírez-Neria P, Villalpando-Gómez Y, Romero-Morales V, García-Franco R. The role of various imaging techniques in identifying and locating intraocular foreign bodies related to open-globe injury: three case reports and literature review. Medwave 2020;20(1):e7773 doi: 10.5867/medwave.2020.01.7773
Submission date: 6/9/2019
Acceptance date: 7/1/2020
Publication date: 28/1/2020
Origin: Not commissioned.
Type of review: Externally peer-reviewed by three peer reviewers, double blind.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Beshay N, Keay L, Dunn H, Kamalden TA, Hoskin AK, Watson SL. The epidemiology of Open Globe Injuries presenting to a tertiary referral eye hospital in Australia. Injury. 2017 Jul;48(7):1348-1354. | CrossRef | PubMed |
- Mester V, Kuhn F. Intraocular foreign bodies. Ophthalmol Clin North Am. 2002 Jun;15(2):235-42. | CrossRef | PubMed |
- Zhang Y, Zhang M, Jiang C, Qiu HY. Intraocular foreign bodies in china: clinical characteristics, prognostic factors, and visual outcomes in 1,421 eyes. Am J Ophthalmol. 2011 Jul;152(1):66-73.e1. | CrossRef | PubMed |
- Yaşa D, Erdem ZG, Demircan A, Demir G, Alkın Z. Prognostic value of ocular trauma score for open globe injuries associated with metallic intraocular foreign bodies. BMC Ophthalmol. 2018 Aug 9;18(1):194. | CrossRef | PubMed |
- Sharma S, Thapa R, Bajimaya S, Pradhan E, Poudyal G. Clinical characteristics and visual outcome, prognostic factor, visual acuity and globe survival in posterior segment intraocular foreign body at Tilganga Institute of Ophthalmology. Nepal J Ophthalmol. 2018 Jan;10(19):66-72. | CrossRef | PubMed |
- Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: A review. Surv Ophthalmol. 2016 Sep-Oct;61(5):582-96. | CrossRef | PubMed |
- Duan F, Yuan Z, Liao J, Zheng Y, Yang Y, Lin X. Incidence and Risk Factors of Intraocular Foreign Body-Related Endophthalmitis in Southern China. J Ophthalmol. 2018 Sep 30;2018:8959108. | CrossRef | PubMed |
- Modjtahedi BS, Rong A, Bobinski M, McGahan J, Morse LS. Imaging characteristics of intraocular foreign bodies: a comparative study of plain film X-ray, computed tomography, ultrasound, and magnetic resonance imaging. Retina. 2015 Jan;35(1):95-104. | CrossRef | PubMed |
- Lin TC, Liao TC, Yuan WH, Lee FL, Chen SJ. Management and clinical outcomes of intraocular foreign bodies with the aid of orbital computed tomography. J Chin Med Assoc. 2014 Aug;77(8):433-6. | CrossRef | PubMed |
- Kaushik S, Ichhpujani P, Ramasubramanian A, Pandav SS. Occult intraocular foreign body: ultrasound biomicroscopy holds the key. Int Ophthalmol. 2008 Feb;28(1):71-3. | CrossRef | PubMed |
- Siedlecki AN, Tsui E, Deng J, Miller DM. Long-Term Retention of an Intraorbital Metallic Foreign Body Adjacent to the Optic Nerve. Case Rep Ophthalmol Med. 2016;2016:3918592. | CrossRef | PubMed |
- Parke DW 3rd, Flynn HW Jr, Fisher YL. Management of intraocular foreign bodies: a clinical flight plan. Can J Ophthalmol. 2013 Feb;48(1):8-12. | CrossRef | PubMed |
- Ho VT, McGuckin JF Jr, Smergel EM. Intraorbital wooden foreign body: CT and MR appearance. AJNR Am J Neuroradiol. 1996 Jan;17(1):134-6. | PubMed |
- Pieramici DJ, Sternberg P Jr, Aaberg TM Sr, Bridges WZ Jr, Capone A Jr, Cardillo JA, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997 Jun;123(6):820-31. | CrossRef | PubMed |
- Williams DF, Mieler WF, Abrams GW, Lewis H. Results and prognostic factors in penetrating ocular injuries with retained intraocular foreign bodies. Ophthalmology. 1988 Jul;95(7):911-6. | CrossRef | PubMed |
- Jonas JB, Knorr HL, Budde WM. Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology. 2000 May;107(5):823-8. | CrossRef | PubMed |
- Kuhn F, Morris R, Witherspoon CD, Mann L. Epidemiology of blinding trauma in the United States Eye Injury Registry. Ophthalmic Epidemiol. 2006 Jun;13(3):209-16. | CrossRef | PubMed |
- Woodcock MG, Scott RA, Huntbach J, Kirkby GR. Mass and shape as factors in intraocular foreign body injuries. Ophthalmology. 2006 Dec;113(12):2262-9. | CrossRef | PubMed |
- Ehlers JP, Kunimoto DY, Ittoop S, Maguire JI, Ho AC, Regillo CD. Metallic intraocular foreign bodies: characteristics, interventions, and prognostic factors for visual outcome and globe survival. Am J Ophthalmol. 2008 Sep;146(3):427-433. | CrossRef | PubMed |
- Bhagat N, Nagori S, Zarbin M. Post-traumatic Infectious Endophthalmitis. Surv Ophthalmol. 2011 May-Jun;56(3):214-51. | CrossRef | PubMed |
- Patel SN, Langer PD, Zarbin MA, Bhagat N. Diagnostic value of clinical examination and radiographic imaging in identification of intraocular foreign bodies in open globe injury. Eur J Ophthalmol. 2012 Mar-Apr;22(2):259-68. | CrossRef | PubMed |
- Saeed A, Cassidy L, Malone DE, Beatty S. Plain X-ray and computed tomography of the orbit in cases and suspected cases of intraocular foreign body. Eye (Lond). 2008 Nov;22(11):1373-7. | CrossRef | PubMed |
- de Santana Santos T, Avelar RL, Melo AR, de Moraes HH, Dourado E. Current approach in the management of patients with foreign bodies in the maxillofacial region. J Oral Maxillofac Surg. 2011 Sep;69(9):2376-82. | CrossRef | PubMed |
- Bray LC, Griffiths PG. The value of plain radiography in suspected intraocular foreign body. Eye (Lond). 1991;5 ( Pt 6):751-4. | CrossRef | PubMed |
- McElvanney AM, Fielder AR. Intraocular foreign body missed by radiography. BMJ. 1993 Apr 17;306(6884):1060-1. | CrossRef | PubMed |
- Winegar BA, Gutierrez JE. Imaging of Orbital Trauma and Emergent Non-traumatic Conditions. Neuroimaging Clin N Am. 2015 Aug;25(3):439-56. | CrossRef | PubMed |
- Lagalla R, Manfrè L, Caronia A, Bencivinni F, Duranti C, Ponte F. Plain film, CT and MRI sensibility in the evaluation of intraorbital foreign bodies in an in vitro model of the orbit and in pig eyes. Eur Radiol. 2000;10(8):1338-41. | CrossRef | PubMed |
- Chacko JG, Figueroa RE, Johnson MH, Marcus DM, Brooks SE. Detection and localization of steel intraocular foreign bodies using computed tomography. A comparison of helical and conventional axial scanning. Ophthalmology. 1997 Feb;104(2):319-23. | CrossRef | PubMed |
- Rong AJ, Fan KC, Golshani B, Bobinski M, McGahan JP, Eliott D, et al. Multimodal imaging features of intraocular foreign bodies. Semin Ophthalmol. 2019;34(7-8):518-532. | CrossRef | PubMed |
- Tate E, Cupples H. Detection of orbital foreign bodies with computed tomography: current limits. AJR Am J Roentgenol. 1981 Sep;137(3):493-5. | CrossRef | PubMed |
- Javadrashid R, Golamian M, Shahrzad M, Hajalioghli P, Shahmorady Z, Fouladi DF, et al. Visibility of Different Intraorbital Foreign Bodies Using Plain Radiography, Computed Tomography, Magnetic Resonance Imaging, and Cone-Beam Computed Tomography: An In Vitro Study. Can Assoc Radiol J. 2017 May;68(2):194-201. | CrossRef | PubMed |
- Lakits A, Prokesch R, Scholda C, Bankier A. Orbital helical computed tomography in the diagnosis and management of eye trauma. Ophthalmology. 1999 Dec;106(12):2330-5. | CrossRef | PubMed |
- Prokesch R, Lakits A, Scholda C, Bankier A, Ba-Ssalamah A, Imhof H. [Spiral CT and conventional CT in the preoperative imaging of intraocular metal foreign bodies]. Radiologe. 1998 Aug;38(8):667-73. | CrossRef | PubMed |
- Gor DM, Kirsch CF, Leen J, Turbin R, Von Hagen S. Radiologic differentiation of intraocular glass: evaluation of imaging techniques, glass types, size, and effect of intraocular hemorrhage. AJR Am J Roentgenol. 2001 Nov;177(5):1199-203. | CrossRef | PubMed |
- Lit ES, Young LH. Anterior and posterior segment intraocular foreign bodies. Int Ophthalmol Clin. 2002 Summer;42(3):107-20. | CrossRef | PubMed |
- Wickham L, Xing W, Bunce C, Sullivan P. Outcomes of surgery for posterior segment intraocular foreign bodies--a retrospective review of 17 years of clinical experience. Graefes Arch Clin Exp Ophthalmol. 2006 Dec;244(12):1620-6. | CrossRef | PubMed |
- Costa MA, Garcia PN, Barroso LF, Ferreira MA, Okuda ÉA, Allemann N. Composition of intraocular foreign bodies: experimental study of ultrasonographic presentation. Arq Bras Oftalmol. 2013 Jan-Feb;76(1):13-7. | CrossRef | PubMed |
- Zacks DN, Hart L, Young LH. Ultrasonography in the traumatized eye: intraocular foreign body versus artifact. Int Ophthalmol Clin. 2002 Summer;42(3):121-8. | CrossRef | PubMed |
- Wang K, Liu J, Chen M. Role of B-scan ultrasonography in the localization of intraocular foreign bodies in the anterior segment: a report of three cases. BMC Ophthalmol. 2015 Aug 14;15:102. | CrossRef | PubMed |
- Ahmed Y, Schimel AM, Pathengay A, Colyer MH, Flynn HW Jr. Endophthalmitis following open-globe injuries. Eye (Lond). 2012 Feb;26(2):212-7. | CrossRef | PubMed |
- Teitelbaum GP, Raney M, Carvlin MJ, Matsumoto AH, Barth KH. Evaluation of ferromagnetism and magnetic resonance imaging artifacts of the Strecker tantalum vascular stent. Cardiovasc Intervent Radiol. 1989 May-Jun;12(3):125-7. | CrossRef | PubMed |
- Teitelbaum GP, Ortega HV, Vinitski S, Stern H, Tsuruda JS, Mitchell DG, et al. Low-artifact intravascular devices: MR imaging evaluation. Radiology. 1988 Sep;168(3):713-9. | CrossRef | PubMed |
- Zhou FY, Qiu KJ, Li HF, Huang T, Wang BL, Li L, et al. Screening on binary Zr-1X (X = Ti, Nb, Mo, Cu, Au, Pd, Ag, Ru, Hf and Bi) alloys with good in vitro cytocompatibility and magnetic resonance imaging compatibility. Acta Biomater. 2013 Dec;9(12):9578-87. | CrossRef | PubMed |
- Zhang Y, Cheng J, Bai J, Ren C, Zhang Y, Gao X, et al. Tiny ferromagnetic intraocular foreign bodies detected by magnetic resonance imaging: a report of two cases. J Magn Reson Imaging. 2009 Mar;29(3):704-7. | CrossRef | PubMed |
- Moisseiev E, Barequet D, Zunz E, Barak A, Mardor Y, Last D, et al. VALIDATION OF AN ALGORITHM FOR NONMETALLIC INTRAOCULAR FOREIGN BODIES' COMPOSITION IDENTIFICATION BASED ON COMPUTED TOMOGRAPHY AND MAGNETIC RESONANCE IMAGING. Retina. 2015 Sep;35(9):1898-904. | CrossRef | PubMed |
- Moisseiev E, Last D, Goez D, Barak A, Mardor Y. Magnetic resonance imaging and computed tomography for the detection and characterization of nonmetallic intraocular foreign bodies. Retina. 2015 Jan;35(1):82-94. | CrossRef | PubMed |
- Otto PM, Otto RA, Virapongse C, Friedman SM, Emerson S, Li KC, et al. Screening test for detection of metallic foreign objects in the orbit before magnetic resonance imaging. Invest Radiol. 1992 Apr;27(4):308-11. | CrossRef | PubMed |
- Bryden FM, Pyott AA, Bailey M, McGhee CN. Real time ultrasound in the assessment of intraocular foreign bodies. Eye (Lond). 1990;4 ( Pt 5):727-31. | CrossRef | PubMed |
- Deramo VA, Shah GK, Baumal CR, Fineman MS, Corrĕa ZM, Benson WE, et al. The role of ultrasound biomicroscopy in ocular trauma. Trans Am Ophthalmol Soc. 1998;96:355-65; discussion 365-7. | PubMed |
- Syed R, Kim SH, Palacio A, Nunery WR, Schaal S. EX VIVO MODEL FOR THE CHARACTERIZATION AND IDENTIFICATION OF DRYWALL INTRAOCULAR FOREIGN BODIES ON COMPUTED TOMOGRAPHY. Retina. 2018 Jul;38(7):1432-1435. | CrossRef | PubMed |
- Baillif S, Paoli V. [Open-globe injuries and intraocular foreign bodies involving the posterior segment]. J Fr Ophtalmol. 2012 Feb;35(2):136-45. | CrossRef | PubMed |
- Yeh S, Colyer MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol. 2008 May;19(3):225-33. | CrossRef | PubMed |
- Chaudhry IA, Shamsi FA, Al-Harthi E, Al-Theeb A, Elzaridi E, Riley FC. Incidence and visual outcome of endophthalmitis associated with intraocular foreign bodies. Graefes Arch Clin Exp Ophthalmol. 2008 Feb;246(2):181-6. | CrossRef | PubMed |
- Colyer MH, Weber ED, Weichel ED, Dick JS, Bower KS, Ward TP, et al. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology. 2007 Aug;114(8):1439-47. | CrossRef | PubMed |
- Markowski J, Dziubdziela W, Gierek T, Witkowska M, Mrukwa-Kominek E, Niedzielska I, et al. Intraorbital foreign bodies--5 own cases and review of literature. Otolaryngol Pol. 2012 Jul-Aug;66(4):295-300. | CrossRef | PubMed |
- Ho VH, Wilson MW, Fleming JC, Haik BG. Retained intraorbital metallic foreign bodies. Ophthalmic Plast Reconstr Surg. 2004 May;20(3):232-6. | CrossRef | PubMed |
 Beshay N, Keay L, Dunn H, Kamalden TA, Hoskin AK, Watson SL. The epidemiology of Open Globe Injuries presenting to a tertiary referral eye hospital in Australia. Injury. 2017 Jul;48(7):1348-1354. | CrossRef | PubMed |
Beshay N, Keay L, Dunn H, Kamalden TA, Hoskin AK, Watson SL. The epidemiology of Open Globe Injuries presenting to a tertiary referral eye hospital in Australia. Injury. 2017 Jul;48(7):1348-1354. | CrossRef | PubMed | Mester V, Kuhn F. Intraocular foreign bodies. Ophthalmol Clin North Am. 2002 Jun;15(2):235-42. | CrossRef | PubMed |
Mester V, Kuhn F. Intraocular foreign bodies. Ophthalmol Clin North Am. 2002 Jun;15(2):235-42. | CrossRef | PubMed | Zhang Y, Zhang M, Jiang C, Qiu HY. Intraocular foreign bodies in china: clinical characteristics, prognostic factors, and visual outcomes in 1,421 eyes. Am J Ophthalmol. 2011 Jul;152(1):66-73.e1. | CrossRef | PubMed |
Zhang Y, Zhang M, Jiang C, Qiu HY. Intraocular foreign bodies in china: clinical characteristics, prognostic factors, and visual outcomes in 1,421 eyes. Am J Ophthalmol. 2011 Jul;152(1):66-73.e1. | CrossRef | PubMed | Yaşa D, Erdem ZG, Demircan A, Demir G, Alkın Z. Prognostic value of ocular trauma score for open globe injuries associated with metallic intraocular foreign bodies. BMC Ophthalmol. 2018 Aug 9;18(1):194. | CrossRef | PubMed |
Yaşa D, Erdem ZG, Demircan A, Demir G, Alkın Z. Prognostic value of ocular trauma score for open globe injuries associated with metallic intraocular foreign bodies. BMC Ophthalmol. 2018 Aug 9;18(1):194. | CrossRef | PubMed | Sharma S, Thapa R, Bajimaya S, Pradhan E, Poudyal G. Clinical characteristics and visual outcome, prognostic factor, visual acuity and globe survival in posterior segment intraocular foreign body at Tilganga Institute of Ophthalmology. Nepal J Ophthalmol. 2018 Jan;10(19):66-72. | CrossRef | PubMed |
Sharma S, Thapa R, Bajimaya S, Pradhan E, Poudyal G. Clinical characteristics and visual outcome, prognostic factor, visual acuity and globe survival in posterior segment intraocular foreign body at Tilganga Institute of Ophthalmology. Nepal J Ophthalmol. 2018 Jan;10(19):66-72. | CrossRef | PubMed | Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: A review. Surv Ophthalmol. 2016 Sep-Oct;61(5):582-96. | CrossRef | PubMed |
Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: A review. Surv Ophthalmol. 2016 Sep-Oct;61(5):582-96. | CrossRef | PubMed | Duan F, Yuan Z, Liao J, Zheng Y, Yang Y, Lin X. Incidence and Risk Factors of Intraocular Foreign Body-Related Endophthalmitis in Southern China. J Ophthalmol. 2018 Sep 30;2018:8959108. | CrossRef | PubMed |
Duan F, Yuan Z, Liao J, Zheng Y, Yang Y, Lin X. Incidence and Risk Factors of Intraocular Foreign Body-Related Endophthalmitis in Southern China. J Ophthalmol. 2018 Sep 30;2018:8959108. | CrossRef | PubMed | Modjtahedi BS, Rong A, Bobinski M, McGahan J, Morse LS. Imaging characteristics of intraocular foreign bodies: a comparative study of plain film X-ray, computed tomography, ultrasound, and magnetic resonance imaging. Retina. 2015 Jan;35(1):95-104. | CrossRef | PubMed |
Modjtahedi BS, Rong A, Bobinski M, McGahan J, Morse LS. Imaging characteristics of intraocular foreign bodies: a comparative study of plain film X-ray, computed tomography, ultrasound, and magnetic resonance imaging. Retina. 2015 Jan;35(1):95-104. | CrossRef | PubMed | Lin TC, Liao TC, Yuan WH, Lee FL, Chen SJ. Management and clinical outcomes of intraocular foreign bodies with the aid of orbital computed tomography. J Chin Med Assoc. 2014 Aug;77(8):433-6. | CrossRef | PubMed |
Lin TC, Liao TC, Yuan WH, Lee FL, Chen SJ. Management and clinical outcomes of intraocular foreign bodies with the aid of orbital computed tomography. J Chin Med Assoc. 2014 Aug;77(8):433-6. | CrossRef | PubMed | Kaushik S, Ichhpujani P, Ramasubramanian A, Pandav SS. Occult intraocular foreign body: ultrasound biomicroscopy holds the key. Int Ophthalmol. 2008 Feb;28(1):71-3. | CrossRef | PubMed |
Kaushik S, Ichhpujani P, Ramasubramanian A, Pandav SS. Occult intraocular foreign body: ultrasound biomicroscopy holds the key. Int Ophthalmol. 2008 Feb;28(1):71-3. | CrossRef | PubMed | Siedlecki AN, Tsui E, Deng J, Miller DM. Long-Term Retention of an Intraorbital Metallic Foreign Body Adjacent to the Optic Nerve. Case Rep Ophthalmol Med. 2016;2016:3918592. | CrossRef | PubMed |
Siedlecki AN, Tsui E, Deng J, Miller DM. Long-Term Retention of an Intraorbital Metallic Foreign Body Adjacent to the Optic Nerve. Case Rep Ophthalmol Med. 2016;2016:3918592. | CrossRef | PubMed | Parke DW 3rd, Flynn HW Jr, Fisher YL. Management of intraocular foreign bodies: a clinical flight plan. Can J Ophthalmol. 2013 Feb;48(1):8-12. | CrossRef | PubMed |
Parke DW 3rd, Flynn HW Jr, Fisher YL. Management of intraocular foreign bodies: a clinical flight plan. Can J Ophthalmol. 2013 Feb;48(1):8-12. | CrossRef | PubMed | Ho VT, McGuckin JF Jr, Smergel EM. Intraorbital wooden foreign body: CT and MR appearance. AJNR Am J Neuroradiol. 1996 Jan;17(1):134-6. | PubMed |
Ho VT, McGuckin JF Jr, Smergel EM. Intraorbital wooden foreign body: CT and MR appearance. AJNR Am J Neuroradiol. 1996 Jan;17(1):134-6. | PubMed | Pieramici DJ, Sternberg P Jr, Aaberg TM Sr, Bridges WZ Jr, Capone A Jr, Cardillo JA, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997 Jun;123(6):820-31. | CrossRef | PubMed |
Pieramici DJ, Sternberg P Jr, Aaberg TM Sr, Bridges WZ Jr, Capone A Jr, Cardillo JA, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997 Jun;123(6):820-31. | CrossRef | PubMed | Williams DF, Mieler WF, Abrams GW, Lewis H. Results and prognostic factors in penetrating ocular injuries with retained intraocular foreign bodies. Ophthalmology. 1988 Jul;95(7):911-6. | CrossRef | PubMed |
Williams DF, Mieler WF, Abrams GW, Lewis H. Results and prognostic factors in penetrating ocular injuries with retained intraocular foreign bodies. Ophthalmology. 1988 Jul;95(7):911-6. | CrossRef | PubMed | Jonas JB, Knorr HL, Budde WM. Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology. 2000 May;107(5):823-8. | CrossRef | PubMed |
Jonas JB, Knorr HL, Budde WM. Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology. 2000 May;107(5):823-8. | CrossRef | PubMed | Kuhn F, Morris R, Witherspoon CD, Mann L. Epidemiology of blinding trauma in the United States Eye Injury Registry. Ophthalmic Epidemiol. 2006 Jun;13(3):209-16. | CrossRef | PubMed |
Kuhn F, Morris R, Witherspoon CD, Mann L. Epidemiology of blinding trauma in the United States Eye Injury Registry. Ophthalmic Epidemiol. 2006 Jun;13(3):209-16. | CrossRef | PubMed | Woodcock MG, Scott RA, Huntbach J, Kirkby GR. Mass and shape as factors in intraocular foreign body injuries. Ophthalmology. 2006 Dec;113(12):2262-9. | CrossRef | PubMed |
Woodcock MG, Scott RA, Huntbach J, Kirkby GR. Mass and shape as factors in intraocular foreign body injuries. Ophthalmology. 2006 Dec;113(12):2262-9. | CrossRef | PubMed | Ehlers JP, Kunimoto DY, Ittoop S, Maguire JI, Ho AC, Regillo CD. Metallic intraocular foreign bodies: characteristics, interventions, and prognostic factors for visual outcome and globe survival. Am J Ophthalmol. 2008 Sep;146(3):427-433. | CrossRef | PubMed |
Ehlers JP, Kunimoto DY, Ittoop S, Maguire JI, Ho AC, Regillo CD. Metallic intraocular foreign bodies: characteristics, interventions, and prognostic factors for visual outcome and globe survival. Am J Ophthalmol. 2008 Sep;146(3):427-433. | CrossRef | PubMed | Bhagat N, Nagori S, Zarbin M. Post-traumatic Infectious Endophthalmitis. Surv Ophthalmol. 2011 May-Jun;56(3):214-51. | CrossRef | PubMed |
Bhagat N, Nagori S, Zarbin M. Post-traumatic Infectious Endophthalmitis. Surv Ophthalmol. 2011 May-Jun;56(3):214-51. | CrossRef | PubMed | Patel SN, Langer PD, Zarbin MA, Bhagat N. Diagnostic value of clinical examination and radiographic imaging in identification of intraocular foreign bodies in open globe injury. Eur J Ophthalmol. 2012 Mar-Apr;22(2):259-68. | CrossRef | PubMed |
Patel SN, Langer PD, Zarbin MA, Bhagat N. Diagnostic value of clinical examination and radiographic imaging in identification of intraocular foreign bodies in open globe injury. Eur J Ophthalmol. 2012 Mar-Apr;22(2):259-68. | CrossRef | PubMed | Saeed A, Cassidy L, Malone DE, Beatty S. Plain X-ray and computed tomography of the orbit in cases and suspected cases of intraocular foreign body. Eye (Lond). 2008 Nov;22(11):1373-7. | CrossRef | PubMed |
Saeed A, Cassidy L, Malone DE, Beatty S. Plain X-ray and computed tomography of the orbit in cases and suspected cases of intraocular foreign body. Eye (Lond). 2008 Nov;22(11):1373-7. | CrossRef | PubMed | de Santana Santos T, Avelar RL, Melo AR, de Moraes HH, Dourado E. Current approach in the management of patients with foreign bodies in the maxillofacial region. J Oral Maxillofac Surg. 2011 Sep;69(9):2376-82. | CrossRef | PubMed |
de Santana Santos T, Avelar RL, Melo AR, de Moraes HH, Dourado E. Current approach in the management of patients with foreign bodies in the maxillofacial region. J Oral Maxillofac Surg. 2011 Sep;69(9):2376-82. | CrossRef | PubMed | Bray LC, Griffiths PG. The value of plain radiography in suspected intraocular foreign body. Eye (Lond). 1991;5 ( Pt 6):751-4. | CrossRef | PubMed |
Bray LC, Griffiths PG. The value of plain radiography in suspected intraocular foreign body. Eye (Lond). 1991;5 ( Pt 6):751-4. | CrossRef | PubMed | McElvanney AM, Fielder AR. Intraocular foreign body missed by radiography. BMJ. 1993 Apr 17;306(6884):1060-1. | CrossRef | PubMed |
McElvanney AM, Fielder AR. Intraocular foreign body missed by radiography. BMJ. 1993 Apr 17;306(6884):1060-1. | CrossRef | PubMed | Winegar BA, Gutierrez JE. Imaging of Orbital Trauma and Emergent Non-traumatic Conditions. Neuroimaging Clin N Am. 2015 Aug;25(3):439-56. | CrossRef | PubMed |
Winegar BA, Gutierrez JE. Imaging of Orbital Trauma and Emergent Non-traumatic Conditions. Neuroimaging Clin N Am. 2015 Aug;25(3):439-56. | CrossRef | PubMed | Lagalla R, Manfrè L, Caronia A, Bencivinni F, Duranti C, Ponte F. Plain film, CT and MRI sensibility in the evaluation of intraorbital foreign bodies in an in vitro model of the orbit and in pig eyes. Eur Radiol. 2000;10(8):1338-41. | CrossRef | PubMed |
Lagalla R, Manfrè L, Caronia A, Bencivinni F, Duranti C, Ponte F. Plain film, CT and MRI sensibility in the evaluation of intraorbital foreign bodies in an in vitro model of the orbit and in pig eyes. Eur Radiol. 2000;10(8):1338-41. | CrossRef | PubMed | Chacko JG, Figueroa RE, Johnson MH, Marcus DM, Brooks SE. Detection and localization of steel intraocular foreign bodies using computed tomography. A comparison of helical and conventional axial scanning. Ophthalmology. 1997 Feb;104(2):319-23. | CrossRef | PubMed |
Chacko JG, Figueroa RE, Johnson MH, Marcus DM, Brooks SE. Detection and localization of steel intraocular foreign bodies using computed tomography. A comparison of helical and conventional axial scanning. Ophthalmology. 1997 Feb;104(2):319-23. | CrossRef | PubMed | Rong AJ, Fan KC, Golshani B, Bobinski M, McGahan JP, Eliott D, et al. Multimodal imaging features of intraocular foreign bodies. Semin Ophthalmol. 2019;34(7-8):518-532. | CrossRef | PubMed |
Rong AJ, Fan KC, Golshani B, Bobinski M, McGahan JP, Eliott D, et al. Multimodal imaging features of intraocular foreign bodies. Semin Ophthalmol. 2019;34(7-8):518-532. | CrossRef | PubMed | Tate E, Cupples H. Detection of orbital foreign bodies with computed tomography: current limits. AJR Am J Roentgenol. 1981 Sep;137(3):493-5. | CrossRef | PubMed |
Tate E, Cupples H. Detection of orbital foreign bodies with computed tomography: current limits. AJR Am J Roentgenol. 1981 Sep;137(3):493-5. | CrossRef | PubMed | Javadrashid R, Golamian M, Shahrzad M, Hajalioghli P, Shahmorady Z, Fouladi DF, et al. Visibility of Different Intraorbital Foreign Bodies Using Plain Radiography, Computed Tomography, Magnetic Resonance Imaging, and Cone-Beam Computed Tomography: An In Vitro Study. Can Assoc Radiol J. 2017 May;68(2):194-201. | CrossRef | PubMed |
Javadrashid R, Golamian M, Shahrzad M, Hajalioghli P, Shahmorady Z, Fouladi DF, et al. Visibility of Different Intraorbital Foreign Bodies Using Plain Radiography, Computed Tomography, Magnetic Resonance Imaging, and Cone-Beam Computed Tomography: An In Vitro Study. Can Assoc Radiol J. 2017 May;68(2):194-201. | CrossRef | PubMed | Lakits A, Prokesch R, Scholda C, Bankier A. Orbital helical computed tomography in the diagnosis and management of eye trauma. Ophthalmology. 1999 Dec;106(12):2330-5. | CrossRef | PubMed |
Lakits A, Prokesch R, Scholda C, Bankier A. Orbital helical computed tomography in the diagnosis and management of eye trauma. Ophthalmology. 1999 Dec;106(12):2330-5. | CrossRef | PubMed | Prokesch R, Lakits A, Scholda C, Bankier A, Ba-Ssalamah A, Imhof H. [Spiral CT and conventional CT in the preoperative imaging of intraocular metal foreign bodies]. Radiologe. 1998 Aug;38(8):667-73. | CrossRef | PubMed |
Prokesch R, Lakits A, Scholda C, Bankier A, Ba-Ssalamah A, Imhof H. [Spiral CT and conventional CT in the preoperative imaging of intraocular metal foreign bodies]. Radiologe. 1998 Aug;38(8):667-73. | CrossRef | PubMed | Gor DM, Kirsch CF, Leen J, Turbin R, Von Hagen S. Radiologic differentiation of intraocular glass: evaluation of imaging techniques, glass types, size, and effect of intraocular hemorrhage. AJR Am J Roentgenol. 2001 Nov;177(5):1199-203. | CrossRef | PubMed |
Gor DM, Kirsch CF, Leen J, Turbin R, Von Hagen S. Radiologic differentiation of intraocular glass: evaluation of imaging techniques, glass types, size, and effect of intraocular hemorrhage. AJR Am J Roentgenol. 2001 Nov;177(5):1199-203. | CrossRef | PubMed | Lit ES, Young LH. Anterior and posterior segment intraocular foreign bodies. Int Ophthalmol Clin. 2002 Summer;42(3):107-20. | CrossRef | PubMed |
Lit ES, Young LH. Anterior and posterior segment intraocular foreign bodies. Int Ophthalmol Clin. 2002 Summer;42(3):107-20. | CrossRef | PubMed | Wickham L, Xing W, Bunce C, Sullivan P. Outcomes of surgery for posterior segment intraocular foreign bodies--a retrospective review of 17 years of clinical experience. Graefes Arch Clin Exp Ophthalmol. 2006 Dec;244(12):1620-6. | CrossRef | PubMed |
Wickham L, Xing W, Bunce C, Sullivan P. Outcomes of surgery for posterior segment intraocular foreign bodies--a retrospective review of 17 years of clinical experience. Graefes Arch Clin Exp Ophthalmol. 2006 Dec;244(12):1620-6. | CrossRef | PubMed | Costa MA, Garcia PN, Barroso LF, Ferreira MA, Okuda ÉA, Allemann N. Composition of intraocular foreign bodies: experimental study of ultrasonographic presentation. Arq Bras Oftalmol. 2013 Jan-Feb;76(1):13-7. | CrossRef | PubMed |
Costa MA, Garcia PN, Barroso LF, Ferreira MA, Okuda ÉA, Allemann N. Composition of intraocular foreign bodies: experimental study of ultrasonographic presentation. Arq Bras Oftalmol. 2013 Jan-Feb;76(1):13-7. | CrossRef | PubMed | Zacks DN, Hart L, Young LH. Ultrasonography in the traumatized eye: intraocular foreign body versus artifact. Int Ophthalmol Clin. 2002 Summer;42(3):121-8. | CrossRef | PubMed |
Zacks DN, Hart L, Young LH. Ultrasonography in the traumatized eye: intraocular foreign body versus artifact. Int Ophthalmol Clin. 2002 Summer;42(3):121-8. | CrossRef | PubMed | Wang K, Liu J, Chen M. Role of B-scan ultrasonography in the localization of intraocular foreign bodies in the anterior segment: a report of three cases. BMC Ophthalmol. 2015 Aug 14;15:102. | CrossRef | PubMed |
Wang K, Liu J, Chen M. Role of B-scan ultrasonography in the localization of intraocular foreign bodies in the anterior segment: a report of three cases. BMC Ophthalmol. 2015 Aug 14;15:102. | CrossRef | PubMed | Ahmed Y, Schimel AM, Pathengay A, Colyer MH, Flynn HW Jr. Endophthalmitis following open-globe injuries. Eye (Lond). 2012 Feb;26(2):212-7. | CrossRef | PubMed |
Ahmed Y, Schimel AM, Pathengay A, Colyer MH, Flynn HW Jr. Endophthalmitis following open-globe injuries. Eye (Lond). 2012 Feb;26(2):212-7. | CrossRef | PubMed | Teitelbaum GP, Raney M, Carvlin MJ, Matsumoto AH, Barth KH. Evaluation of ferromagnetism and magnetic resonance imaging artifacts of the Strecker tantalum vascular stent. Cardiovasc Intervent Radiol. 1989 May-Jun;12(3):125-7. | CrossRef | PubMed |
Teitelbaum GP, Raney M, Carvlin MJ, Matsumoto AH, Barth KH. Evaluation of ferromagnetism and magnetic resonance imaging artifacts of the Strecker tantalum vascular stent. Cardiovasc Intervent Radiol. 1989 May-Jun;12(3):125-7. | CrossRef | PubMed | Teitelbaum GP, Ortega HV, Vinitski S, Stern H, Tsuruda JS, Mitchell DG, et al. Low-artifact intravascular devices: MR imaging evaluation. Radiology. 1988 Sep;168(3):713-9. | CrossRef | PubMed |
Teitelbaum GP, Ortega HV, Vinitski S, Stern H, Tsuruda JS, Mitchell DG, et al. Low-artifact intravascular devices: MR imaging evaluation. Radiology. 1988 Sep;168(3):713-9. | CrossRef | PubMed | Zhou FY, Qiu KJ, Li HF, Huang T, Wang BL, Li L, et al. Screening on binary Zr-1X (X = Ti, Nb, Mo, Cu, Au, Pd, Ag, Ru, Hf and Bi) alloys with good in vitro cytocompatibility and magnetic resonance imaging compatibility. Acta Biomater. 2013 Dec;9(12):9578-87. | CrossRef | PubMed |
Zhou FY, Qiu KJ, Li HF, Huang T, Wang BL, Li L, et al. Screening on binary Zr-1X (X = Ti, Nb, Mo, Cu, Au, Pd, Ag, Ru, Hf and Bi) alloys with good in vitro cytocompatibility and magnetic resonance imaging compatibility. Acta Biomater. 2013 Dec;9(12):9578-87. | CrossRef | PubMed | Zhang Y, Cheng J, Bai J, Ren C, Zhang Y, Gao X, et al. Tiny ferromagnetic intraocular foreign bodies detected by magnetic resonance imaging: a report of two cases. J Magn Reson Imaging. 2009 Mar;29(3):704-7. | CrossRef | PubMed |
Zhang Y, Cheng J, Bai J, Ren C, Zhang Y, Gao X, et al. Tiny ferromagnetic intraocular foreign bodies detected by magnetic resonance imaging: a report of two cases. J Magn Reson Imaging. 2009 Mar;29(3):704-7. | CrossRef | PubMed | Moisseiev E, Barequet D, Zunz E, Barak A, Mardor Y, Last D, et al. VALIDATION OF AN ALGORITHM FOR NONMETALLIC INTRAOCULAR FOREIGN BODIES' COMPOSITION IDENTIFICATION BASED ON COMPUTED TOMOGRAPHY AND MAGNETIC RESONANCE IMAGING. Retina. 2015 Sep;35(9):1898-904. | CrossRef | PubMed |
Moisseiev E, Barequet D, Zunz E, Barak A, Mardor Y, Last D, et al. VALIDATION OF AN ALGORITHM FOR NONMETALLIC INTRAOCULAR FOREIGN BODIES' COMPOSITION IDENTIFICATION BASED ON COMPUTED TOMOGRAPHY AND MAGNETIC RESONANCE IMAGING. Retina. 2015 Sep;35(9):1898-904. | CrossRef | PubMed | Moisseiev E, Last D, Goez D, Barak A, Mardor Y. Magnetic resonance imaging and computed tomography for the detection and characterization of nonmetallic intraocular foreign bodies. Retina. 2015 Jan;35(1):82-94. | CrossRef | PubMed |
Moisseiev E, Last D, Goez D, Barak A, Mardor Y. Magnetic resonance imaging and computed tomography for the detection and characterization of nonmetallic intraocular foreign bodies. Retina. 2015 Jan;35(1):82-94. | CrossRef | PubMed | Otto PM, Otto RA, Virapongse C, Friedman SM, Emerson S, Li KC, et al. Screening test for detection of metallic foreign objects in the orbit before magnetic resonance imaging. Invest Radiol. 1992 Apr;27(4):308-11. | CrossRef | PubMed |
Otto PM, Otto RA, Virapongse C, Friedman SM, Emerson S, Li KC, et al. Screening test for detection of metallic foreign objects in the orbit before magnetic resonance imaging. Invest Radiol. 1992 Apr;27(4):308-11. | CrossRef | PubMed | Bryden FM, Pyott AA, Bailey M, McGhee CN. Real time ultrasound in the assessment of intraocular foreign bodies. Eye (Lond). 1990;4 ( Pt 5):727-31. | CrossRef | PubMed |
Bryden FM, Pyott AA, Bailey M, McGhee CN. Real time ultrasound in the assessment of intraocular foreign bodies. Eye (Lond). 1990;4 ( Pt 5):727-31. | CrossRef | PubMed | Deramo VA, Shah GK, Baumal CR, Fineman MS, Corrĕa ZM, Benson WE, et al. The role of ultrasound biomicroscopy in ocular trauma. Trans Am Ophthalmol Soc. 1998;96:355-65; discussion 365-7. | PubMed |
Deramo VA, Shah GK, Baumal CR, Fineman MS, Corrĕa ZM, Benson WE, et al. The role of ultrasound biomicroscopy in ocular trauma. Trans Am Ophthalmol Soc. 1998;96:355-65; discussion 365-7. | PubMed | Syed R, Kim SH, Palacio A, Nunery WR, Schaal S. EX VIVO MODEL FOR THE CHARACTERIZATION AND IDENTIFICATION OF DRYWALL INTRAOCULAR FOREIGN BODIES ON COMPUTED TOMOGRAPHY. Retina. 2018 Jul;38(7):1432-1435. | CrossRef | PubMed |
Syed R, Kim SH, Palacio A, Nunery WR, Schaal S. EX VIVO MODEL FOR THE CHARACTERIZATION AND IDENTIFICATION OF DRYWALL INTRAOCULAR FOREIGN BODIES ON COMPUTED TOMOGRAPHY. Retina. 2018 Jul;38(7):1432-1435. | CrossRef | PubMed | Baillif S, Paoli V. [Open-globe injuries and intraocular foreign bodies involving the posterior segment]. J Fr Ophtalmol. 2012 Feb;35(2):136-45. | CrossRef | PubMed |
Baillif S, Paoli V. [Open-globe injuries and intraocular foreign bodies involving the posterior segment]. J Fr Ophtalmol. 2012 Feb;35(2):136-45. | CrossRef | PubMed | Yeh S, Colyer MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol. 2008 May;19(3):225-33. | CrossRef | PubMed |
Yeh S, Colyer MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol. 2008 May;19(3):225-33. | CrossRef | PubMed | Chaudhry IA, Shamsi FA, Al-Harthi E, Al-Theeb A, Elzaridi E, Riley FC. Incidence and visual outcome of endophthalmitis associated with intraocular foreign bodies. Graefes Arch Clin Exp Ophthalmol. 2008 Feb;246(2):181-6. | CrossRef | PubMed |
Chaudhry IA, Shamsi FA, Al-Harthi E, Al-Theeb A, Elzaridi E, Riley FC. Incidence and visual outcome of endophthalmitis associated with intraocular foreign bodies. Graefes Arch Clin Exp Ophthalmol. 2008 Feb;246(2):181-6. | CrossRef | PubMed | Colyer MH, Weber ED, Weichel ED, Dick JS, Bower KS, Ward TP, et al. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology. 2007 Aug;114(8):1439-47. | CrossRef | PubMed |
Colyer MH, Weber ED, Weichel ED, Dick JS, Bower KS, Ward TP, et al. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology. 2007 Aug;114(8):1439-47. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








