Key Words: advanced gallbladder cancer, resective surgery, palliative, Epistemonikos, GRADE..
Abstract
INTRODUCTION
Despite multiple advances in medicine, gallbladder cancer remains a disease with poor prognosis. In advanced stages, the main options are surgical management or palliative non-surgical care. However, it is not clear which therapy constitutes a better alternative.
METHODS
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified one systematic review including three primary studies, none of them randomized. We concluded that resective surgery may increase survival rates in patients with advanced gallbladder cancer, but the certainty of the evidence is low.
Problem
Gallbladder cancer is an uncommon cancer, but it is the most common biliary duct cancer, representing 85-90% [1]. However, diagnosis is frequently done at a late stage, since it does not present with symptoms or signs in earlier stages, and prognosis remains ominous in comparison to other types of cancer. Five-year overall survival is 18%, while in advanced stages it might be as low as 2 to 8 percent [2]. Thus, it is imperative to clarify the best type of treatment, particularly in stages considered incurable.
Traditionally, two distinct forms of treatment have been proposed in advanced stages: resective surgery and palliative non-surgical care. Unlike resective surgery which has curative intent in early stages, in advanced gallbladder cancer the aim is to reduce tumor size, and to improve quality of life and survival.
However, its comparative effectiveness against other palliative alternatives such as chemotherapy, endoscopic therapy, interventional radiology or other medical therapies is still a matter of controversy.
Methods
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
Only one systematic review [3] was found, which included three primary studies [4], [5], [6], none of them a randomized trial. |
|
What types of patients were included* |
All primary studies included adult patients with advanced gallbladder cancer. |
|
What types of interventions were included* |
All primary studies assessed surgical treatment in comparison to any type of palliative non-surgical treatment. One study [4] assessed resective surgery, palliative chemotherapy and best available supportive care (biliary duct prosthesis, external biliary drain and radiotherapy). Another study [5] evaluated resective surgery and palliative care (chemotherapy and radiotherapy). The last study [6] compared surgical treatment to chemotherapy and other palliative treatments. |
|
What types of outcomes |
All studies and the review reported survival as main outcome. |
* Information about primary studies is not extracted directly from primary studies but from identified systematic reviews, unless otherwise stated.
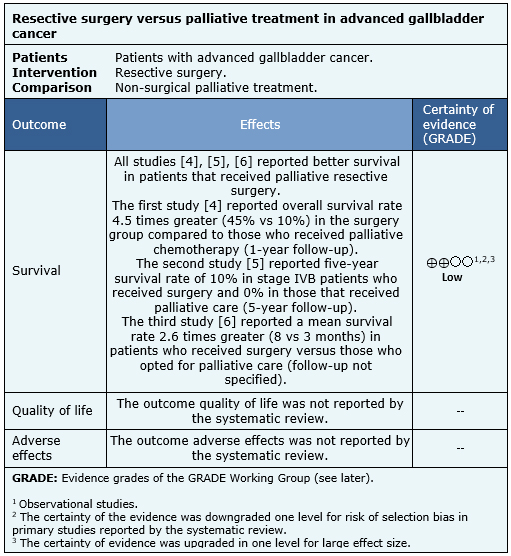
Summary of findings
Information about the effects of resective surgery on advanced gallbladder cancer is based on three studies, that included 2990 participants overall [4], [5], [6].
All of the studies assessed overall survival rate. The review reported the data were not suitable for incorporation into a meta-analysis, so the information is presented as a narrative synthesis.
The summary of findings is as follows:
- Resective surgery may increase survival rate in advanced gallbladder cancer (low certainty of evidence)
- No studies were found that assessed quality of life.
- No studies were found that assessed adverse effects.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
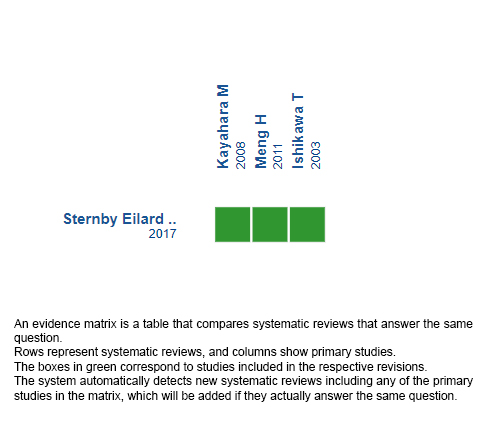
Follow the link to access the interactive version: Resective surgery versus palliative care in advanced gallbladder cancer
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
A pesar de los múltiples avances de la medicina, el cáncer de vesícula sigue siendo una enfermedad con mal pronóstico. En su etapa avanzada, se plantea el tratamiento quirúrgico o paliativo no quirúrgico, pero no está claro cual de las alternativas constituye una mejor opción.
MÉTODOS
Realizamos una búsqueda en Epistemonikos, la mayor base de datos de revisiones sistemáticas en salud, la cual es mantenida mediante el cribado de múltiples fuentes de información, incluyendo MEDLINE, EMBASE, Cochrane, entre otras. Extrajimos los datos desde las revisiones identificadas, analizamos los datos de los estudios primarios y preparamos una tabla de resumen de los resultados utilizando el método GRADE.
RESULTADOS Y CONCLUSIONES
Identificamos sólo una revisión sistemática que incluyó tres estudios primarios, de los cuales ninguno corresponde a un ensayo aleatorizado. Concluimos que la cirugía resectiva podría aumentar la sobrevida en los pacientes con cáncer de vesícula avanzado, pero la certeza de la evidencia es baja.
 Authors:
Jai-sen Leung [1,2], Eduardo Viñuela[2,3]
Authors:
Jai-sen Leung [1,2], Eduardo Viñuela[2,3]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile.
[2] Proyecto Epistemonikos, Santiago, Chile.
[3] Departamento de Cirugía, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile.
E-mail: evinuela@uc.cl
Author address:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Diagonal Paraguay 476 Santiago Chile

Citation: Leung J, Viñuela E. Resective surgery versus palliative care in advanced gallbladder cancer. Medwave 2019;19(10):e7725 doi: 10.5867/medwave.2019.10.7725
Submission date: 4/8/2019
Acceptance date: 21/11/2019
Publication date: 26/11/2019
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Epistemonikos Evidence Synthesis Project.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Hundal R, Shaffer EA. Gallbladder cancer: epidemiology and outcome [Internet]. Clinical epidemiology. Dove Medical Press; 2014 . | CrossRef | PubMed | Link |
- Survival Rates for Gallbladder Cancer [Internet]. American Cancer Society. 2018. | Link |
- Surgical treatment for gallbladder cancer – a systematic literature review. Scandinavian Journal of Gastroenterology . 2017 ;52(5):505-514. | CrossRef | PubMed | Link |
- Ishikawa T, Horimi T, Shima Y, Okabayashi T, Nishioka Y, Hamada M et al. Evaluation of aggressive surgical treatment for advanced carcinoma of the gallbladder. Journal of Hepato-Biliary-Pancreatic Surgery. 2003;10(3):233-238. | CrossRef | PubMed |
- Kayahara M, Nagakawa T, Nakagawara H, Kitagawa H, Ohta T. Prognostic Factors for Gallbladder Cancer in Japan. Annals of Surgery. 2008;248(5):807-814. | CrossRef | PubMed |
- Meng H, Wang X, Fong Y, Wang Z, Wang Y, Zhang Z. Outcomes of Radical Surgery for Gallbladder Cancer Patients with Lymphatic Metastases. Japanese Journal of Clinical Oncology. 2011;41(8):992-998. | CrossRef | PubMed |
- Lee S, Kim K, Kim W, Kim I, Nah Y, Ryu D et al. Practical Guidelines for the Surgical Treatment of Gallbladder Cancer. Journal of Korean Medical Science. 2014;29(10):1333. | CrossRef | PubMed |
- Benson A, Abrams T, Ben-Josef E, Bloomston P, Botha J, Clary B et al. NCCN clinical practice guidelines in oncology: hepatobiliary cancers. J Natl Compr Canc Netw. 2009;7(4):350-391. | PubMed |
- Bethesda. Gallbladder Cancer Treatment . National Cancer Institute. 2019. | Link |
- Matull W, Dhar D, Ayaru L, Sandanayake N, Chapman M, Dias A et al. R0 but not R1/R2 resection is associated with better survival than palliative photodynamic therapy in biliary tract cancer. Liver International. 2010;31(1):99-107. | CrossRef | PubMed |
- Amblard I, Mercier F, Bartlett D, Ahrendt S, Lee K, Zeh H et al. Cytoreductive surgery and HIPEC improve survival compared to palliative chemotherapy for biliary carcinoma with peritoneal metastasis: A multi-institutional cohort from PSOGI and BIG RENAPE groups. European Journal of Surgical Oncology. 2018;44(9):1378-1383. | CrossRef | PubMed |
- Buettner S, Wilson A, Margonis G, Gani F, Ethun C, Poultsides G et al. Assessing Trends in Palliative Surgery for Extrahepatic Biliary Malignancies: A 15-Year Multicenter Study. Journal of Gastrointestinal Surgery. 2016;20(8):1444-1452. | CrossRef | PubMed |
 Hundal R, Shaffer EA. Gallbladder cancer: epidemiology and outcome [Internet]. Clinical epidemiology. Dove Medical Press; 2014 . | CrossRef | PubMed | Link |
Hundal R, Shaffer EA. Gallbladder cancer: epidemiology and outcome [Internet]. Clinical epidemiology. Dove Medical Press; 2014 . | CrossRef | PubMed | Link | Surgical treatment for gallbladder cancer – a systematic literature review. Scandinavian Journal of Gastroenterology . 2017 ;52(5):505-514. | CrossRef | PubMed | Link |
Surgical treatment for gallbladder cancer – a systematic literature review. Scandinavian Journal of Gastroenterology . 2017 ;52(5):505-514. | CrossRef | PubMed | Link | Ishikawa T, Horimi T, Shima Y, Okabayashi T, Nishioka Y, Hamada M et al. Evaluation of aggressive surgical treatment for advanced carcinoma of the gallbladder. Journal of Hepato-Biliary-Pancreatic Surgery. 2003;10(3):233-238. | CrossRef | PubMed |
Ishikawa T, Horimi T, Shima Y, Okabayashi T, Nishioka Y, Hamada M et al. Evaluation of aggressive surgical treatment for advanced carcinoma of the gallbladder. Journal of Hepato-Biliary-Pancreatic Surgery. 2003;10(3):233-238. | CrossRef | PubMed | Kayahara M, Nagakawa T, Nakagawara H, Kitagawa H, Ohta T. Prognostic Factors for Gallbladder Cancer in Japan. Annals of Surgery. 2008;248(5):807-814. | CrossRef | PubMed |
Kayahara M, Nagakawa T, Nakagawara H, Kitagawa H, Ohta T. Prognostic Factors for Gallbladder Cancer in Japan. Annals of Surgery. 2008;248(5):807-814. | CrossRef | PubMed | Meng H, Wang X, Fong Y, Wang Z, Wang Y, Zhang Z. Outcomes of Radical Surgery for Gallbladder Cancer Patients with Lymphatic Metastases. Japanese Journal of Clinical Oncology. 2011;41(8):992-998. | CrossRef | PubMed |
Meng H, Wang X, Fong Y, Wang Z, Wang Y, Zhang Z. Outcomes of Radical Surgery for Gallbladder Cancer Patients with Lymphatic Metastases. Japanese Journal of Clinical Oncology. 2011;41(8):992-998. | CrossRef | PubMed | Lee S, Kim K, Kim W, Kim I, Nah Y, Ryu D et al. Practical Guidelines for the Surgical Treatment of Gallbladder Cancer. Journal of Korean Medical Science. 2014;29(10):1333. | CrossRef | PubMed |
Lee S, Kim K, Kim W, Kim I, Nah Y, Ryu D et al. Practical Guidelines for the Surgical Treatment of Gallbladder Cancer. Journal of Korean Medical Science. 2014;29(10):1333. | CrossRef | PubMed | Benson A, Abrams T, Ben-Josef E, Bloomston P, Botha J, Clary B et al. NCCN clinical practice guidelines in oncology: hepatobiliary cancers. J Natl Compr Canc Netw. 2009;7(4):350-391. | PubMed |
Benson A, Abrams T, Ben-Josef E, Bloomston P, Botha J, Clary B et al. NCCN clinical practice guidelines in oncology: hepatobiliary cancers. J Natl Compr Canc Netw. 2009;7(4):350-391. | PubMed | Matull W, Dhar D, Ayaru L, Sandanayake N, Chapman M, Dias A et al. R0 but not R1/R2 resection is associated with better survival than palliative photodynamic therapy in biliary tract cancer. Liver International. 2010;31(1):99-107. | CrossRef | PubMed |
Matull W, Dhar D, Ayaru L, Sandanayake N, Chapman M, Dias A et al. R0 but not R1/R2 resection is associated with better survival than palliative photodynamic therapy in biliary tract cancer. Liver International. 2010;31(1):99-107. | CrossRef | PubMed | Amblard I, Mercier F, Bartlett D, Ahrendt S, Lee K, Zeh H et al. Cytoreductive surgery and HIPEC improve survival compared to palliative chemotherapy for biliary carcinoma with peritoneal metastasis: A multi-institutional cohort from PSOGI and BIG RENAPE groups. European Journal of Surgical Oncology. 2018;44(9):1378-1383. | CrossRef | PubMed |
Amblard I, Mercier F, Bartlett D, Ahrendt S, Lee K, Zeh H et al. Cytoreductive surgery and HIPEC improve survival compared to palliative chemotherapy for biliary carcinoma with peritoneal metastasis: A multi-institutional cohort from PSOGI and BIG RENAPE groups. European Journal of Surgical Oncology. 2018;44(9):1378-1383. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








