Key Words: lifting, rejuvenation, hyaluronic acid, polydioxanone, hydrolysis, complications
Abstract
We present the case of a female patient with complications from superficial implantation of polydioxanone spiculated threads in the facial middle third. The manifestations were edema, ecchymosis, superficial palpation of the thread and skin plication. For the treatment we propose a novel protocol of clinical degradation of polydioxanone threads, using hyaluronic acid injecting it into the implantation area of the polydioxanone threads. Non-cross linked hyaluronic acid was infiltrated along the path of the thread. The follow-up at seven, 21 and 45 days showed decreased edema, folds and skin irregularities due to wire traction and attenuation of secondary rhytides. A sample of the thread in hyaluronic acid was observed in a laminar flow campaign evidencing degradation at 72 hours. Administering hyaluronic acid was effective in inducing clinical biodegradation of the thread suggesting that non-crosslinked hyaluronic acid is a powerful catalyst for the hydrolytic degradation of polydioxanone.
|
Main Messages
|
Introduction
Facial rejuvenation requires understanding facial ageing by planes and that every facial layer is affected, rather than just the skin. It involves changes in subcutaneous fat redistribution that lead to deflation (soft tissue ptosis or sagging due to a loss of volume in surface panniculus adiposus and deep anniculus adiposus underneath the dermis) and lipomatosis (fat accumulation that worsens skin flaccidity). There is also thinning of the superficial musculoaponeurotic system, laxity in the main skin retaining ligaments, compensatory facial muscle activity due to soft tissue fixation loss and reabsorption in the facial skeleton, the first of the tissues to age[1],[2].
This understanding has led to the development of rejuvenation techniques, such as facial threading, preferably inserting absorbable sutures, like polydioxanone, which create tension and restructure facial tissues with ptosis[3] using the direction of the vectors, which must act against the force of gravity to provide efficient lifting[4]. This is one of the most requested procedures given the simplicity of the outpatient method and the patient’s quick recovery[5]. Adoption is so widespread that facial lifting will soon have two competing methods, lifting with tightening threads and microsurgery for deep vertical suspension[6].
From Sulamanidze’s pioneering proposal to use polypropylene sutures[7] up to the present day, a range of techniques for implanting smooth or barbed polydioxanone threads (vectors or mesh) have been proposed. The recent barbed polydioxanone threads have emerged to increase the tensile strength created[8] by the barbs on the thread that attach and induce fibrosis, mediated by myofibroblasts[9],[10]. The tightening effect comes from a reaction to a controlled and targeted foreign body along the thread vector. After insertion, it stabilises through lymphocyte infiltration mechanisms, collagen deposition, and fibrosis around the biomaterial[1].
Facial lifting with polydioxanone tightening threads has become widespread thanks to its clinical success. It has been shown to reverse deflation, lipomatosis, rhytids, and deep folds in some cases. This technique is particularly useful when requiring an absorbable and resistant fibre combination[11],[12],[13]. However, their accidental placement in a very superficial plane leads to difficult complications to resolve, as occurred with this case report.
The complications associated with barbed polydioxanone thread implants are normally haematomas, oedemas, dimples, or irregularities in the skin covering the thread, surface palpation of the thread, and folds due to retraction of the skin, events that are directly related with incorrect placement or the thread being inserted too close to the surface[4],[14],[15].
Although these are transitory events, they can last for days or weeks. The patient normally cannot return to their everyday activities until those complications have been resolved. Therefore, the recovery time after lifting using threads can be the same as required after rhytidoplasty. In this case, the patient may need a subcision to release the tissue, which implies more aggression to tissues, resulting in a longer period of convalescence. The resolution rate using surgery after the thread lifting procedures is high. 11% of patients need their threads removed as they are palpable, extruded, or because they are unhappy with their appearance[16]. Therefore, even though it is considered a transient complication, surgery ends up being required to resolve it, which goes against the aim of the polydioxanone thread lifting technique being a minimally invasive protocol.
When searching for a minimally invasive solution for this type of post barbed polydioxanone thread implantation adverse reactions in patients in whom surgical removal of the suture is indicated, the authors of this clinical case proposed an alternative method for resolving those complications. The proposal involves injecting non cross-linked hyaluronic acid along the thread to induce its hydrolysis. This derived in the objective of this case report in providing evidence of the clinical usefulness of hyaluronic acid for polydioxanone thread degradation, as a treatment for post-implantation complications.
Case presentation
This is a 36-year-old female patient with Fitzpatrick type II skin phototype and Glogau type 2 photo-ageing, who visited the office requesting medical help to resolve non-infectious complications that appeared 24 hours after implanting barbed polydioxanone threads for midface skin lifting. After the interview or anamnesis and the general clinical examination, the skin was examined directly using a magnifying glass with an artificial light source focused on the area affected by the placement of the polydioxanone threads, located between the mid and lower right face.
A direct visual inspection was undertaken to establish a diagnosis, determining the lesion’s morphological characteristics. An extensive zone of oedematous erythema, intraepidermal oedema, and ecchymosis at the ends of the thread was observed. The thread was also palpable on the surface, with evident irregularities in the form of the fold around the proximal end of the suture, toward the labial commissure, corresponding to a “skin folding” phenomenon from excessive skin retraction (Figure 1).
The findings suggested a primary basic lesion with symptoms such as increased skin temperature and sore skin on palpation. The lesion was not suppurative and was triggered by the implantation of the thread.
With the change in colour and oedema enabling the differentiation of the type of vascular lesion produced by inserting the thread, it was decided to perform a diascopy of the area or apply pressure to a glass slide, which concluded there was an exanthematous or diffuse erythematous macular basic lesion.
Dermatosis without desquamation was established as the main diagnosis, which was flat and of an exanthematous or diffuse macular-erythematous type derived from an iatrogenic lesion. A blood test was requested as a complementary analytical paraclinical test in order to confirm that the complication was not infected.
As a secondary diagnosis for the basic lesions examined in the dermis, it was determined that the clinical condition corresponds to non-infectious complications due to implantation in the incorrect plane, with the suture located on the surface. The chosen treatment involved infiltrating non cross-linked hyaluronic acid along the suture to induce its hydrolysis, rather than surgery to remove the thread.
After a local anaesthetic, the treatment approach involved using cannulas along the implanted thread to deposit non cross-linked hyaluronic acid, adding the greatest volume in the furthest zone from its insertion. This was all undertaken with the aim of quickly inducing suture degradation in order to rapidly resolve the aesthetic and inflammatory complications affecting the patient.
The patient was indicated to continue the non-steroidal anti-inflammatory drug treatment prescribed by the doctor that implanted the polydioxanone threads (ketorolac 20 milligrams administered under the tongue every eight hours) for three days. The clinical treatment, injecting non cross-linked hyaluronic acid, began 24 hours after the complication occurred, administering 0.5 millilitres of non-cross-linked hyaluronic acid. The procedure was repeated after 21 and 45 days.
During this period, the patient was advised to avoid massaging the affected area, placing warm or cold compresses, applying creams or ointments, applying pressure on her right side during sleep, and to clean the area of the incision furthest away from the thread using distilled water and antiseptic liquid soap every day, followed by covering the wound with latex-free hypoallergenic adhesive tape.
The follow up after seven, 21, and 45 days showed a positive and gradual evolution of the area treated with hyaluronic acid, initially noted as a reduction of the oedema, then a reduction in the number and depth of skin irregularities and folds deriving from the traction due to the thread fixation, as well as the skin redensifying in the area with numerous secondary rhytids before the operation (Figure 2).
Figure 2. Clinical evidence of progress at 7, 21, and 45 days respectively.
Additionally, a blood test was performed on a segment of the polydioxanone thread prior to establishing the treatment plan. The test consisted of a degradation test or in vitro hydrolysis in a medium containing non cross-linked hyaluronic to enable the macroscopic observation of its dilution in that medium.
A similar polydioxanone thread fragment to the one implanted in the patient was subjected to placement in a Petri dish for biological samples at 37 degrees Celsius for subsequent observation in a laminar flow cabinet and through an optical microscope. The one centimetre long 21G gauge polydioxanone thread segment was immersed in 1.5 millilitres of undiluted non cross-linked hyaluronic acid.
It was observed using an ultramicroscope at 4x and 10x after 24, 48, and 72 hours. The microphotographs at 24 hours already showed evidence of structural changes in the fibres with increased interlaminar spaces and dilution of the violet pigment. The degradation continued at 48 hours, observing polydioxanone hygroscopy in the form of an aqueous content between the thread’s peripheral layers and its central core. There was evidence some fibre breakage and an increase in interlaminar and interfibrillar spaces (Figure 3).
Figure 3. Polydioxanone thread after 48 hours immersed in hyaluronic acid.
At 72 hours it had diluted in the medium, the release of the pigment indicating more extensive empty spaces in the thread’s central column, observing the disorganisation of the “frayed” peripheral fibrils throughout the fibre (Figure 4).
Discussion
The reported case introduces a new treatment, applied to a patient that requested medical attention for presenting exanthematous dermatosis, derived from the incorrect implantation of barbed polydioxanone threads in her midface. The treatment involved infiltrating non cross-linked hyaluronic acid along the suture to induce its hydrolysis, rather than surgery to remove the thread. The treatment choice was based on previous results from an in vitro test undertaken by the authors of this case study to verify the degradation or hydrolysis of the polydioxanone thread in a medium containing non cross-linked hyaluronic acid. The aforementioned suture dilution was observed under a microscope at 48 and 72 hours from its incubation.
The polydioxanone thread implanted in the patient of this case study was not found inserted in the superficial musculoaponeurotic system or in the hypodermis. It was placed on the surface of the dermis, with palpation possible, causing the complications in the patient. This lead to the need to apply the technique as described in the literature. One of the most recent authors[8] recommends inserting the threads at an angle or vertically downwards, with lifting vectors aimed towards the temporal or zygomatic zone to enable significant lifting of the cheek and mandibular contour. They emphasise that polydioxanone threads should be inserted into the superficial musculoaponeurotic system area. The entry and/or exit points are likely to coincide with the areas where the retaining ligaments are located, increasing their consistency and enabling targeting their objective. As a result, facial lifting with threads should not pose any risks of complication, as long as both the technique and facial anatomy is properly understood. This is a very important aspect, particularly when the limits between the planes are almost virtual and the depths between planes are only a question of millimetres.
When it comes to complications after inserting threads, similar studies to this case have shown that barbed type threads have caused most complications. The incidence is high, with around 69% of adverse events associated with barbed thread implants[17]. Other authors[5] also found a high number of patients (27%) experienced what could be considered minimal or moderate complications, which did not leave any permanent sequalae. The most common complication involves skin dimples and irregularities (11.4%), followed by ecchymosis (8.1%), suture extrusion (2.7%), pain (2.7%), and suture migration (1.35%), which resolved without assistance in almost every patient within three to seven days. This is in line with the complications presented by the patient in this case report, although no suture migration or extrusion occurred.
It is maintained that the achieved lifting effect derived more from the technique used rather than the thread itself. Despite being widely accepted, adverse events can occur after their implantation that have a major impact on the development of the patient in question[18], as occurred with the patient whose case is presented in this article. Given the high morbidity associated with using barbed threads, some authors recommend observing the patient for the first 72 hours after implantation. They are placed differently in the hypodermis to the smooth or coiled types and strong reactions may occur up to four weeks after being placed[19].
Few systematic studies compiling a review of the absorbable sutures used for lifting and their complications exist[17],[20],[21],[22]. The absorbable sutures used in these studies were made from polydioxanone, polylactic acid, and caprolactone. The aforementioned complications can be attributed to the material’s composition, the design of the suture, and/or the procedure itself[5].
In accordance with previous studies, a commonly observed complication when inserting barbed polydioxanone threads involves the formation of skin dimples and irregularities. Skin traction with dimpling has been linked to incorrect suture placement or insertion too close to the surface[23], which is exactly what occurred with this clinical case, as the patient presented retraction dimples because of the superficial insertion of the suture. In this respect, Hochman et al.[6] suggested that dimples at the far end of the suture can be avoided by not exiting transcutaneously and ensuring that the suture is not placed too close to the dermis inside the malar fat pad. If the complication lasts for weeks, undertaking a subcision of the area with the problem is recommended so that the defect disappears without assistance. The estimated recovery after that procedure can be at least seven days[14].
In this case, the patient experienced most of the aforementioned complications associated with the thread’s morphology and thread insertion technique faults, apart from infection. This coincided with the described authors[4],[5],[6],[15],[17],[20],[21],[22] with a clinical picture comprising of oedema, large ecchymoses, thread palpation, skin irregularities, skin dimples and traction folds. These derived from implanting the suture in the incorrect plane, placing it on the surface of the epidermis.
Large ecchymoses, local infection, and thread protrusion / palpation are also often common complications after implanting barbed threads even when they are absorbable. Ecchymoses resolve themselves after a few weeks without requiring treatment. Local infections are common at the point of intersection or where the thread enters. In most cases, treatment involves removing the threads from the infected site. Thread protrusion or palpation is treated by partially removing the thread[4]. Some experts suggest making a small incision of one to two millimetres in the skin to remove and extract it using a Gillis skin hook, gripping the thread gently in order to cut and remove it[23]. This surgical treatment and its slow recovery period differs from that applied to the reviewed case, which offers a minimally invasive alternative for the complications. The proposed technique only involves infiltrating hyaluronic acid along the thread, which induces hydrolysis of the suture, means it loses strength and detaches from the tissues, improving all the observed symptoms.
Furthermore, even though this protocol is becoming widely used by facial aesthetics professionals, hyaluronic acid should not be injected along the thread when performing lifting therapy with a polydioxanone suture as there is no scientific evidence for this practice. On the contrary, from a biochemical point of view, applying hyaluronic acid to a very hydrolytic suture does not make sense, as adding this molecule will promote more and faster thread degradation. This process was witnessed in vivo with the evolution of the affected area in the patient in this clinical case, and in vitro with the test undertaken on the suture immersed in hyaluronic acid, which showed the hydrolytic degradation of polydioxanone.
The only experience of the conjugation of a suture thread with hyaluronic acid was published by Sudhir et al.[24], who evaluated the effectiveness of silk sutures and polyglycolic acid sutures treated with hyaluronic acid to reduce bacterial colonisation. Their results show the enzymatic or catalysing action of hyaluronic acid on these sutures and that the chemical treatment of suture materials with enzyme solutions, such as hyaluronic acid, significantly reduces the bacterial colonisation of the suture through capillary action. This occurs because the suture absorbs and chemically binds to the hyaluronic acid, which occupies the interstitial spaces inside the suture thread filaments, preventing bacteria from colonising there. These authors[24] also suggest testing different suture materials in future investigations, incubating them for over 24 hours to evaluate the impact of treating the suture with hyaluronic acid. This will provide a better understanding of the physical and biological properties of absorption for the different suture materials. This is all in line with the investigation hypothesis we followed before applying the treatment, when undertaking the in vitro polydioxanone in hyaluronic acid degradation test.
Although polydioxanone reabsorbs in 180 days and its residual effect can remain for two years[23], it was possible to initiate its degradation 24 hours after the hyaluronic acid injection therapy for the case reported here. Despite the polydioxanone thread not being correctly attached in this case, administering hyaluronic acid in three phases turned out to be an effective technique for inducing rapid thread biodegradation. This did not lead to a reduction in the support that the doctor achieved when applying the vector in a zygomatic direction, which was sustained by some correctly inserted thread sections in the hypodermic plane.
The clinical hypothesis that we derive from this experience suggests that non cross-linked hyaluronic acid is a potent catalysing agent[24] of polydioxanone hydrolytic degradation, given that it is highly hydrophilic. This derives from the chemical bond between the hyaluronic acid and the polymeric chains comprising the suture[25]. Polydioxanone absorbs at least 0.5% water, even at temperatures below 24 degrees Celsius, and it shows little resistance to diluted acids. This means that combining non cross-linked hyaluronic acid with polydioxanone reduces the chemical resistance of the suture’s biopolymer, possibly shortening the chains or opening bonds in the monomer, enabling greater uptake of aqueous substances into the polydioxanone structure[25]. The bond between polydioxanone and hyaluronic acid may derive from a third type of compound that is biochemically responsible for degrading the suture, mimicking the role of lipase[25], an enzyme traditionally responsible for degrading the polydioxanone polymer.
The constant uptake of water by the hyaluronic acid molecules into the suture means more ions capable of causing interlaminar and interfibrillar structural changes inside the thread are added. Those changes manage to reduce its deformation tensile modulus until the thread fails or splits, mainly in the amorphous regions of the material’s fibrillar microstructure. This idea is reinforced in some studies[26],[27] conducted outside the aesthetic medicine field, which focus on the basic investigation of biomaterials. Other works measured morphological changes in polydioxanone sutures, in terms of their mechanical and chemical properties, when the polydioxanone suture is subjected to hydration, degrading as a function of time[28],[29].
Hyaluronic acid may be well known in facial aesthetics as a biopolymer for skin filling, but the polymer has many other applications as a therapeutic agent[30]. This is why the authors, for this clinical case, consider that the recovery observed in the patient may be partly down to the tissue restructuring therapeutic properties of hyaluronic acid. Its therapeutic effects may derive from its identical composition to the glycosaminoglycans found in the extracellular matrix. This makes it a support or environment that promotes the attachment of molecules and proteins for cell signalling. These are responsible for coding for the production of sustaining element substances and for the molecular biostimulation of growth factors involved in tissue regeneration[31].
This is why, in addition to the suture hydrolysis, a large part of the beneficial effect observed in the patient in this case is also derived from tissue remodelling around the thread, induced by the hyaluronic acid infiltrated in the thread implantation area. In other words, a series of biological events involved with in vivo autologous tissue engineering was induced, which restructured the affected tissues.
Conclusions
In accordance with the symptomatic findings in the patient in this case (oedema, ecchymosis, thread surface palpation, skin dimpling or folding irregularities), the definitive diagnosis was exanthematous dermatosis due to iatrogenic lesion. In other words, basic lesions in the dermis deriving from non-infectious complications after the incorrect placement of the polydioxanone thread or its implantation in the wrong skin plane, with the suture placed too close to the surface.
Faced with the aforementioned complications, administering hyaluronic acid was effective in inducing the rapid clinical biodegradation of the thread. For this reason, based on the patient’s clinical evolution and the additional in vitro degradation test when deciding on the treatment plan, the derived hypothesis suggests that non cross-linked hyaluronic acid is a potent catalyst of hydrolytic polydioxanone degradation.
As a result, hyaluronic acid could be indicated for resolving complications deriving from polydioxanone lifting threads being placed at the surface, fulfilling the dual objective of accelerating the thread’s biodegradation and inducing the regeneration of the tissue around the suture.
Notes
Authors’ roles
DSV: conceptualisation, methodology, formal analysis, investigation, resources, writing and preparing the original project, writing, reviewing and editing, viewing, supervising, and management of the project.
GVM: conceptualisation, methodology, formal analysis, investigation, resources, writing and preparing the original project, writing, reviewing and editing, viewing, supervising, and management of the project.
VGG: conceptualisation, methodology, formal analysis, investigation, resources, writing and preparing the original project, writing, reviewing and editing, viewing, supervising, and management of the project.
VMK: conceptualisation, methodology, formal analysis, investigation, resources, writing and preparing the original project, writing, reviewing and editing, viewing, supervising, and management of the project.
KML: conceptualisation, methodology, formal analysis, investigation, resources, writing and preparing the original project, writing, reviewing and editing, viewing, supervising, and management of the project.
Acknowledgements
To Dr. Reynaldo Ortiz, PhD, electrochemistry laboratory professor in the Faculty of Sciences of the University of the Andes, for providing access to the laboratory’s installations to undertake and monitor the in vitro degradation test.
Ethical aspects
The patient signed the informed consent requested by Medwave. A copy was sent to the Journal’s publishing management.
Conflict of interests statement
The authors filled out the ICMJE conflicts of interests statement and declared that they did not receive funding for completing the report. They do not have any financial links with organisations that may have an interest in the published article within the last three years. They don’t have any other relationships or activities that may influence the published article either. The forms can be requested by contacting the lead author or the publishing committee at the Journal.
Funding statement
The authors state that there are no external funding sources.

 Figure 1. Female patient with an oedema and ecchymosis derived from unsuitable thread traction in zone 3 between the midface and lower right face.
Figure 1. Female patient with an oedema and ecchymosis derived from unsuitable thread traction in zone 3 between the midface and lower right face.

 Figure 2. Clinical evidence of progress at 7, 21, and 45 days respectively.
Figure 2. Clinical evidence of progress at 7, 21, and 45 days respectively.

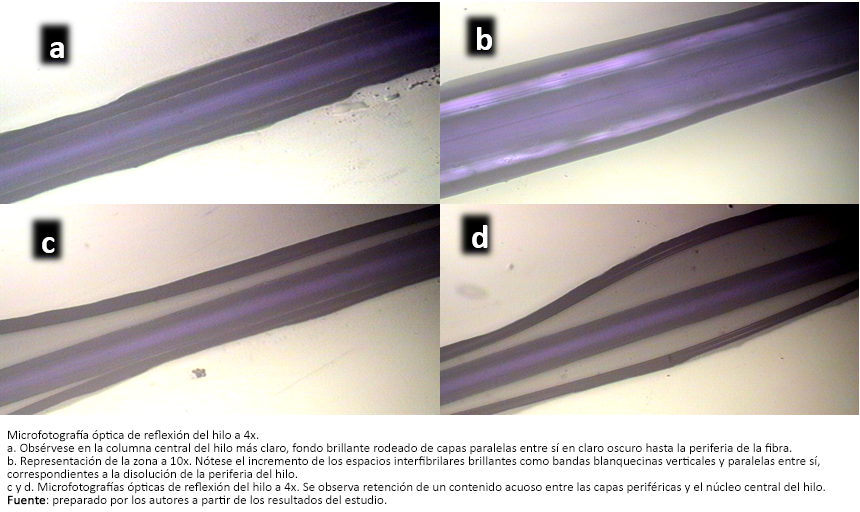 Figure 3. Polydioxanone thread after 48 hours immersed in hyaluronic acid.
Figure 3. Polydioxanone thread after 48 hours immersed in hyaluronic acid.

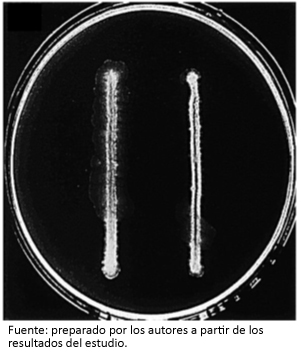 Figure 4. Onset of the polydioxanone fragment dilution at 72 hours immersed in a simulated medium with hyaluronic acid.
Figure 4. Onset of the polydioxanone fragment dilution at 72 hours immersed in a simulated medium with hyaluronic acid.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Se expone el caso de una paciente remitida por complicaciones posteriores a la implantación superficial en el tercio medio facial de hilos de polidioxanona espiculados. Presentaba edema, equimosis, palpación superficial del hilo y plicación dérmica. Para el tratamiento planteamos un novedoso protocolo de degradación clínica de hilos de polidioxanona, empleando ácido hialurónico inyectándolo en el área de su implantación. Se infiltró ácido hialurónico no reticulado en el trayecto a lo largo del recorrido del hilo. El seguimiento a los siete, 21 y 45 días evidenció disminución del edema, de los pliegues e irregularidades dérmicas por la tracción del hilo y atenuación de rítides secundarias. Una muestra del hilo en ácido hialurónico fue observado en campana de flujo laminar evidenciándose degradación a las 72 horas. Administrar ácido hialurónico fue efectivo para inducir la biodegradación clínica del hilo. La hipótesis derivada sugiere que el ácido hialurónico no reticulado es un poderoso catalizador de la degradación hidrolítica de la polidioxanona.
 Authors:
Dubraska Suárez-Vega[1], Gladys Velazco de Maldonado[1], Víctor García-Guevara[2], Blanca Miller-Kobisher[3], Katia Morena-López[4]
Authors:
Dubraska Suárez-Vega[1], Gladys Velazco de Maldonado[1], Víctor García-Guevara[2], Blanca Miller-Kobisher[3], Katia Morena-López[4]
Affiliation:
[1] Departamento de Investigación, Centro de Investigaciones Odontológicas, Universidad de Los Andes, Mérida, Venezuela
[2] Fundación Centro de Estudios de Medicina Estética (FUCEME), Caracas, Venezuela
[3] Instituto Panamericano de Profesionales Científicos (IPPC), Ciudad de México, México
[4] Asociación Salvadoreña de Medicina Estética y Longevidad (ASAMEL), San Salvador, El Salvador
E-mail: dubraskasuarez.ula@gmail.com
Author address:
[1] Facultad de Odontología
Departamento de Investigación Universidad de Los Andes
Calle 23 entre avenidas 2 y 3
Mérida
Venezuela

Citation: Suárez-Vega D, Velazco de Maldonado G, García-Guevara V, Miller-Kobisher B, Morena-López K. Microscopic and clinical evidence of the degradation of polydioxanone lifting threads in the presence of hyaluronic acid: a case report. Medwave 2019;19(1):e7575 doi: 10.5867/medwave.2019.01.7575
Submission date: 4/10/2018
Acceptance date: 15/1/2019
Publication date: 28/1/2019
Origin: not commissioned
Type of review: reviewed by two external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Ali YH. Two years' outcome of thread lifting with absorbable barbed PDO threads: Innovative score for objective and subjective assessment. J Cosmet Laser Ther. 2018 Feb;20(1):41-49. | CrossRef | PubMed |
- Ilankovan V. Recent Advances in Face Lift to Achieve Facial Balance. J Maxillofac Oral Surg. 2017 Mar;16(1):3-12. | CrossRef | PubMed |
- Tavares JP, Oliveira CACP, Torres RP, Bahmad F Jr. Facial thread lifting with suture suspension. Braz J Otorhinolaryngol. 2017 Nov - Dec;83(6):712-719. | CrossRef | PubMed |
- Sardesai MG, Zakhary K, Ellis DA. Thread-lifts: the good, the bad, and the ugly. Arch Facial Plast Surg. 2008 Jul-Aug;10(4):284-5. | CrossRef | PubMed |
- Sarigul Guduk S, Karaca N. Safety and complications of absorbable threads made of poly-L-lactic acid and poly lactide/glycolide: Experience with 148 consecutive patients. J Cosmet Dermatol. 2018 Dec;17(6):1189-1193. | CrossRef | PubMed |
- Hochman M. Midface barbed suture lift. Facial Plast Surg Clin North Am. 2007 May;15(2):201-7, vi. | CrossRef | PubMed |
- Sulamanidze M, Sulamanidze G, Vozdvizhenskiy I, Sulamanidze K, Kadzhaya A. New method of face elastic thread lift. Chapter 14. en: Miniinvasive Face and Body Lifts. IntechOpen; 2013:277-286. | CrossRef |
- De las Heras C. Técnicas antiptosis con hilos de suspensión subdérmica. Revista de la Asociación de Medicina Estética de Castilla- La Mancha (AMECLM) 2014;4:17-21. | Link |
- Jang HJ, Lee WS, Hwang K, Park JH, Kim DJ. Effect of cog threads under rat skin. Dermatol Surg. 2005 Dec;31(12):1639-43; discussion 1644. | PubMed |
- Kurita M, Matsumoto D, Kato H, Araki J, Higashino T, Fujino T, et al. Tissue reactions to cog structure and pure gold in lifting threads: a histological study in rats. Aesthet Surg J. 2011 Mar;31(3):347-51. | CrossRef | PubMed |
- Kim J, Kim HS, Seo JM, Nam KA, Chung KY. Evaluation of a novel thread-lift for the improvement of nasolabial folds and cheek laxity. J Eur Acad Dermatol Venereol. 2017 Mar;31(3):e136-e179. | CrossRef | PubMed |
- San Román, J. Polímeros biodegradables de interés en cirugía I: síntesis, propiedades y mecanismos biodegradativos. Revista de Plásticos Modernos. 1990;413:689-704. | Link |
- Roby MS, Kennedy J. Sutures. Biomaterials Science – An Introduction to materials in medicine, 2nd Edition. Elsevier Academic Press, 2004:614-627. | Link |
- Mototsugu Fukaya. Long-term effect of the insoluble thread-lifting technique. Clinical, Cosmetic and Investigational Dermatology 2017; 10:483-491. | CrossRef |
- Cornette de Saint Cyr B, Benouaiche L. [Face rejuvenation with tensor threads]. Ann Chir Plast Esthet. 2017 Oct;62(5):488-494. | CrossRef | PubMed |
- García V, Velazco G, Miller B. Complicación con hilos de polidioxanona por ruptura de la mucosa bucal. Reporte de un caso. Acta Bioclínica. 2018;8(16):212-220. | Link |
- Rachel JD, Lack EB, Larson B. Incidence of complications and early recurrence in 29 patients after facial rejuvenation with barbed suture lifting. Dermatol Surg. 2010 Mar;36(3):348-54. | CrossRef | PubMed |
- Bisaccia E, Kadry R, Rogachefsky A, Saap L, Scarborough DA. Midface lift using a minimally invasive technique and a novel absorbable suture. Dermatol Surg. 2009 Jul;35(7):1073-8; discussion 1078. | CrossRef | PubMed |
- Savoia A, Accardo C, Vannini F, Di Pasquale B, Baldi A. Outcomes in thread lift for facial rejuvenation: a study performed with happy lift™ revitalizing. Dermatol Ther (Heidelb). 2014 Jun;4(1):103-14. | CrossRef | PubMed |
- Suh DH, Jang HW, Lee SJ, Lee WS, Ryu HJ. Outcomes of polydioxanone knotless thread lifting for facial rejuvenation. Dermatol Surg. 2015 Jun;41(6):720-5. | CrossRef | PubMed |
- Baek WI, Kim WS, Suh JH, Kim BJ. Lower Facial Rejuvenation Using Absorbable Casting Barbed Thread. Dermatol Surg. 2017 Jun;43(6):884-887. | CrossRef | PubMed |
- Sulamanidze, M; Sulamanidze, G; Vozdvizhensky,I ; Sulamanidze C. Avoiding Complications With Aptos Sutures. Aesthet Surg J. 2011 Nov;31(8):863-73. | PubMed |
- De Masi E, De Masi F, De Masi R. Suspension Threads. Facial Plast Surg. 2016 Dec;32(6):662-663. | CrossRef | PubMed |
- Sudhir VR, Biju T, Ramesh A, Ergieg S, Fanas SA, Desai V, et al. Effect of Hyaluronic Acid Added to Suture Material and its Relationship with Bacterial Colonization: An In vitro Study. J Int Soc Prev Community Dent. 2018 Sep-Oct;8(5):391-395. | CrossRef | PubMed |
- George Wypych. PDS polydioxanone. En Handbook of Polymers (Second Edition). Canada. ChemTec Publishing; 2016: 346-348. | CrossRef |
- Peterlin A. Morphology and properties of crystalline polymers with fiber structure. Text Res J 1972;42:20. | CrossRef |
- Ping Ooi C, Cameron RE. The hydrolytic degradation of polydioxanone (PDSII) sutures. Part I: Morphological aspects. J Biomed Mater Res. 2002;63(3):280-90. | CrossRef | PubMed |
- Molea G, Schonauer F, Bifulco G, D'Angelo D. Comparative study on biocompatibility and absorption times of three absorbable monofilament suture materials (Polydioxanone, Poliglecaprone 25, Glycomer 631). Br J Plast Surg. 2000 Mar;53(2):137-41. | CrossRef | PubMed |
- Ping Ooi C, Cameron RE. The hydrolytic degradation of polydioxanone (PDSII) sutures. Part II: Micromechanisms of deformation. J Biomed Mater Res. 2002;63(3):291-8. | CrossRef | PubMed |
- Neuman M, Nanau RM, Oruña-Sanchez L, Coto G. Hyaluronic Acid and Wound Healing. J Pharm Pharm Sci. 2015;18(1):53-60. | PubMed |
- Sudha PN, Rose MH. Beneficial effects of hyaluronic acid. Adv Food Nutr Res. 2014;72:137-176. | CrossRef | PubMed |
 Ali YH. Two years' outcome of thread lifting with absorbable barbed PDO threads: Innovative score for objective and subjective assessment. J Cosmet Laser Ther. 2018 Feb;20(1):41-49. | CrossRef | PubMed |
Ali YH. Two years' outcome of thread lifting with absorbable barbed PDO threads: Innovative score for objective and subjective assessment. J Cosmet Laser Ther. 2018 Feb;20(1):41-49. | CrossRef | PubMed | Ilankovan V. Recent Advances in Face Lift to Achieve Facial Balance. J Maxillofac Oral Surg. 2017 Mar;16(1):3-12. | CrossRef | PubMed |
Ilankovan V. Recent Advances in Face Lift to Achieve Facial Balance. J Maxillofac Oral Surg. 2017 Mar;16(1):3-12. | CrossRef | PubMed | Tavares JP, Oliveira CACP, Torres RP, Bahmad F Jr. Facial thread lifting with suture suspension. Braz J Otorhinolaryngol. 2017 Nov - Dec;83(6):712-719. | CrossRef | PubMed |
Tavares JP, Oliveira CACP, Torres RP, Bahmad F Jr. Facial thread lifting with suture suspension. Braz J Otorhinolaryngol. 2017 Nov - Dec;83(6):712-719. | CrossRef | PubMed | Sardesai MG, Zakhary K, Ellis DA. Thread-lifts: the good, the bad, and the ugly. Arch Facial Plast Surg. 2008 Jul-Aug;10(4):284-5. | CrossRef | PubMed |
Sardesai MG, Zakhary K, Ellis DA. Thread-lifts: the good, the bad, and the ugly. Arch Facial Plast Surg. 2008 Jul-Aug;10(4):284-5. | CrossRef | PubMed | Sarigul Guduk S, Karaca N. Safety and complications of absorbable threads made of poly-L-lactic acid and poly lactide/glycolide: Experience with 148 consecutive patients. J Cosmet Dermatol. 2018 Dec;17(6):1189-1193. | CrossRef | PubMed |
Sarigul Guduk S, Karaca N. Safety and complications of absorbable threads made of poly-L-lactic acid and poly lactide/glycolide: Experience with 148 consecutive patients. J Cosmet Dermatol. 2018 Dec;17(6):1189-1193. | CrossRef | PubMed | Hochman M. Midface barbed suture lift. Facial Plast Surg Clin North Am. 2007 May;15(2):201-7, vi. | CrossRef | PubMed |
Hochman M. Midface barbed suture lift. Facial Plast Surg Clin North Am. 2007 May;15(2):201-7, vi. | CrossRef | PubMed | Sulamanidze M, Sulamanidze G, Vozdvizhenskiy I, Sulamanidze K, Kadzhaya A. New method of face elastic thread lift. Chapter 14. en: Miniinvasive Face and Body Lifts. IntechOpen; 2013:277-286. | CrossRef |
Sulamanidze M, Sulamanidze G, Vozdvizhenskiy I, Sulamanidze K, Kadzhaya A. New method of face elastic thread lift. Chapter 14. en: Miniinvasive Face and Body Lifts. IntechOpen; 2013:277-286. | CrossRef | De las Heras C. Técnicas antiptosis con hilos de suspensión subdérmica. Revista de la Asociación de Medicina Estética de Castilla- La Mancha (AMECLM) 2014;4:17-21. | Link |
De las Heras C. Técnicas antiptosis con hilos de suspensión subdérmica. Revista de la Asociación de Medicina Estética de Castilla- La Mancha (AMECLM) 2014;4:17-21. | Link | Jang HJ, Lee WS, Hwang K, Park JH, Kim DJ. Effect of cog threads under rat skin. Dermatol Surg. 2005 Dec;31(12):1639-43; discussion 1644. | PubMed |
Jang HJ, Lee WS, Hwang K, Park JH, Kim DJ. Effect of cog threads under rat skin. Dermatol Surg. 2005 Dec;31(12):1639-43; discussion 1644. | PubMed | Kurita M, Matsumoto D, Kato H, Araki J, Higashino T, Fujino T, et al. Tissue reactions to cog structure and pure gold in lifting threads: a histological study in rats. Aesthet Surg J. 2011 Mar;31(3):347-51. | CrossRef | PubMed |
Kurita M, Matsumoto D, Kato H, Araki J, Higashino T, Fujino T, et al. Tissue reactions to cog structure and pure gold in lifting threads: a histological study in rats. Aesthet Surg J. 2011 Mar;31(3):347-51. | CrossRef | PubMed | Kim J, Kim HS, Seo JM, Nam KA, Chung KY. Evaluation of a novel thread-lift for the improvement of nasolabial folds and cheek laxity. J Eur Acad Dermatol Venereol. 2017 Mar;31(3):e136-e179. | CrossRef | PubMed |
Kim J, Kim HS, Seo JM, Nam KA, Chung KY. Evaluation of a novel thread-lift for the improvement of nasolabial folds and cheek laxity. J Eur Acad Dermatol Venereol. 2017 Mar;31(3):e136-e179. | CrossRef | PubMed | San Román, J. Polímeros biodegradables de interés en cirugía I: síntesis, propiedades y mecanismos biodegradativos. Revista de Plásticos Modernos. 1990;413:689-704. | Link |
San Román, J. Polímeros biodegradables de interés en cirugía I: síntesis, propiedades y mecanismos biodegradativos. Revista de Plásticos Modernos. 1990;413:689-704. | Link | Roby MS, Kennedy J. Sutures. Biomaterials Science – An Introduction to materials in medicine, 2nd Edition. Elsevier Academic Press, 2004:614-627. | Link |
Roby MS, Kennedy J. Sutures. Biomaterials Science – An Introduction to materials in medicine, 2nd Edition. Elsevier Academic Press, 2004:614-627. | Link | Mototsugu Fukaya. Long-term effect of the insoluble thread-lifting technique. Clinical, Cosmetic and Investigational Dermatology 2017; 10:483-491. | CrossRef |
Mototsugu Fukaya. Long-term effect of the insoluble thread-lifting technique. Clinical, Cosmetic and Investigational Dermatology 2017; 10:483-491. | CrossRef | Cornette de Saint Cyr B, Benouaiche L. [Face rejuvenation with tensor threads]. Ann Chir Plast Esthet. 2017 Oct;62(5):488-494. | CrossRef | PubMed |
Cornette de Saint Cyr B, Benouaiche L. [Face rejuvenation with tensor threads]. Ann Chir Plast Esthet. 2017 Oct;62(5):488-494. | CrossRef | PubMed | García V, Velazco G, Miller B. Complicación con hilos de polidioxanona por ruptura de la mucosa bucal. Reporte de un caso. Acta Bioclínica. 2018;8(16):212-220. | Link |
García V, Velazco G, Miller B. Complicación con hilos de polidioxanona por ruptura de la mucosa bucal. Reporte de un caso. Acta Bioclínica. 2018;8(16):212-220. | Link | Rachel JD, Lack EB, Larson B. Incidence of complications and early recurrence in 29 patients after facial rejuvenation with barbed suture lifting. Dermatol Surg. 2010 Mar;36(3):348-54. | CrossRef | PubMed |
Rachel JD, Lack EB, Larson B. Incidence of complications and early recurrence in 29 patients after facial rejuvenation with barbed suture lifting. Dermatol Surg. 2010 Mar;36(3):348-54. | CrossRef | PubMed | Bisaccia E, Kadry R, Rogachefsky A, Saap L, Scarborough DA. Midface lift using a minimally invasive technique and a novel absorbable suture. Dermatol Surg. 2009 Jul;35(7):1073-8; discussion 1078. | CrossRef | PubMed |
Bisaccia E, Kadry R, Rogachefsky A, Saap L, Scarborough DA. Midface lift using a minimally invasive technique and a novel absorbable suture. Dermatol Surg. 2009 Jul;35(7):1073-8; discussion 1078. | CrossRef | PubMed | Savoia A, Accardo C, Vannini F, Di Pasquale B, Baldi A. Outcomes in thread lift for facial rejuvenation: a study performed with happy lift™ revitalizing. Dermatol Ther (Heidelb). 2014 Jun;4(1):103-14. | CrossRef | PubMed |
Savoia A, Accardo C, Vannini F, Di Pasquale B, Baldi A. Outcomes in thread lift for facial rejuvenation: a study performed with happy lift™ revitalizing. Dermatol Ther (Heidelb). 2014 Jun;4(1):103-14. | CrossRef | PubMed | Suh DH, Jang HW, Lee SJ, Lee WS, Ryu HJ. Outcomes of polydioxanone knotless thread lifting for facial rejuvenation. Dermatol Surg. 2015 Jun;41(6):720-5. | CrossRef | PubMed |
Suh DH, Jang HW, Lee SJ, Lee WS, Ryu HJ. Outcomes of polydioxanone knotless thread lifting for facial rejuvenation. Dermatol Surg. 2015 Jun;41(6):720-5. | CrossRef | PubMed | Baek WI, Kim WS, Suh JH, Kim BJ. Lower Facial Rejuvenation Using Absorbable Casting Barbed Thread. Dermatol Surg. 2017 Jun;43(6):884-887. | CrossRef | PubMed |
Baek WI, Kim WS, Suh JH, Kim BJ. Lower Facial Rejuvenation Using Absorbable Casting Barbed Thread. Dermatol Surg. 2017 Jun;43(6):884-887. | CrossRef | PubMed | Sulamanidze, M; Sulamanidze, G; Vozdvizhensky,I ; Sulamanidze C. Avoiding Complications With Aptos Sutures. Aesthet Surg J. 2011 Nov;31(8):863-73. | PubMed |
Sulamanidze, M; Sulamanidze, G; Vozdvizhensky,I ; Sulamanidze C. Avoiding Complications With Aptos Sutures. Aesthet Surg J. 2011 Nov;31(8):863-73. | PubMed | De Masi E, De Masi F, De Masi R. Suspension Threads. Facial Plast Surg. 2016 Dec;32(6):662-663. | CrossRef | PubMed |
De Masi E, De Masi F, De Masi R. Suspension Threads. Facial Plast Surg. 2016 Dec;32(6):662-663. | CrossRef | PubMed | Sudhir VR, Biju T, Ramesh A, Ergieg S, Fanas SA, Desai V, et al. Effect of Hyaluronic Acid Added to Suture Material and its Relationship with Bacterial Colonization: An In vitro Study. J Int Soc Prev Community Dent. 2018 Sep-Oct;8(5):391-395. | CrossRef | PubMed |
Sudhir VR, Biju T, Ramesh A, Ergieg S, Fanas SA, Desai V, et al. Effect of Hyaluronic Acid Added to Suture Material and its Relationship with Bacterial Colonization: An In vitro Study. J Int Soc Prev Community Dent. 2018 Sep-Oct;8(5):391-395. | CrossRef | PubMed | George Wypych. PDS polydioxanone. En Handbook of Polymers (Second Edition). Canada. ChemTec Publishing; 2016: 346-348. | CrossRef |
George Wypych. PDS polydioxanone. En Handbook of Polymers (Second Edition). Canada. ChemTec Publishing; 2016: 346-348. | CrossRef | Peterlin A. Morphology and properties of crystalline polymers with fiber structure. Text Res J 1972;42:20. | CrossRef |
Peterlin A. Morphology and properties of crystalline polymers with fiber structure. Text Res J 1972;42:20. | CrossRef | Ping Ooi C, Cameron RE. The hydrolytic degradation of polydioxanone (PDSII) sutures. Part I: Morphological aspects. J Biomed Mater Res. 2002;63(3):280-90. | CrossRef | PubMed |
Ping Ooi C, Cameron RE. The hydrolytic degradation of polydioxanone (PDSII) sutures. Part I: Morphological aspects. J Biomed Mater Res. 2002;63(3):280-90. | CrossRef | PubMed | Molea G, Schonauer F, Bifulco G, D'Angelo D. Comparative study on biocompatibility and absorption times of three absorbable monofilament suture materials (Polydioxanone, Poliglecaprone 25, Glycomer 631). Br J Plast Surg. 2000 Mar;53(2):137-41. | CrossRef | PubMed |
Molea G, Schonauer F, Bifulco G, D'Angelo D. Comparative study on biocompatibility and absorption times of three absorbable monofilament suture materials (Polydioxanone, Poliglecaprone 25, Glycomer 631). Br J Plast Surg. 2000 Mar;53(2):137-41. | CrossRef | PubMed | Ping Ooi C, Cameron RE. The hydrolytic degradation of polydioxanone (PDSII) sutures. Part II: Micromechanisms of deformation. J Biomed Mater Res. 2002;63(3):291-8. | CrossRef | PubMed |
Ping Ooi C, Cameron RE. The hydrolytic degradation of polydioxanone (PDSII) sutures. Part II: Micromechanisms of deformation. J Biomed Mater Res. 2002;63(3):291-8. | CrossRef | PubMed | Neuman M, Nanau RM, Oruña-Sanchez L, Coto G. Hyaluronic Acid and Wound Healing. J Pharm Pharm Sci. 2015;18(1):53-60. | PubMed |
Neuman M, Nanau RM, Oruña-Sanchez L, Coto G. Hyaluronic Acid and Wound Healing. J Pharm Pharm Sci. 2015;18(1):53-60. | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








