Key Words: type II choledochal cyst, Roux-en-Y anastomosis
Abstract
Choledochal cyst is a rare pathological condition, which represents 1% of benign diseases of the biliary tract. It is seen with significant frequency in childhood, with a higher prevalence in females, and a greater diagnostic incidence in Asia. Diagnosis is primarily based on clinical suspicion. Its symptoms are variable, and its treatment, depending on the type, is surgical. Case report: a male patient, 46 years old, with clinical symptoms of acute pancreatitis as a complication of a choledochal cyst Todani type II is diagnosed during his hospital stay with cholangial magnetic resonance. The patient recovers from the acute episode and undergoes a cystectomy with biliodigestive liver-jejunum bypass and a Roux-Y anastomosis.
Introduction
Over the last few years, the advent of the technological era has made possible a greater access to diagnosis of several abdominal pathologies. Bile duct cysts, despite being uncommon conditions, cause a series of symptoms which may lead to confusing diagnoses. Therefore, the fact of knowing these pathological alterations, as well as their classification, clinical presentation and eventual solution will enhance the range of diagnostic hypotheses, with a lesser failure rate and clinical complications in patients, thus helping them improve their health condition.
Choledochal cyst is a pathological condition conventionally represented as a complex congenital malformation that involves different degrees of dilation of both the common bile duct and the pancreatic duct [1],[2]. However, it has also been suggested that it may be a consequence of an acquired condition that is incidental to the abnormal joining of the aforementioned ducts [3].
Choledochal cyst is an infrequent condition that represents 1% of the benign diseases of the bile duct [4], whose estimated incidence varies according to the geographical region studied. One out of 1000 cases are reported in some countries in Asia, mainly Japan; one out of two million inhabitants in European countries such as England, one out of 150,000 in the west and one out of 13,500 in America, mainly the United States of America. It has a clear preference for females in most of the cases [5],[6],[7],[8]. This is a reality confirmed in one of the greatest retrospective reviews carried out in the American region by the Vancouver General Hospital in Canada. This review identified a total of 51 cases in a term of 17 years, 80% of which were females [9].
The hypotheses about its formation include the congenital stenosis of the bile duct, whose partial obstruction derives on an increase of the intraluminal pressure and its eventual dilation. Furthermore, the Babbitt Hypothesis [10],[11], which is a physiopathological consequence of the abnormal joining of the bile duct and the pancreatic duct, resulting in pancreatic reflux, and increase of intraluminal pressure of the bile duct and distention thereof [6],[7],[8],[9],[10],[11],[12]. Such reality has been reproduced in animal models through anastomosis of the bile duct, where it is observed a progressive dilation thereof, which is also considered as an acquired etiological factor.
In 1995, Alonso-Lej, et al., based on a series of 94 cases, established the first classification, which was transformed in 1997 by Todani, et al., and, since then, it has been modified by several authors (Table 1) [4],[13].
Table 1. Classification of choledochal cysts.
Case presentation
Patient J.L.B.B., male, aged 46, with a background of depression without current pharmacological treatment, with bile duct prosthesis applied in 2002 for non-specified causes, cholecystectomy and extraction of the bile duct prosthesis in 2013. The patient presented repeated jaundice, and three episodes of acute cholangitis and pancreatitis. On January 30th, 2016, he was admitted to the Urgency Room of San Juan de Dios de Curicó Hospital, upon being referred from Licantén Hospital due to a 3-day long epigastric upper abdominal pain that radiates to the back, which does not respond to intravenous analgesia and is associated to vomiting. When the patient was admitted skin and mucous were anicteric, abdomen soft and depressible, sensitive to palpation, diffusely predominant on the epigastrium, with absent abdominal sounds.
The requested laboratory tests reported as follows: leukocytes 20,8x10^3/uL, C-reactive protein 3.90 mg/dl, alkaline phosphatase 289.40U/L, total bilirubin 4,31mg/dl, indirect bilirubin 1.34 mg/dl, direct bilirubin 2.97 mg/dl, serum amylase 664 U/L and lipase 1521,5U/L, as well as abdominal and pelvic computed tomography scan with contrast, whose findings suggest acute pancreatitis, and dilation of the intra- and extrahepatic bile ducts. Therefore, it is not possible to discard choledocholithiasis and a small left renal cyst, whereby hospitalization for handling and study of his pathology is decided.
During hospitalization, an abdominal echotomography was requested (Figure 1) which shows a dilation of the intra- and extrahepatic bile ducts, aerobilia, dilated bile duct of approximately 15.7 mm with some small inner echogenic images that may correspond to choledocholithiasis and suggestive signs of acute pancreatitis, without free abdominal fluid. Moreover, a cholangiopancreatography was performed (Figure 2), which shows a low, centered dilation of the intrahepatic bile duct, of the confluence and common bile duct, associated to a cystic image dependent on the middle third of the bile duct with a lateral projection, which reaches a size of 2.2 x 1.3 x 1.3cm in diameter, thus corresponding to a Todani type II classification.
Upon resolution of the patient’s clinical presentation of acute pancreatitis, it was decided to perform a cystectomy with a biliodigestive derivation and Roux-en-Y hepaticojejunostomy, as shown in Figure 3. The patient showed a hassle-free, favorable postoperative development, thus being discharged from hospital seven days after surgery. Fifteen days later in the same place outpatient control he showed no clinical complications. The biopsy report showed benign histology compatible with choledochal cyst.
Figure 1. Ultrasound showing a dilated bile duct.
Figure 2. Cholangiopancreatography showing a cyst in the bile duct.
Discussion
The choledochal cyst, based on its main etiologic mechanism, is usually diagnosed during childhood. Fifty percent of reported cases are diagnosed in the first ten years of life; however, 20% correspond to a late diagnosis, and half of them are recognized during adulthood through symptoms related to a bile duct pathology [15]. Given the facts shown in this case, it could be presumed that his diagnosis during adulthood responds to an eventual acquired condition, which is incidental to medical procedures rather to a congenital origin.
Bile duct cysts are associated to an increased risk of cancer, particularly cholangiocarcinoma, which considerably increases with age. It is associated to pediatric age patients in less than 1% of the cases, in contrast to those observed during adulthood, in which frequency ranges between 10 and 30%, even reaching 50% in patients older than 50 years of age, who have a poor survival rate. Evolution towards neoplasia is more common in patients with type I and IV cysts, and it is less frequent in patients with type II cysts, as the abovementioned case, who can be treated with a simple cyst excision [5],[16].
Diagnosis is mainly based on clinical suspicion. Some authors state that for adults the main symptom is abdominal pain, other authors propose that it is the typical triad characterized by jaundice, mass in right hypochondrium and abdominal pain, which is evidenced between 13% and 65% of the studied cases. However, there are new authors supporting pancreatitis as predominant clinical presentation, which is observed in 10% of the cases [17],[18]. Regarding the study methods, abdominal echography can determine up to 92% of the cases of cystic malformations of the bile duct, in which is described a diagnostic sensitivity between 71% and 97%, thus being able to precisely determine the size, contour and location of the cysts. This is a non-invasive, low-cost method, among other advantages; but, its results are observer-dependent.
One alternative includes an endoscopic ultrasonography, which allows a good visualization of the choledochal intrapancreatic portion. However, its limiting factor is the width of the equipment. The pelvic and abdominal CAT scan, which is useful in defining its size, location and continuity of the anomaly in the biliary tree, reaches a sensibility of 93%. Finally, the endoscopic retrograde cholangiopancreatography (ERCP) is able to define lower ductal anatomy and, specifically, the presence of abnormal joining between the bile duct and the pancreatic duct of Wirsung. Nevertheless, its disadvantages lie in the complications inherent to the procedure [17],[19]. Currently, the nuclear magnetic cholangiopancreatography (NMCP) may substitute endoscopic retrograde cholangiopancreatography, since it is a non-invasive exploration with lesser complications, and with a reported diagnosis certainty close to 100% in the study of choledochal cyst; however, it fails to be therapeutic [20],[21].
Handling patients with choledochal cysts depends on the type thereof. However, in general terms, the treatment of choice consists of complete excision of the cyst associated to cholecystectomy, with a reconstruction of the bile duct through a Roux-en-Y hepaticojejunostomy [22],[23]. Usually, during this procedure it is preferred to use the traditional open surgery approach, which is not free of risks. Thus, the approach in current clinical practice tends to use minimally invasive surgeries, such as videolaparoscopy, which was incorporated in 1995 and there is an everyday evidence of cases successfully treated with this technique [24].
For patients with type II cyst, as in the case already exposed, whose risk of association with malignant transformation is extremely low, it is estimated that diverticulectomy by simple excision is sufficient [14]. However, patients with complicated clinical presentations, such as jaundice or malignancy in the cyst, may require a more extensive resection [25]. This is why, based on clinical signs, anatomical location and the experience of our service, we estimated that the surgical management used was the most appropriate.
Conclusions
As described, choledochal cysts are part of a complicated disease entity, over which there are still many debates. Based on the current classification system, different subtypes have different characteristics, from anatomy itself to carcinogenesis. The Todani Type II choledochal cyst is a rare entity, with low risk of malignancy, and whose etiology, classically shown as congenital, may have an acquired causal variant. This has been demonstrated in animal models, in which the bile duct has been altered, thus presenting secondarily dilation and cyst formation.
Nowadays, due to technological advances in imaging methods of the bile duct, a greater number of correct diagnoses is performed. However, there is still a large group of patients whose diagnosis is made during adulthood based on their clinical complications, which leads to think if it is a congenital cause with late diagnosis or, conversely, its etiology is rather the product of triggering or acquired factors, as the ones already mentioned. For this reason, it is extremely important to consider the association between cystic disease of the bile duct as a cause of various abdominal clinical presentations, in order to perform a timely diagnosis and management, thus avoiding complications and maintaining the health condition of patients.
Notes
From the editor
The authors originally submitted this article in Spanish and English. The Journal has not copyedited the English version.
Ethical aspects
The patient signed the informed consent requested by Medwave. A copy was sent to the Journal editorial board.
Conflicts of interest
The authors completed the ICMJE conflicts of interest declaration form, translated to Spanish by Medwave, and declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years, and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Funding
The authors declare that there was no funding coming from external sources.

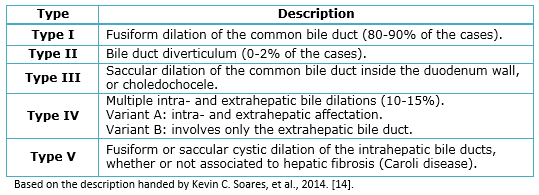 Table 1. Classification of choledochal cysts.
Table 1. Classification of choledochal cysts.

 Figure 1. Ultrasound showing a dilated bile duct.
Figure 1. Ultrasound showing a dilated bile duct.

 Figure 2. Cholangiopancreatography showing a cyst in the bile duct.
Figure 2. Cholangiopancreatography showing a cyst in the bile duct.

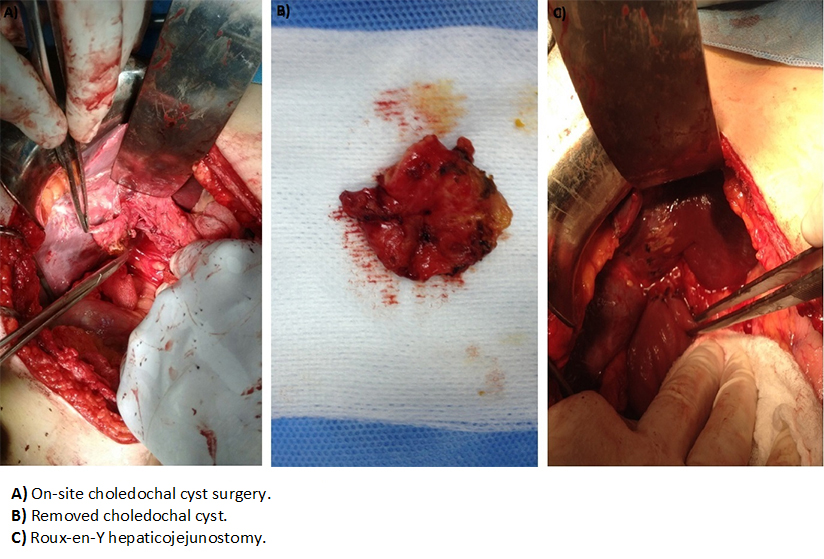 Figure 3. Choledochal cyst.
Figure 3. Choledochal cyst.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

El quiste de colédoco es una condición patológica poco usual, que representa el 1% de las enfermedades benignas de la vía biliar. Se observa con significativa frecuencia durante la edad pediátrica, con prevalencia en el sexo femenino y mayor incidencia diagnóstica en el continente asiático. Su diagnóstico se basa principalmente en la sospecha clínica, cuya sintomatología es variable. Su resolución, que depende del tipo, es quirúrgica. Se presenta el caso clínico de un paciente masculino, 46 años, con cuadro clínico de pancreatitis aguda como complicación de quiste de colédoco Todani tipo II, diagnosticado durante su estancia hospitalaria con colangioresonancia. Evolucionó con resolución de su cuadro agudo favorablemente, por lo que se decidió quistectomía con derivación biliodigestiva hepático-yeyuno anastomosis en Y de Roux.
 Authors:
Solange Marcela Farías Molina [1], Rafael Lisandro Castillo Machado [2 ], Natalia Carolina Sanhueza Palma [1 ], Jeannette Alejandra Calzadilla Riveras [1 ]
Authors:
Solange Marcela Farías Molina [1], Rafael Lisandro Castillo Machado [2 ], Natalia Carolina Sanhueza Palma [1 ], Jeannette Alejandra Calzadilla Riveras [1 ]
Affiliation:
[1] Escuela de Medicina, Universidad de Talca, Hospital San Juan de Dios, Curicó, Chile
[2] Servicio de Cirugía, Hospital San Juan de Dios, Curicó, Chile
E-mail: solangefariasmolina@gmail.com
Author address:
[1] Bilbao 297
Curicó
Región del Maule
Chile

Citation: Farías Molina SM , Castillo Machado RL , Sanhueza Palma NC , Calzadilla Riveras JA . Todani choledochal cyst type II: case report and review. Medwave 2016 Oct;16(9):6583 doi: 10.5867/medwave.2016.09.6583
Submission date: 17/5/2016
Acceptance date: 25/9/2016
Publication date: 20/10/2016
Origin: not requested
Type of review: reviewed by five external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Iwai N, Yanagihara J, Tokiwa K, Shimotake T, Nakamura K. Congenital choledochal dilatation with emphasis on pathophysiology of the biliary tract. Ann Surg. 1992 Jan;215(1):27-30. | PubMed |
- Vivas G, Millán A, De Agustín J. Optimización en la estrategia diagnóstica y terapéutica en el quiste de colédoco. Rev Chil Cir. 2015;67(3):278-284. | Link |
- Han SJ, Hwang EH, Chung KS, Kim MJ, Kim H. Acquired choledochal cyst from anomalous pancreatobiliary duct union. J Pediatr Surg. 1997 Dec;32(12):1735-8. | PubMed |
- Ruiz M, Brenes D, Ayi J. Quiste de colédoco. Revista Médica de Costa Rica y Centroamérica, 2011;596:49-56. | Link |
- Jiménez M, Soria V, Martín J, Olalla J, Giménez A, Alcaraz E, et al. Quiste de colédoco tipo II intrapancreático del adulto malignizado: duodenopancreatectomía. Rev Esp Enferm Dig, 2014;106(3):223-226. | Link |
- Martínez-Ordaz JL, Niño-Solís J. Choledochal cysts in adults. Cir Cir. 2010 Jan-Feb;78(1):61-6. | PubMed |
- O'Neill JA Jr. Choledochal cyst. Curr Probl Surg. 1992 Jun;29(6):361-410. | PubMed |
- Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can J Surg. 2009 Oct;52(5):434-40. | PubMed |
- Wiseman K, Buczkowski AK, Chung SW, Francoeur J, Schaeffer D, Scudamore CH. Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg. 2005 May;189(5):527-31. | PubMed |
- Cha SW, Park MS, Kim KW, Byun JH, Yu JS, Kim MJ, et al. Choledochal cyst and anomalous pancreaticobiliary ductal union in adults: radiological spectrum and complications. J Comput Assist Tomogr. 2008 Jan-Feb;32(1):17-22. | CrossRef | PubMed |
- Han SJ, Hwang EH, Chung KS, Kim MJ, Kim H. Acquired choledochal cyst from anomalous pancreatobiliary duct union. J Pediatr Surg. 1997 Dec;32(12):1735-8. | PubMed |
- Oneil N, Chopra P, Al-Zadjali A, Younas S. Choledochal Cyst in Adults: Etiopathogenesis, Presentation, Management, and Outcome—Case Series and Review. Gastroenterology Research and Practice. 2015;602591:1-10. | Link |
- Jiménez M, Romero R, Romero J. Quistes de colédoco: una enfermedad infrecuente con muchas facetas. RADP online. 2010;33(3):249-252. | Link |
- Siahaya FJ, Lalisang TJ, Jeo WS, Simanjuntak AB, Philippi B. Uncommon Mixed Type I and II Choledochal Cyst: An Indonesian Experience. Case Rep Surg. 2013;2013:821032. | CrossRef | PubMed |
- Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, et al. Choledochal cysts: presentation, clinical differentiation, and management. J Am Coll Surg. 2014 Dec;219(6):1167-80. | CrossRef | PubMed |
- Law R, Topazian M. Diagnosis and treatment of choledochoceles. Clin Gastroenterol Hepatol. 2014 Feb;12(2):196-203. | CrossRef | PubMed |
- Olivera D, García M. Quiste de colédoco. Presentación de un caso. Medisur. 2012;10(3):241-244. | Link |
- Enríquez L, Díaz J, Cabrera E, Gutiérrez P, Aguayo B. Pancreatitis aguda como presentación de un quiste del conducto biliar en el adulto: reporte de caso. Rev Fac Med. 2009;57(1):63-66. | Link |
- Arrieta A, Manzano A, Navarro D, Durango R. Dilema en el diagnóstico de quiste de colédoco. Reporte de un caso. Revista GEN (Gastroenterología Nacional). 2011;65(3):237-239. | Link |
- Uribarrena Amezaga R, Raventós N, Fuentes J, Elías J, Tejedo V, Uribarrena Echebarría R. [Diagnosis and management of choledochal cysts. A review of 10 new cases]. Rev Esp Enferm Dig. 2008 Feb;100(2):71-5. | PubMed |
- Ortega X, Guelfand M. Caso clínico radiológico: quiste de colédoco. Rev Med Clin Condes. 2009; 20(6):911-914. | Link |
- Jabłońska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol. 2012 Sep 21;18(35):4801-10. | PubMed |
- Díaz J, Parada F, Rencoret G, Hodgson F, Aldunate C, Anziani F. Quiste gigante de colédoco. Rev Chil Cir.2007;59(1):3-4. | CrossRef |
- Lu B, Shen Z, Yu J, Yang J, Tang H, Ma H. Laparoscopic surgery for removal of choledochal cysts and Roux-en-Y anastomosis. Int J Clin Exp Med. 2015 Aug 15;8(8):13013-6. | PubMed |
- Ouaïssi M, Kianmanesh R, Belghiti J, Ragot E, Mentha G, Adham M, et al. Todani Type II Congenital Bile Duct Cyst: European Multicenter Study of the French Surgical Association and Literature Review. Ann Surg. 2015 Jul;262(1):130-8. | CrossRef | PubMed |
 Iwai N, Yanagihara J, Tokiwa K, Shimotake T, Nakamura K. Congenital choledochal dilatation with emphasis on pathophysiology of the biliary tract. Ann Surg. 1992 Jan;215(1):27-30. | PubMed |
Iwai N, Yanagihara J, Tokiwa K, Shimotake T, Nakamura K. Congenital choledochal dilatation with emphasis on pathophysiology of the biliary tract. Ann Surg. 1992 Jan;215(1):27-30. | PubMed | Vivas G, Millán A, De Agustín J. Optimización en la estrategia diagnóstica y terapéutica en el quiste de colédoco. Rev Chil Cir. 2015;67(3):278-284. | Link |
Vivas G, Millán A, De Agustín J. Optimización en la estrategia diagnóstica y terapéutica en el quiste de colédoco. Rev Chil Cir. 2015;67(3):278-284. | Link | Han SJ, Hwang EH, Chung KS, Kim MJ, Kim H. Acquired choledochal cyst from anomalous pancreatobiliary duct union. J Pediatr Surg. 1997 Dec;32(12):1735-8. | PubMed |
Han SJ, Hwang EH, Chung KS, Kim MJ, Kim H. Acquired choledochal cyst from anomalous pancreatobiliary duct union. J Pediatr Surg. 1997 Dec;32(12):1735-8. | PubMed | Ruiz M, Brenes D, Ayi J. Quiste de colédoco. Revista Médica de Costa Rica y Centroamérica, 2011;596:49-56. | Link |
Ruiz M, Brenes D, Ayi J. Quiste de colédoco. Revista Médica de Costa Rica y Centroamérica, 2011;596:49-56. | Link | Jiménez M, Soria V, Martín J, Olalla J, Giménez A, Alcaraz E, et al. Quiste de colédoco tipo II intrapancreático del adulto malignizado: duodenopancreatectomía. Rev Esp Enferm Dig, 2014;106(3):223-226. | Link |
Jiménez M, Soria V, Martín J, Olalla J, Giménez A, Alcaraz E, et al. Quiste de colédoco tipo II intrapancreático del adulto malignizado: duodenopancreatectomía. Rev Esp Enferm Dig, 2014;106(3):223-226. | Link | Martínez-Ordaz JL, Niño-Solís J. Choledochal cysts in adults. Cir Cir. 2010 Jan-Feb;78(1):61-6. | PubMed |
Martínez-Ordaz JL, Niño-Solís J. Choledochal cysts in adults. Cir Cir. 2010 Jan-Feb;78(1):61-6. | PubMed | Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can J Surg. 2009 Oct;52(5):434-40. | PubMed |
Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can J Surg. 2009 Oct;52(5):434-40. | PubMed | Wiseman K, Buczkowski AK, Chung SW, Francoeur J, Schaeffer D, Scudamore CH. Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg. 2005 May;189(5):527-31. | PubMed |
Wiseman K, Buczkowski AK, Chung SW, Francoeur J, Schaeffer D, Scudamore CH. Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg. 2005 May;189(5):527-31. | PubMed | Cha SW, Park MS, Kim KW, Byun JH, Yu JS, Kim MJ, et al. Choledochal cyst and anomalous pancreaticobiliary ductal union in adults: radiological spectrum and complications. J Comput Assist Tomogr. 2008 Jan-Feb;32(1):17-22. | CrossRef | PubMed |
Cha SW, Park MS, Kim KW, Byun JH, Yu JS, Kim MJ, et al. Choledochal cyst and anomalous pancreaticobiliary ductal union in adults: radiological spectrum and complications. J Comput Assist Tomogr. 2008 Jan-Feb;32(1):17-22. | CrossRef | PubMed | Han SJ, Hwang EH, Chung KS, Kim MJ, Kim H. Acquired choledochal cyst from anomalous pancreatobiliary duct union. J Pediatr Surg. 1997 Dec;32(12):1735-8. | PubMed |
Han SJ, Hwang EH, Chung KS, Kim MJ, Kim H. Acquired choledochal cyst from anomalous pancreatobiliary duct union. J Pediatr Surg. 1997 Dec;32(12):1735-8. | PubMed | Oneil N, Chopra P, Al-Zadjali A, Younas S. Choledochal Cyst in Adults: Etiopathogenesis, Presentation, Management, and Outcome—Case Series and Review. Gastroenterology Research and Practice. 2015;602591:1-10. | Link |
Oneil N, Chopra P, Al-Zadjali A, Younas S. Choledochal Cyst in Adults: Etiopathogenesis, Presentation, Management, and Outcome—Case Series and Review. Gastroenterology Research and Practice. 2015;602591:1-10. | Link | Jiménez M, Romero R, Romero J. Quistes de colédoco: una enfermedad infrecuente con muchas facetas. RADP online. 2010;33(3):249-252. | Link |
Jiménez M, Romero R, Romero J. Quistes de colédoco: una enfermedad infrecuente con muchas facetas. RADP online. 2010;33(3):249-252. | Link | Siahaya FJ, Lalisang TJ, Jeo WS, Simanjuntak AB, Philippi B. Uncommon Mixed Type I and II Choledochal Cyst: An Indonesian Experience. Case Rep Surg. 2013;2013:821032. | CrossRef | PubMed |
Siahaya FJ, Lalisang TJ, Jeo WS, Simanjuntak AB, Philippi B. Uncommon Mixed Type I and II Choledochal Cyst: An Indonesian Experience. Case Rep Surg. 2013;2013:821032. | CrossRef | PubMed | Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, et al. Choledochal cysts: presentation, clinical differentiation, and management. J Am Coll Surg. 2014 Dec;219(6):1167-80. | CrossRef | PubMed |
Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, et al. Choledochal cysts: presentation, clinical differentiation, and management. J Am Coll Surg. 2014 Dec;219(6):1167-80. | CrossRef | PubMed | Law R, Topazian M. Diagnosis and treatment of choledochoceles. Clin Gastroenterol Hepatol. 2014 Feb;12(2):196-203. | CrossRef | PubMed |
Law R, Topazian M. Diagnosis and treatment of choledochoceles. Clin Gastroenterol Hepatol. 2014 Feb;12(2):196-203. | CrossRef | PubMed | Olivera D, García M. Quiste de colédoco. Presentación de un caso. Medisur. 2012;10(3):241-244. | Link |
Olivera D, García M. Quiste de colédoco. Presentación de un caso. Medisur. 2012;10(3):241-244. | Link | Enríquez L, Díaz J, Cabrera E, Gutiérrez P, Aguayo B. Pancreatitis aguda como presentación de un quiste del conducto biliar en el adulto: reporte de caso. Rev Fac Med. 2009;57(1):63-66. | Link |
Enríquez L, Díaz J, Cabrera E, Gutiérrez P, Aguayo B. Pancreatitis aguda como presentación de un quiste del conducto biliar en el adulto: reporte de caso. Rev Fac Med. 2009;57(1):63-66. | Link | Arrieta A, Manzano A, Navarro D, Durango R. Dilema en el diagnóstico de quiste de colédoco. Reporte de un caso. Revista GEN (Gastroenterología Nacional). 2011;65(3):237-239. | Link |
Arrieta A, Manzano A, Navarro D, Durango R. Dilema en el diagnóstico de quiste de colédoco. Reporte de un caso. Revista GEN (Gastroenterología Nacional). 2011;65(3):237-239. | Link | Uribarrena Amezaga R, Raventós N, Fuentes J, Elías J, Tejedo V, Uribarrena Echebarría R. [Diagnosis and management of choledochal cysts. A review of 10 new cases]. Rev Esp Enferm Dig. 2008 Feb;100(2):71-5. | PubMed |
Uribarrena Amezaga R, Raventós N, Fuentes J, Elías J, Tejedo V, Uribarrena Echebarría R. [Diagnosis and management of choledochal cysts. A review of 10 new cases]. Rev Esp Enferm Dig. 2008 Feb;100(2):71-5. | PubMed | Ortega X, Guelfand M. Caso clínico radiológico: quiste de colédoco. Rev Med Clin Condes. 2009; 20(6):911-914. | Link |
Ortega X, Guelfand M. Caso clínico radiológico: quiste de colédoco. Rev Med Clin Condes. 2009; 20(6):911-914. | Link | Jabłońska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol. 2012 Sep 21;18(35):4801-10. | PubMed |
Jabłońska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol. 2012 Sep 21;18(35):4801-10. | PubMed | Díaz J, Parada F, Rencoret G, Hodgson F, Aldunate C, Anziani F. Quiste gigante de colédoco. Rev Chil Cir.2007;59(1):3-4. | CrossRef |
Díaz J, Parada F, Rencoret G, Hodgson F, Aldunate C, Anziani F. Quiste gigante de colédoco. Rev Chil Cir.2007;59(1):3-4. | CrossRef | Lu B, Shen Z, Yu J, Yang J, Tang H, Ma H. Laparoscopic surgery for removal of choledochal cysts and Roux-en-Y anastomosis. Int J Clin Exp Med. 2015 Aug 15;8(8):13013-6. | PubMed |
Lu B, Shen Z, Yu J, Yang J, Tang H, Ma H. Laparoscopic surgery for removal of choledochal cysts and Roux-en-Y anastomosis. Int J Clin Exp Med. 2015 Aug 15;8(8):13013-6. | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








