Key Words: carbamazepine, drug eruptions, maculopapular drug eruption, DRESS syndrome
Abstract
Carbamazepine is a frequently used drug that can produce adverse reactions like vertigo, somnolence and severe skin reactions like Drug Rash with Eosinophilia and Systemic Symptoms Syndrome (DRESS Syndrome). This syndrome is characterized by a late-appearing, slow-progressing cutaneous eruption accompanied by atypical lymphocytes, eosinophilia, and systemic symptoms such as fever, lymphadenopathy, hepatic compromise, and renal dysfunction that can be severe enough to cause death. We present a case that aims to highlight the importance of an early diagnosis of DRESS syndrome to adjust therapy and improve survival. The patient is a female patient prescribed carbamazepine for trigeminal neuralgia who presented with skin lesions, which were initially attributed to a hypersensitivity reaction. The lesions worsened in spite of treatment and systemic symptoms ensued. A diagnosis of DRESS syndrome was proposed and steroid treatment was initiated with rapid improvement.
Introduction:
Carbamazepine is a drug frequently prescribed for treating multiple conditions like epilepsy, trigeminal and glossopharyngeal neuralgia, post-herpetic neuritis, diabetic neuropathy and other severe pain symptoms associated to neurological disorders [1].
In most of these cases prolonged treatments are required in order to achieve the therapeutic objective. Consequently, side effects frequently appear, and sometimes even adverse reactions like vertigo, drowsiness, ataxia, nystagmus, and generalized erythematous skin rash [1],[2].
Occasionally a real entity can show up, like the acute generalized exanthematous pustulosis, the Stevens Johnson Syndrome or Toxic Epidermis Necrosis, pathologies that present themselves with systemic conditions that could lead to the patient’s death [3],[4].
The term “DRESS” was initially proposed in 1996 by Bocquet et al. to refer to a skin reaction caused by the effect of some drugs, accompanied by eosinophilia and systemic symptoms. Thereby, it could be differentiated from the drug-induced pseudo lymphoma described by Saltzstein and Ackerman in 1959 [5].
This entity has a late start and a slow and prolonged course, with an incidence of one out of 1000 to one out of 10 000 patients having a drug reaction, and represents a diagnosis challenge because of the variety of ways in which it can appear [6]. This is why we present this case, in order to highlight the importance of the DRESS Syndrome’s early diagnosis which guarantees the correct therapy to achieve the patient’s survival.
Case presentation
The case is a 60 year old female patient who started with pain in the face that felt like “lashes” at the right mental foramen level without any other symptoms. She is treated with analgesics and anti-inflammatory non-steroidal drugs in her health center, having a quick relief.
A few days after finishing the treatment, the patient starts with pain in the same place again; this time it was more intense and it spread to the rest of the face. Therefore, she turns to the maxillofacial surgery services where a trigeminal neuralgia, third branch, is diagnosed and a treatment with carbamazepine, 200 mg every 8 hours, is prescribed.
Two months after initiating the treatment with carbamazepine, the patient returns with hyperchromic maculopapular skin lesions located in the upper limbs and face. The lesions are accompanied by a light edema limited to the lips, and pruritus (Figure 1). In view of the manifestations, hypersensitivity to carbamazepine is diagnosed, the treatment with this drug is suspended and a systemic antihistaminic is prescribed.

Figure 1. Skin reaction to carbamazepine in a patient with DRESS Syndrome.
Three days later, the patient arrives with a 39 degrees fever, discomfort and more skin injuries. These symptoms led to complementary tests. A skin biopsy is carried out and a dermatologist is consulted, diagnosing her with the DRESS Syndrome because of the clinical manifestations and the test results (Table 1)
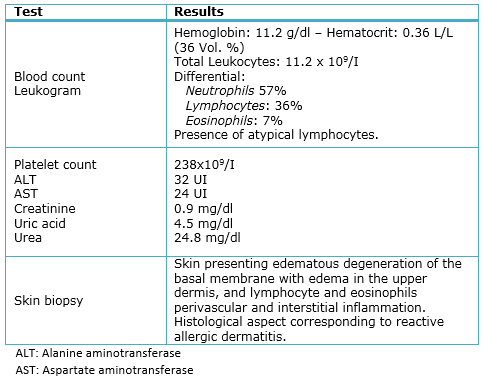
Table 1. Complementary test results of a patient diagnosed with the DRESS Syndrome.
The patient starts a treatment with prednisone 20 mg every 8 hours for three days, which was then reduced to 10 mg every 8 hours, 5 mg every 8 hours, then every 12 hours and finally daily. Each change was prescribed every 3 days. In addition, the patient had to apply triamcinolone to the affected area twice a day.

Figure 2: Skin condition after finishing the treatment.
The treatment for trigeminal neuralgia consisted in infiltrations in the surrounding areas at mandibular foramen level, near the Spix’s spine, in the internal side of the jaw, with 0.5 ml of 95% alcohol and 0.5 ml of 2% lidocaine. The inferior dental branch, which is the third trigeminal branch, is blocked at mental foramen level where it emerges in the front portion of the jaw, at first and second premolar level, specifically in the right side. With this treatment, her condition improved in only two sessions with a week interval between them.
Discussion
The World Health Organization (WHO) defines adverse reaction to drugs as the harmful, unintended response to a medicine, which occurs as it is administered in normal doses for an illness’ prophylaxis, diagnosis or treatment, or to modify a physiological function [7].
Adverse skin reactions can affect between 2 and 7% of the patients under systemic treatments, being carbamazepine and antimicrobials the drugs most likely to cause them. These reactions are a very serious health problem for patients who present them, it is estimated that they cause 6.7% of the deaths in the US, 6.5% in the UK and 3% in Switzerland [8].
Hypersensitivity reactions to carbamazepine are classified as type B and cannot be predicted because they are not dose-related and affect only a minority of the patients. They have to do specifically with the host characteristics which cannot be reproduced in animals [9].
Several mechanisms could explain these reactions, like the typical alterations of the drug’s metabolism, the high differential sensitivity to this metabolism toxic products and even immunological implications mediated by interleukin -5 [9],[10].
In patients who present hypersensitivity syndrome because of carbamazepine, several types of T cells are observed in the blood, including CD4 +, CD8 + y CD4-CD8 + cells related to the presence of the allele gen HLA-A*3101 [9],[11].
The DRESS Syndrome is one of the varieties of reactions to carbamazepine and, even though this entity’s prevalence is low, its diagnosis is to be considered because untreated patients may progress to death [12],[13].
The disease is more frequent in Latin-American black adults, both sexes similarly, although there have been some less frequent cases in pediatric ages and senior patients, which have turned out to be generally more severe [12],[13].
The clinical characteristics of the syndrome, as well as the methods for its definite diagnosis, are not yet well established because of the strange way in which it appears and the variable way of presentation, dermatologically speaking [10],[14].
Nevertheless, some of Bocquet’s criteria should be taken into account, which were used as reference by Philips et al., related to the clinical manifestations of a skin eruption due to medicine usage and to the result of complementary tests, like the presence of typical lymphocytes in peripheral blood, and an excessive count of eosinophils, similar to the case presented [5],[15].
Other clinical manifestations analogous to this case may appear, this is the case of fever, pruritus, generalized redness, edema and others like 2 cm or bigger lymphadenopathy, hepatic compromise with high transaminase, renal disorder caused by interstitial nephritis and pneumonitis or myocarditis [5],[14],[15].
Due to its multiple manifestations, some of them unspecific, it can be confused with adverse reactions to drugs (as it happened in the case presented) and with diseases with similar early symptoms, like scarlet fever and other skin exanthematous lesions described by Quintero Martínez and Muciño Bermejo [16],[17].
The early treatment of the DRESS syndrome includes immediate suspension of the drug, as it was done in this case, and the prescription of systemic steroids, not taken into account initially in this case. Some patients will require the administration of intravenous immunoglobulin, plasmapheresis or a combination of them [18].
It is important to highlight that many patients may require intensive treatment because of the systemic deterioration, with the objective of closely monitoring the patient’s progression watching the appearance of possible complications that could result in the patient’s death [19].
The presentation of the case considered the CARE guidelines for reporting clinical cases [20].
Conclusions
Not every skin injury in patients who start a treatment are an adverse reaction to the drug. In some cases it could be a true disease like the DRESS Syndrome.
In view of the appearance of systemic symptoms and an alteration in the differential series in a patient with an alleged skin reaction brought on by medication, a more severe clinical entity should be ruled out.
The suspension of the drug responsible for the DRESS Syndrome should be the first step to treat these patients, together with the systemic administration of steroids
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The patient signed the consent form requested by Medwave and a copy was sent to the Journal editorial board.
Conflicts of interest
The authors completed the ICMJE declaration of conflicts of interest, translated into Spanish by Medwave, and declare they have not received funding for the completion of the report; have no financial relationships with organizations that may have interests in the article published in the last three years; and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or editorial direction of the Journal.
Funding
The authors declare there are no external funding sources for this article.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

La carbamazepina es un medicamento de empleo habitual que puede producir efectos secundarios y en algunos casos reacciones adversas como vértigos, somnolencia y reacciones cutáneas que pueden ser severas como el síndrome DRESS (Drug Rash with Eosinophilia and Systemic Symptoms). Se caracteriza por erupción cutánea tardía y lenta progresión, linfocitos atípicos con eosinofilia y síntomas sistémicos como fiebre, adenopatías, hepatopatía y trastornos renales, pudiendo llegar a la muerte del paciente. Se presenta un caso para destacar la importancia del diagnóstico temprano del síndrome DRESS, que garantice un manejo adecuado para la supervivencia del paciente. Es una paciente bajo tratamiento con carbamazepina para neuralgia del trigémino, que al tiempo comienza con lesiones cutáneas que se interpretan como reacción de hipersensibilidad. Al no mejorar con tratamiento inicial y empeorar el cuadro cutáneo, acompañándose de síntomas generales, se realizan análisis complementarios y se plantea el diagnóstico de síndrome DRESS que se resuelve definitivamente con esteroides.
 Authors:
Emigdio Jesús Cabrera Fundora [1], Yuliet Cabrera Osorio [1], Claudia Cabrera Osorio [1]
Authors:
Emigdio Jesús Cabrera Fundora [1], Yuliet Cabrera Osorio [1], Claudia Cabrera Osorio [1]
Affiliation:
[1] Policlínico Hospital Alberto Fernández Valdés, Santa Cruz del Norte, Mayabeque, Cuba
E-mail: emigdio@infomed.sld.cu
Author address:
[1] Avenida 11
Edificio 22 A 27
Apartamento 1 Santa Cruz del Norte
Mayabeque
Cuba

Citation: Cabrera Fundora EJ, Cabrera Osorio Y, Cabrera Osorio C . Skin reaction to carbamazepine or DRESS syndrome: a case presentation. Medwave 2016 Feb;16(1):e6389 doi: 10.5867/medwave.2016.01.6389
Submission date: 7/11/2015
Acceptance date: 29/1/2016
Publication date: 25/2/2016
Origin: not requested
Type of review: reviewed by two external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Calvo Barbado DM, Delgado Martínez I, editores. Formulario Nacional de Medicamentos. 4ta ed. La Habana: Editorial Ciencias Médicas; 2014. | Link |
- Martínez Leiva A, Rivero León A, del Pozo Nistal Y. Uso y abuso en la prescripción de la carbamazepina en el Área Sur de Morón. Mediciego, 2012;18 (no. Esp) | Link |
- Roujeau JC, Stern RS. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994 Nov 10;331(19):1272-85. | PubMed |
- Chávez-Lemus FA, Reynoso-von Drateln C, Rodríguez-Martínez N. Prevalencia de las farmacodermias en pacientes hospitalizados en el Servicio de Dermatología de la UMAE del Centro Médico Nacional de Occidente. Periodo 2004-2012. Dermatol Rev Mex. 2014;58(4):339-45. | Link |
- Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996 Dec;15(4):250-7. | PubMed |
- Osuna Osuna J, Toledo Bahena ME, Valencia Herera A, Ramírez Cortés E, Mena Cedillos C. Reacción por drogas con eosinofilia: Síndrome DRESS, un gran simulador. Dermatología CMQ. 2013;11(2):142-7. | Link |
- Organización Mundial de la Salud. Medicamentos Esenciales y Productos de Salud. La seguridad de los medicamentos. Ginebra: OMS; 2003. | Link |
- Ferraz AV, Escasany AA, Xolvi CP, de Bolós JMA. Revisión sistemática de los estudios de evaluación del coste de las reacciones adversas a medicamentos. Gac Sanit. 2012;26(3): 277-83. | Link |
- Fricke-Galindo I, Jung-Cook B, LLerena A, López-López M. Farmacogenética de reacciones adversas a fármacos antiepilépticos. Neurología. 2015. De próxima aparición. | Link |
- Revuz J, Valeyrie-Allanore L. Drug Reactions. In: Bolognia JL, Jorizzo JL, Schaffer JV, Cerroni L, Heymann WR, Callen JP, editors. Dermatology. 2nd ed. Philadelphia: Elsevier Saunders; 2008: 335-356. | Link |
- McCormack M, Alfirevic A, Bourgeois S, Farrell JJ, Kasperavičiūtė D, Carrington M, et al. HLA-A*3101 and carbamazepine-induced hypersensitivity reactions in Europeans. N Engl J Med. 2011 Mar 24;364(12):1134-43. | CrossRef | PubMed |
- Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, Roujeau JC. The DRESS syndrome: a literature review. Am J Med. 2011 Jul;124(7):588-97. | CrossRef | PubMed |
- Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2011 Jan;36(1):6-11. | CrossRef | PubMed |
- Criado PR, Criado RFJ, Avancini JDM, Santi CD. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Drug-Induced Hypersensitivity Syndrome (DIHS): a review of current concepts. An Bras Dermatol. 2012; 87(3):435-49. | Link |
- Phillips EJ, Chung WH, Mockenhaupt M, Roujeau JC, Mallal SA. Drug hypersensitivity: pharmacogenetics and clinical syndromes. J Allergy Clin Immunol. 2011 Mar;127(3 Suppl):S60-6. | CrossRef | PubMed |
- Quintero-Martínez DC, Flores-Arizmendi RA, Torres-Rodríguez L. Síndrome de DRESS asociado con carbamazepina. Bol Med Hosp Infant Mex. 2015;72(2):118-23. | Link |
- Muciño-Bermejo J, Díaz de León-Ponce M, Briones-Vega CG, Guerrero-Hernández A, Sandoval-Ayala OI, Sáenz-Coronado AG, et al. Síndrome de DRESS. Reporte de un caso clínico. Rev Med Inst Mex Seguro Soc. 2013;51(3):330-5. | Link |
- Funck-Brentano E, Duong TA, Bouvresse S, Bagot M, Wolkenstein P, Roujeau J, et al. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72(2): 246-52. | Link |
- Darlenski R, Kazandjieva J, Tsankov N. Systemic drug reactions with skin involvement: Stevens-Johnson syndrome, toxic epidermal necrolysis, and DRESS. Clin Dermatol. 2015 Sep-Oct;33(5):538-41. | CrossRef | PubMed |
- Gagnier JJ, Riley D, Altman DG, Moher D, Sox H, Kienle G,er al. The CARE guidelines: consensus-based clinical case reporting guideline development. Dtsch Arztebl Int. 2013 Sep;110(37):603-8. | CrossRef | PubMed |
 Calvo Barbado DM, Delgado Martínez I, editores. Formulario Nacional de Medicamentos. 4ta ed. La Habana: Editorial Ciencias Médicas; 2014. | Link |
Calvo Barbado DM, Delgado Martínez I, editores. Formulario Nacional de Medicamentos. 4ta ed. La Habana: Editorial Ciencias Médicas; 2014. | Link | Martínez Leiva A, Rivero León A, del Pozo Nistal Y. Uso y abuso en la prescripción de la carbamazepina en el Área Sur de Morón. Mediciego, 2012;18 (no. Esp) | Link |
Martínez Leiva A, Rivero León A, del Pozo Nistal Y. Uso y abuso en la prescripción de la carbamazepina en el Área Sur de Morón. Mediciego, 2012;18 (no. Esp) | Link | Roujeau JC, Stern RS. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994 Nov 10;331(19):1272-85. | PubMed |
Roujeau JC, Stern RS. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994 Nov 10;331(19):1272-85. | PubMed | Chávez-Lemus FA, Reynoso-von Drateln C, Rodríguez-Martínez N. Prevalencia de las farmacodermias en pacientes hospitalizados en el Servicio de Dermatología de la UMAE del Centro Médico Nacional de Occidente. Periodo 2004-2012. Dermatol Rev Mex. 2014;58(4):339-45. | Link |
Chávez-Lemus FA, Reynoso-von Drateln C, Rodríguez-Martínez N. Prevalencia de las farmacodermias en pacientes hospitalizados en el Servicio de Dermatología de la UMAE del Centro Médico Nacional de Occidente. Periodo 2004-2012. Dermatol Rev Mex. 2014;58(4):339-45. | Link | Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996 Dec;15(4):250-7. | PubMed |
Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996 Dec;15(4):250-7. | PubMed | Osuna Osuna J, Toledo Bahena ME, Valencia Herera A, Ramírez Cortés E, Mena Cedillos C. Reacción por drogas con eosinofilia: Síndrome DRESS, un gran simulador. Dermatología CMQ. 2013;11(2):142-7. | Link |
Osuna Osuna J, Toledo Bahena ME, Valencia Herera A, Ramírez Cortés E, Mena Cedillos C. Reacción por drogas con eosinofilia: Síndrome DRESS, un gran simulador. Dermatología CMQ. 2013;11(2):142-7. | Link | Organización Mundial de la Salud. Medicamentos Esenciales y Productos de Salud. La seguridad de los medicamentos. Ginebra: OMS; 2003. | Link |
Organización Mundial de la Salud. Medicamentos Esenciales y Productos de Salud. La seguridad de los medicamentos. Ginebra: OMS; 2003. | Link | Ferraz AV, Escasany AA, Xolvi CP, de Bolós JMA. Revisión sistemática de los estudios de evaluación del coste de las reacciones adversas a medicamentos. Gac Sanit. 2012;26(3): 277-83. | Link |
Ferraz AV, Escasany AA, Xolvi CP, de Bolós JMA. Revisión sistemática de los estudios de evaluación del coste de las reacciones adversas a medicamentos. Gac Sanit. 2012;26(3): 277-83. | Link | Fricke-Galindo I, Jung-Cook B, LLerena A, López-López M. Farmacogenética de reacciones adversas a fármacos antiepilépticos. Neurología. 2015. De próxima aparición. | Link |
Fricke-Galindo I, Jung-Cook B, LLerena A, López-López M. Farmacogenética de reacciones adversas a fármacos antiepilépticos. Neurología. 2015. De próxima aparición. | Link | Revuz J, Valeyrie-Allanore L. Drug Reactions. In: Bolognia JL, Jorizzo JL, Schaffer JV, Cerroni L, Heymann WR, Callen JP, editors. Dermatology. 2nd ed. Philadelphia: Elsevier Saunders; 2008: 335-356. | Link |
Revuz J, Valeyrie-Allanore L. Drug Reactions. In: Bolognia JL, Jorizzo JL, Schaffer JV, Cerroni L, Heymann WR, Callen JP, editors. Dermatology. 2nd ed. Philadelphia: Elsevier Saunders; 2008: 335-356. | Link | McCormack M, Alfirevic A, Bourgeois S, Farrell JJ, Kasperavičiūtė D, Carrington M, et al. HLA-A*3101 and carbamazepine-induced hypersensitivity reactions in Europeans. N Engl J Med. 2011 Mar 24;364(12):1134-43. | CrossRef | PubMed |
McCormack M, Alfirevic A, Bourgeois S, Farrell JJ, Kasperavičiūtė D, Carrington M, et al. HLA-A*3101 and carbamazepine-induced hypersensitivity reactions in Europeans. N Engl J Med. 2011 Mar 24;364(12):1134-43. | CrossRef | PubMed | Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, Roujeau JC. The DRESS syndrome: a literature review. Am J Med. 2011 Jul;124(7):588-97. | CrossRef | PubMed |
Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, Roujeau JC. The DRESS syndrome: a literature review. Am J Med. 2011 Jul;124(7):588-97. | CrossRef | PubMed | Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2011 Jan;36(1):6-11. | CrossRef | PubMed |
Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2011 Jan;36(1):6-11. | CrossRef | PubMed | Criado PR, Criado RFJ, Avancini JDM, Santi CD. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Drug-Induced Hypersensitivity Syndrome (DIHS): a review of current concepts. An Bras Dermatol. 2012; 87(3):435-49. | Link |
Criado PR, Criado RFJ, Avancini JDM, Santi CD. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Drug-Induced Hypersensitivity Syndrome (DIHS): a review of current concepts. An Bras Dermatol. 2012; 87(3):435-49. | Link | Phillips EJ, Chung WH, Mockenhaupt M, Roujeau JC, Mallal SA. Drug hypersensitivity: pharmacogenetics and clinical syndromes. J Allergy Clin Immunol. 2011 Mar;127(3 Suppl):S60-6. | CrossRef | PubMed |
Phillips EJ, Chung WH, Mockenhaupt M, Roujeau JC, Mallal SA. Drug hypersensitivity: pharmacogenetics and clinical syndromes. J Allergy Clin Immunol. 2011 Mar;127(3 Suppl):S60-6. | CrossRef | PubMed | Quintero-Martínez DC, Flores-Arizmendi RA, Torres-Rodríguez L. Síndrome de DRESS asociado con carbamazepina. Bol Med Hosp Infant Mex. 2015;72(2):118-23. | Link |
Quintero-Martínez DC, Flores-Arizmendi RA, Torres-Rodríguez L. Síndrome de DRESS asociado con carbamazepina. Bol Med Hosp Infant Mex. 2015;72(2):118-23. | Link | Muciño-Bermejo J, Díaz de León-Ponce M, Briones-Vega CG, Guerrero-Hernández A, Sandoval-Ayala OI, Sáenz-Coronado AG, et al. Síndrome de DRESS. Reporte de un caso clínico. Rev Med Inst Mex Seguro Soc. 2013;51(3):330-5. | Link |
Muciño-Bermejo J, Díaz de León-Ponce M, Briones-Vega CG, Guerrero-Hernández A, Sandoval-Ayala OI, Sáenz-Coronado AG, et al. Síndrome de DRESS. Reporte de un caso clínico. Rev Med Inst Mex Seguro Soc. 2013;51(3):330-5. | Link | Funck-Brentano E, Duong TA, Bouvresse S, Bagot M, Wolkenstein P, Roujeau J, et al. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72(2): 246-52. | Link |
Funck-Brentano E, Duong TA, Bouvresse S, Bagot M, Wolkenstein P, Roujeau J, et al. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72(2): 246-52. | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








