Key Words: heart injuries, angioplasty, balloon, coronary, percutaneous coronary intervention
Abstract
Coronary perforation is a rare complication in patients undergoing percutaneous coronary angioplasty. The mortality of this complication varies depending on factors related to the patient and the procedure performed, reaching 44% in patients with Ellis type III perforation. We report the case of an 81 year old male with multiple cardiovascular risk factors, who underwent percutaneous angioplasty for high risk acute coronary syndrome (ACSs) Non-ST-Elevation Myocardial Infarction (NSTEMI) management. The patient developed grade III coronary perforation in the anterior descending artery, which was successfully managed with balloon inflation to 6 atmospheres for 10 minutes twice in the affected area, with an interval of 5 minutes between each dilatation. The patient improved and was discharged.
Background
Coronary perforation is an uncommon complication of percutaneous coronary intervention, which has an incidence between 0.19 and 0.56% [1],[2],[3]. According to the classification of Ellis et al. [4], there are four types of coronary perforation: type I, which refers to an extra luminal crater without contrast extravasation; type II or pericardial/myocardial blush without extravasation; type III or frank contrast extravasation through perforation and type IV or IIICS which refers to extravasation of contrast to anatomical cavities such as the coronary sinus [4]. The mortality rate in all types of coronary perforation is 7-17% and depends on several factors related to the perforation (Ellis type III, complex coronary anatomy) and the patient (elderly, prior myocardial infarction and hypertension) [1],[5],[6]; besides, this rate increases in 44% with type III perforation [7]. Generally, it has been described that for grade III coronary perforation management, the average time of balloon inflation is 48 minutes and require several times the use of other therapeutic options for achieving hemostasis [8].
We present the case of an 81-year-old patient successfully treated for type III coronary perforation following angioplasty with balloon inflation for 20 minutes and subsequent placement of stent in a private clinic in Lima, Peru.
Case report
An 81-year-old male patient from Lima diagnosed of coronary artery disease (chronic stable angina) with an ejection fraction of 69% at rest and post- stress, treated with enalapril, amlodipine, metformin, aspirin, clopidogrel, nitroglycerin in patch; and several cardiovascular risk factors (hypertension, type 2 diabetes mellitus, morbid obesity, dyslipidemia, and family history of coronary artery disease). He went to consult declaring an exacerbation of angina and was diagnosed with high risk acute coronary syndrome (ACSs) Non-ST-Elevation Myocardial Infarction (NSTEMI), with TIMI score 5 and GRACE (Global Registry of Acute Coronary Events) score 151 points. As a consequence, he underwent percutaneous coronary intervention. In coronariography, a segmental coronary lesion was found in anterior descending artery (80 % proximal third and 90% middle third) with signs of calcification (Figure 1), it was managed by angioplasty with placement of 02 medicated stents.
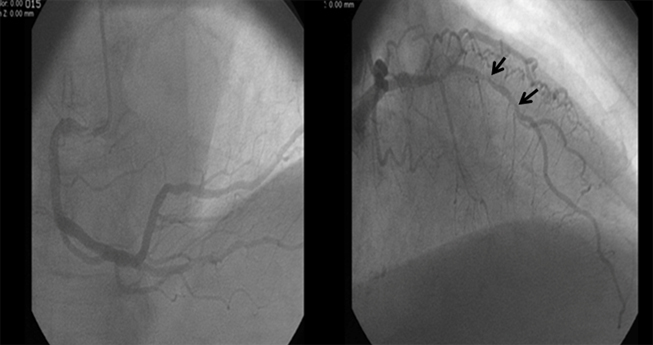
Figure 1. Coronary angiogram images. On the left, the right coronary artery and on the right, anterior descending artery previous to angioplasty
Procedure
Prior administration of 10,000 heparin units, angioplasty of the anterior descending artery was started by radial approach. A JL4 6F guiding catheter was placed, after contrast injection it was observed a segmental lesion of 80 % proximal and 90 % medium, these lesions were crossed with a 0.014'' Extrassuport guide for posterior dilatation of two balloons, the first of 1, 25 x 20 mm at 14 atm and the other 2,75x15mm at 10 atm at different levels of the obstruction. Subsequently, the medicated stent with Zotarolimus 2.75 x 14mm was deployed at distal middle third at 12 atm pressure. After stenting, contrast injection showed free extravasation compatible with coronary perforation in the middle/distal third portion of the stent (Figure 2).
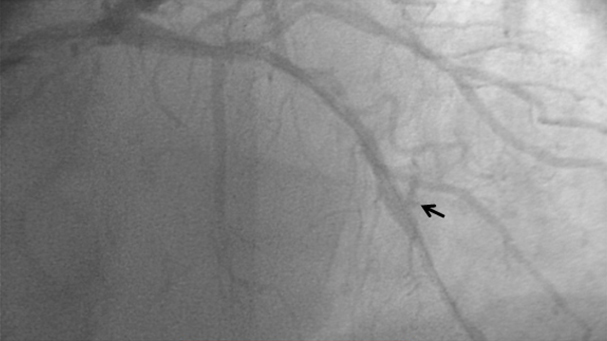
Figure 2. Image showing contrast extravasation to the pericardium (arrow)
For the perforation management, a balloon was dilated at 6 atm for 10 minutes on two occasions with an interval of 5 minutes between insufflations, after that, a decrease in contrast output was noted and immediately a second medicated stent with Biolimus 3.0 x 28mm at 10 atm was placed in proximal/middle third with complete resolution, maintaining a TIMI III coronary flow (Figure 3). During the procedure no hemodynamic changes were observed and post-procedure echocardiogram did not show pericardial effusion or abnormal motility. The patient was managed in the intensive care unit and was discharged after 5 days uneventful. Three months later, the patient remains stable and with an improved ejection fraction at rest and post effort.
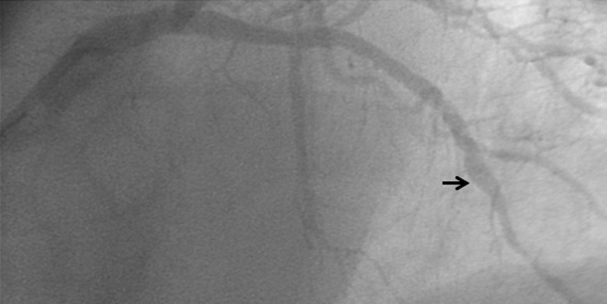
Figure 3. Resolution of contrast extravasation after balloon inflation (arrow)
Discussion
Coronary perforation is a rare, life-threatening complication in patients undergoing percutaneous coronary intervention. To date, possible causes of coronary perforation have been identified: slippage or leakage of the guidewire or intracoronary stent, overinflated or rupture of the balloon, passing the balloon or stent through dissected vessel, perforation with catheter intravascular ultrasound (IVUS), etcetera [3],[7],[9],[10].
It has been found that coronary perforation post percutaneous coronary intervention is mainly caused by over dilation or implanting an improperly sized stent; in the presented case two dilatations of balloon at 14 and 10 atm, respectively, were performed at the obstructions mentioned [9]. Later, medicated stent was placed at 12 atm probably resulting in the grade III coronary perforation. It is thought that this complication may have been caused by the presence of diffuse calcifications in the left anterior descending artery, this was not demonstrated due to lack of IVUS in the center.
On the other hand, there are several risk factors for coronary perforation linked to the patients as: advanced age, female gender, renal failure, arterial hypertension, peripheral artery disease and myocardial infarction [2],[3],[6],[9]. The patient of the case presentation was over 80 years old and suffered high blood pressure, increasing the risk for this complication. Also, angiographic risk factors have been reported in this complication such as: total chronic occlusion, coronary artery calcification, tortuous vessels, lesions in the circumflex and right coronary arteries and long lesions (> 10 mm) [11],[12]. In this case long injury, calcification and tortuosity of the coronary anatomy were present.
There is no consensus about treatment for the coronary perforation, in fact there are several therapeutic options such as placing a coated stent, embolization, observation, pericardiocentesis and emergency coronary artery bypass graft [13],[14],[15],[16],[17],[18],[19]. However, prolonged balloon inflation proximal or at the level of perforation plus the reversal of anticoagulation and, if indicated, platelet transfusions are most commonly used [20],[21],[22]. In this case, the balloon inflation was performed in two times every 10 minutes at 6 atm as suggested for stopping bleeding [12]. Even though, no reversal of anticoagulation was used, successful angiographic and ultrasounds results were obtained, despite some authors mention this has less chance of success [23]. Also, it has been reported that type III coronary perforation need an average of 48 minutes of balloon inflation, which is more than twice the time that was required (20 minutes) [8]. This could be explained by the rapid implementation of balloon inflation during the procedure, as well as the correct placement of it. In addition, the reduced time of balloon inflation allowed a reduction in chances of producing myocardial ischemia.
Coronary perforation can cause cardiac tamponade, arrhythmias, myocardial infarction and death [2],[3]. The most important are acute myocardial infarction and cardiac tamponade, these occur in 40% of type III coronary perforation and in patients with complex coronary anatomy [11],[24],[1]. As occurs in this case, perforation was type III and the patient had coronary anatomy complex (long lesion, tortuosity and calcification); however, no cardiac tamponed occurred probably because of rapid recognition and management or reduced width of perforation.
Conclusion
In conclusion, coronary perforation is a rare complication of percutaneous coronary intervention but leads to considerable mortality. The management of this complication does not have consensus, but primarily consists of balloon inflation and reversal of anticoagulation. In this case, successful resolution of a Type III coronary perforation was evidenced by balloon dilation for only 20 minutes. We have carried out the first report of a coronary perforation successfully managed in Peru.
Notes
From the editor
This article was originally submitted in Spanish and was translated into English by the authors. The Journal has not copyedited this version.
Conflicts of interests
The authors completed the ICMJE conflict of interest declaration form. They declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Funding
The authors declare that no external funding sources.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

La perforación coronaria es una complicación rara en los pacientes sometidos a angioplastias percutáneas coronarias. La mortalidad de esta complicación es variable, dependiendo de factores relacionados al paciente y al procedimiento realizado. Alcanza el 44% en pacientes con perforación tipo III, según la escala de Ellis. Presentamos el caso de un varón de 81 años con múltiples factores de riesgo cardiovascular, a quien se le realizó una angioplastia percutánea para manejo de un síndrome coronario agudo tipo angina inestable. El procedimiento se complicó con una perforación coronaria grado III en la arteria descendente anterior, la cual fue manejada exitosamente con dilatación de balón a 6 atmósferas por 10 minutos en dos oportunidades en la zona afectada, con intervalo de 5 minutos entre insuflaciones. El paciente evolucionó favorablemente y fue dado de alta.
 Authors:
Ricardo Coloma Araniya[1], Renato Beas[2], Jesús Maticorena-Quevedo[2], Alexander Anduaga-Beramendi[2], Marco Antonio Pastrana Castillo[1]
Authors:
Ricardo Coloma Araniya[1], Renato Beas[2], Jesús Maticorena-Quevedo[2], Alexander Anduaga-Beramendi[2], Marco Antonio Pastrana Castillo[1]
Affiliation:
[1] Clínica San Borja, Lima, Perú
[2] Escuela de medicina, Universidad Peruana de Ciencias Aplicadas, Lima, Perú
E-mail: renatobeas@gmail.com
Author address:
[1] Las Vascongadas
Manzana H
Lote 14
Los Girasoles de la Molina
Lima
Perú

Citation: Coloma Araniya R, Beas R, Maticorena-Quevedo J, Anduaga-Beramendi A, Pastrana Castillo MA. Successful management of grade III coronary perforation after percutaneous angioplasty in a high-risk patient: a case report. Medwave 2016 Mar;16(2):e6395 doi: 10.5867/medwave.2016.02.6395
Submission date: 18/11/2015
Acceptance date: 10/2/2016
Publication date: 3/3/2016
Origin: not requested
Type of review: reviewed by one external peer reviewer, with one double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Javaid A, Buch AN, Satler LF, Kent KM, Suddath WO, Lindsay J Jr, et al. Management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2006 Oct 1;98(7):911-4. | PubMed |
- Bauer T, Boeder N, Nef HM, Möllmann H, Hochadel M, Marco J, et al. Fate of Patients With Coronary Perforation Complicating Percutaneous Coronary Intervention (from the Euro Heart Survey Percutaneous Coronary Intervention Registry). Am J Cardiol. 2015 Nov 1;116(9):1363-7. | CrossRef | PubMed |
- Hendry C, Fraser D, Eichhofer J, Mamas MA, Fath-Ordoubadi F, El-Omar M, et al. Coronary perforation in the drug-eluting stent era: incidence, risk factors, management and outcome: the UK experience. EuroIntervention. 2012 May 15;8(1):79-86. | CrossRef | PubMed |
- Ellis SG, Ajluni S, Arnold AZ, Popma JJ, Bittl JA, Eigler NLet al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation. 1994 Dec;90(6):2725-30. | PubMed |
- Ben-Gal Y, Weisz G, Collins MB, Genereux P, Dangas GD, Teirstein PS, et al. Dual catheter technique for the treatment of severe coronary artery perforations. Catheter Cardiovasc Interv. 2010 Apr 1;75(5):708-12. | CrossRef | PubMed |
- Shimony A, Zahger D, Van Straten M, Shalev A, Gilutz H, Ilia R, et al. Incidence, risk factors, management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2009 Dec 15;104(12):1674-7. | CrossRef | PubMed |
- Al-Lamee R, Ielasi A, Latib A, Godino C, Ferraro M, Mussardo M, et al. Incidence, predictors, management, immediate and long-term outcomes following grade III coronary perforation. JACC Cardiovasc Interv. 2011 Jan;4(1):87-95. | CrossRef | PubMed |
- Meguro K, Ohira H, Nishikido T, Fujita M, Chinen T, Kikuchi T, et al. Outcome of prolonged balloon inflation for the management of coronary perforation. J Cardiol. 2013 Mar;61(3):206-9. | CrossRef | PubMed |
- Al-Mukhaini M, Panduranga P, Sulaiman K, Riyami AA, Deeb M, Riyami MB. Coronary perforation and covered stents: an update and review. Heart Views. 2011 Apr;12(2):63-70. | CrossRef | PubMed |
- Kilic ID, Alihanoglu YI, Yildiz SB, Taskoylu O, Zungur M, Uyar IS, et al. Coronary artery perforations: four different cases and a review. Rev Port Cardiol. 2013 Oct;32(10):811-5. | CrossRef | PubMed |
- Ramana RK, Arab D, Joyal D, Steen L, Cho L, Lewis Bet al. Coronary artery perforation during percutaneous coronary intervention: incidence and outcomes in the new interventional era. J Invasive Cardiol. 2005 Nov;17(11):603-5. | PubMed |
- Witzke CF, Martin-Herrero F, Clarke SC, Pomerantzev E, Palacios IF. The changing pattern of coronary perforation during percutaneous coronary intervention in the new device era. J Invasive Cardiol. 2004 Jun;16(6):257-301. | PubMed |
- Shirakabe A, Takano H, Nakamura S, Kikuchi A, Sasaki A, Yamamoto E, et al. Coronary perforation during percutaneous coronary intervention. Int Heart J. 2007 Jan;48(1):1-9. | PubMed |
- Rogers JH, Lasala JM. Coronary artery dissection and perforation complicating percutaneous coronary intervention. J Invasive Cardiol. 2004 Sep;16(9):493-9. | PubMed |
- Martí V, Castaño C, Guiteras P, Vallés E, Domínguez de Rozas J, Augé J. Perforación coronaria complicada con taponamiento cardíaco sellada mediante coils metálicos. Rev Esp Cardiol. 2004;57:990-2. | CrossRef |
- Inoue Y, Ueda T, Taguchi S, Kashima I, Koizumi K, Noma S. Teflon felt wrapping repair for coronary perforation after failed angioplasty. Ann Thorac Surg. 2006 Dec;82(6):2312-4. | PubMed |
- Totsugawa T, Kuinose M, Yoshitaka H, Katayama K, Tsushima Y, Ishida A, et al. Surgical treatment for Ellis type 3 coronary perforation during percutaneous catheter intervention. Circ J. 2012;76(2):377-81. | PubMed |
- Von Sohsten R, Kopistansky C, Cohen M, Kussmaul WG 3rd. Cardiac tamponade in the "new device" era: evaluation of 6999 consecutive percutaneous coronary interventions. Am Heart J. 2000 Aug;140(2):279-83. | PubMed |
- Krabatsch T, Becher D, Schweiger M, Hetzer R. Severe left atrium compression after percutaneous coronary intervention with perforation of a circumflex branch of the left coronary artery. Interact Cardiovasc Thorac Surg. 2010 Dec;11(6):811-3. | CrossRef | PubMed |
- Wang X, Ge J. Balloon Occlusion Types in the Treatment of Coronary Perforation during Percutaneous Coronary Intervention. Cardiol Res Pract. 2014;2014:784018. | CrossRef | PubMed |
- Briguori C, Di Mario C, De Gregorio J, Sheiban I, Vaghetti M, Colombo A. Administration of protamine after coronary stent deployment. Am Heart J. 1999 Jul;138(1 Pt 1):64-8. | PubMed |
- Gruberg L, Pinnow E, Flood R, Bonnet Y, Tebeica M, Waksman R, et al. Incidence, management, and outcome of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2000 Sep 15;86(6):680-2, A8. | PubMed |
- Meguro K, Ohira H, Nishikido T, Fujita M, Chinen T, Kikuchi T, et al. Outcome of prolonged balloon inflation for the management of coronary perforation. J Cardiol. 2013 Mar;61(3):206-9. | CrossRef | PubMed |
- Stathopoulos I, Kossidas K, Panagopoulos G, Garratt K. Cardiac tamponade complicating coronary perforation during angioplasty: short-term outcomes and long-term survival. J Invasive Cardiol. 2013 Oct;25(10):486-91. | PubMed |
 Javaid A, Buch AN, Satler LF, Kent KM, Suddath WO, Lindsay J Jr, et al. Management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2006 Oct 1;98(7):911-4. | PubMed |
Javaid A, Buch AN, Satler LF, Kent KM, Suddath WO, Lindsay J Jr, et al. Management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2006 Oct 1;98(7):911-4. | PubMed | Bauer T, Boeder N, Nef HM, Möllmann H, Hochadel M, Marco J, et al. Fate of Patients With Coronary Perforation Complicating Percutaneous Coronary Intervention (from the Euro Heart Survey Percutaneous Coronary Intervention Registry). Am J Cardiol. 2015 Nov 1;116(9):1363-7. | CrossRef | PubMed |
Bauer T, Boeder N, Nef HM, Möllmann H, Hochadel M, Marco J, et al. Fate of Patients With Coronary Perforation Complicating Percutaneous Coronary Intervention (from the Euro Heart Survey Percutaneous Coronary Intervention Registry). Am J Cardiol. 2015 Nov 1;116(9):1363-7. | CrossRef | PubMed | Hendry C, Fraser D, Eichhofer J, Mamas MA, Fath-Ordoubadi F, El-Omar M, et al. Coronary perforation in the drug-eluting stent era: incidence, risk factors, management and outcome: the UK experience. EuroIntervention. 2012 May 15;8(1):79-86.
| CrossRef | PubMed |
Hendry C, Fraser D, Eichhofer J, Mamas MA, Fath-Ordoubadi F, El-Omar M, et al. Coronary perforation in the drug-eluting stent era: incidence, risk factors, management and outcome: the UK experience. EuroIntervention. 2012 May 15;8(1):79-86.
| CrossRef | PubMed | Ellis SG, Ajluni S, Arnold AZ, Popma JJ, Bittl JA, Eigler NLet al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation. 1994 Dec;90(6):2725-30. | PubMed |
Ellis SG, Ajluni S, Arnold AZ, Popma JJ, Bittl JA, Eigler NLet al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation. 1994 Dec;90(6):2725-30. | PubMed | Ben-Gal Y, Weisz G, Collins MB, Genereux P, Dangas GD, Teirstein PS, et al. Dual catheter technique for the treatment of severe coronary artery perforations. Catheter Cardiovasc Interv. 2010 Apr 1;75(5):708-12. | CrossRef | PubMed |
Ben-Gal Y, Weisz G, Collins MB, Genereux P, Dangas GD, Teirstein PS, et al. Dual catheter technique for the treatment of severe coronary artery perforations. Catheter Cardiovasc Interv. 2010 Apr 1;75(5):708-12. | CrossRef | PubMed | Shimony A, Zahger D, Van Straten M, Shalev A, Gilutz H, Ilia R, et al. Incidence, risk factors, management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2009 Dec 15;104(12):1674-7. | CrossRef | PubMed |
Shimony A, Zahger D, Van Straten M, Shalev A, Gilutz H, Ilia R, et al. Incidence, risk factors, management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2009 Dec 15;104(12):1674-7. | CrossRef | PubMed | Al-Lamee R, Ielasi A, Latib A, Godino C, Ferraro M, Mussardo M, et al. Incidence, predictors, management, immediate and long-term outcomes following grade III coronary perforation. JACC Cardiovasc Interv. 2011 Jan;4(1):87-95. | CrossRef | PubMed |
Al-Lamee R, Ielasi A, Latib A, Godino C, Ferraro M, Mussardo M, et al. Incidence, predictors, management, immediate and long-term outcomes following grade III coronary perforation. JACC Cardiovasc Interv. 2011 Jan;4(1):87-95. | CrossRef | PubMed | Meguro K, Ohira H, Nishikido T, Fujita M, Chinen T, Kikuchi T, et al. Outcome of prolonged balloon inflation for the management of coronary perforation. J Cardiol. 2013 Mar;61(3):206-9. | CrossRef | PubMed |
Meguro K, Ohira H, Nishikido T, Fujita M, Chinen T, Kikuchi T, et al. Outcome of prolonged balloon inflation for the management of coronary perforation. J Cardiol. 2013 Mar;61(3):206-9. | CrossRef | PubMed | Al-Mukhaini M, Panduranga P, Sulaiman K, Riyami AA, Deeb M, Riyami MB. Coronary perforation and covered stents: an update and review. Heart Views. 2011 Apr;12(2):63-70. | CrossRef | PubMed |
Al-Mukhaini M, Panduranga P, Sulaiman K, Riyami AA, Deeb M, Riyami MB. Coronary perforation and covered stents: an update and review. Heart Views. 2011 Apr;12(2):63-70. | CrossRef | PubMed | Kilic ID, Alihanoglu YI, Yildiz SB, Taskoylu O, Zungur M, Uyar IS, et al. Coronary artery perforations: four different cases and a review. Rev Port Cardiol. 2013 Oct;32(10):811-5. | CrossRef | PubMed |
Kilic ID, Alihanoglu YI, Yildiz SB, Taskoylu O, Zungur M, Uyar IS, et al. Coronary artery perforations: four different cases and a review. Rev Port Cardiol. 2013 Oct;32(10):811-5. | CrossRef | PubMed | Ramana RK, Arab D, Joyal D, Steen L, Cho L, Lewis Bet al. Coronary artery perforation during percutaneous coronary intervention: incidence and outcomes in the new interventional era. J Invasive Cardiol. 2005 Nov;17(11):603-5. | PubMed |
Ramana RK, Arab D, Joyal D, Steen L, Cho L, Lewis Bet al. Coronary artery perforation during percutaneous coronary intervention: incidence and outcomes in the new interventional era. J Invasive Cardiol. 2005 Nov;17(11):603-5. | PubMed | Witzke CF, Martin-Herrero F, Clarke SC, Pomerantzev E, Palacios IF. The changing pattern of coronary perforation during percutaneous coronary intervention in the new device era. J Invasive Cardiol. 2004 Jun;16(6):257-301. | PubMed |
Witzke CF, Martin-Herrero F, Clarke SC, Pomerantzev E, Palacios IF. The changing pattern of coronary perforation during percutaneous coronary intervention in the new device era. J Invasive Cardiol. 2004 Jun;16(6):257-301. | PubMed | Shirakabe A, Takano H, Nakamura S, Kikuchi A, Sasaki A, Yamamoto E, et al. Coronary perforation during percutaneous coronary intervention. Int Heart J. 2007 Jan;48(1):1-9. | PubMed |
Shirakabe A, Takano H, Nakamura S, Kikuchi A, Sasaki A, Yamamoto E, et al. Coronary perforation during percutaneous coronary intervention. Int Heart J. 2007 Jan;48(1):1-9. | PubMed | Rogers JH, Lasala JM. Coronary artery dissection and perforation complicating percutaneous coronary intervention. J Invasive Cardiol. 2004 Sep;16(9):493-9. | PubMed |
Rogers JH, Lasala JM. Coronary artery dissection and perforation complicating percutaneous coronary intervention. J Invasive Cardiol. 2004 Sep;16(9):493-9. | PubMed | Martí V, Castaño C, Guiteras P, Vallés E, Domínguez de Rozas J, Augé J. Perforación coronaria complicada con taponamiento cardíaco sellada mediante coils metálicos. Rev Esp Cardiol. 2004;57:990-2. | CrossRef |
Martí V, Castaño C, Guiteras P, Vallés E, Domínguez de Rozas J, Augé J. Perforación coronaria complicada con taponamiento cardíaco sellada mediante coils metálicos. Rev Esp Cardiol. 2004;57:990-2. | CrossRef | Inoue Y, Ueda T, Taguchi S, Kashima I, Koizumi K, Noma S. Teflon felt wrapping repair for coronary perforation after failed angioplasty. Ann Thorac Surg. 2006 Dec;82(6):2312-4. | PubMed |
Inoue Y, Ueda T, Taguchi S, Kashima I, Koizumi K, Noma S. Teflon felt wrapping repair for coronary perforation after failed angioplasty. Ann Thorac Surg. 2006 Dec;82(6):2312-4. | PubMed | Totsugawa T, Kuinose M, Yoshitaka H, Katayama K, Tsushima Y, Ishida A, et al. Surgical treatment for Ellis type 3 coronary perforation during percutaneous catheter intervention. Circ J. 2012;76(2):377-81. | PubMed |
Totsugawa T, Kuinose M, Yoshitaka H, Katayama K, Tsushima Y, Ishida A, et al. Surgical treatment for Ellis type 3 coronary perforation during percutaneous catheter intervention. Circ J. 2012;76(2):377-81. | PubMed | Von Sohsten R, Kopistansky C, Cohen M, Kussmaul WG 3rd. Cardiac tamponade in the "new device" era: evaluation of 6999 consecutive percutaneous coronary interventions. Am Heart J. 2000 Aug;140(2):279-83. | PubMed |
Von Sohsten R, Kopistansky C, Cohen M, Kussmaul WG 3rd. Cardiac tamponade in the "new device" era: evaluation of 6999 consecutive percutaneous coronary interventions. Am Heart J. 2000 Aug;140(2):279-83. | PubMed | Krabatsch T, Becher D, Schweiger M, Hetzer R. Severe left atrium compression after percutaneous coronary intervention with perforation of a circumflex branch of the left coronary artery. Interact Cardiovasc Thorac Surg. 2010 Dec;11(6):811-3. | CrossRef | PubMed |
Krabatsch T, Becher D, Schweiger M, Hetzer R. Severe left atrium compression after percutaneous coronary intervention with perforation of a circumflex branch of the left coronary artery. Interact Cardiovasc Thorac Surg. 2010 Dec;11(6):811-3. | CrossRef | PubMed | Wang X, Ge J. Balloon Occlusion Types in the Treatment of Coronary Perforation during Percutaneous Coronary Intervention. Cardiol Res Pract. 2014;2014:784018. | CrossRef | PubMed |
Wang X, Ge J. Balloon Occlusion Types in the Treatment of Coronary Perforation during Percutaneous Coronary Intervention. Cardiol Res Pract. 2014;2014:784018. | CrossRef | PubMed | Briguori C, Di Mario C, De Gregorio J, Sheiban I, Vaghetti M, Colombo A. Administration of protamine after coronary stent deployment. Am Heart J. 1999 Jul;138(1 Pt 1):64-8. | PubMed |
Briguori C, Di Mario C, De Gregorio J, Sheiban I, Vaghetti M, Colombo A. Administration of protamine after coronary stent deployment. Am Heart J. 1999 Jul;138(1 Pt 1):64-8. | PubMed | Gruberg L, Pinnow E, Flood R, Bonnet Y, Tebeica M, Waksman R, et al. Incidence, management, and outcome of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2000 Sep 15;86(6):680-2, A8. | PubMed |
Gruberg L, Pinnow E, Flood R, Bonnet Y, Tebeica M, Waksman R, et al. Incidence, management, and outcome of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2000 Sep 15;86(6):680-2, A8. | PubMed | Meguro K, Ohira H, Nishikido T, Fujita M, Chinen T, Kikuchi T, et al. Outcome of prolonged balloon inflation for the management of coronary perforation. J Cardiol. 2013 Mar;61(3):206-9. | CrossRef | PubMed |
Meguro K, Ohira H, Nishikido T, Fujita M, Chinen T, Kikuchi T, et al. Outcome of prolonged balloon inflation for the management of coronary perforation. J Cardiol. 2013 Mar;61(3):206-9. | CrossRef | PubMed | Stathopoulos I, Kossidas K, Panagopoulos G, Garratt K. Cardiac tamponade complicating coronary perforation during angioplasty: short-term outcomes and long-term survival. J Invasive Cardiol. 2013 Oct;25(10):486-91. | PubMed |
Stathopoulos I, Kossidas K, Panagopoulos G, Garratt K. Cardiac tamponade complicating coronary perforation during angioplasty: short-term outcomes and long-term survival. J Invasive Cardiol. 2013 Oct;25(10):486-91. | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








