Key Words: Schonlein-Henoch purpura, bees, vasculitis, leukocytoclastic, cutaneous
Abstract
Henoch Schonlein purpura (HSP) is a common childhood vasculitis, characterized by a non-thrombocytopenic palpable purpura and systemic features. It can be triggered by conditions like infections and insect bites. We present the case of a six-year-old girl with palpable maculopapular lesions on the lower limbs, itching, mild pain, swelling of feet, limitation of limb mobility, and a history of bee sting. Thigh skin biopsy was performed, with a report of leucocytoclastic vasculitis, and was diagnosed as HSP. She was prescribed bed rest, and was given oral hydration. The patient outcome was favorable and was discharged after five days. This is the fifth report of a HSP case associated with a bee sting with an uncomplicated course, which is in contrast to previous case reports.
Introduction
Henoch Schonlein purpura is one the most common vasculitis in childhood. It is characterized as a palpable not thrombocytopenic purpura and shows gastrointestinal bleeding, abdominal distress, glomerulonephritis, arthritis and arthralgia. It also presents with leukocytoclastic vasculitis with immunoglobulin A at histopathological levels [1]. Heberden published the first description of Henoch Schonlein purpura in 1801, in two five-year-old boys. They had abdominal vomiting, melena, arthralgia, purpuric erythema and hematuria [2]. Johann Schonlein who recognized the association between purple and arthralgia, calling it “rheumatic peliosis”, characterized Henoch Schonlein purpura. His student, the pediatrician Eduard Henoch, who described the abdominal and renal compromise in four children [3],[4], extended this description. Afterwards, Gairdner used the term anaphylactoid purpura [5],[6].
Henoch Schonlein purpura often occurs in childhood, is predominant in males and is related to various triggers. These include bacterial, fungal, protozoan infections and insect bites [7]. Worldwide, there have been only four case reports associated with bee sting. We show here the case of a six-year-old student with Henoch Schonlein purpura with antecedent of a bee sting.
Case presentation
We received a six year and nine months old female student, from Trujillo (Peru), without comorbidities and up to date on vaccinations at the Hospital Regional Docente-Trujillo. Three weeks before her entry to the Hospital, she presented an upper respiratory tract infection. She was treated with mucolytic medication, amoxicillin and clavulanic acid. The respiratory infection subsided seven days later. Ten days before her entry to the hospital, she presented with nausea, headache, hiporexia, oral intolerance and vomiting. Six days before her entry to the hospital, she showed intermittent crampy abdominal pain for two days. Five days before her entry to the hospital, she sustained a bee sting on a foot with subsequent formation of painful inflammatory papule with puctiform injury.
Three days before her entry to the hospital, she presented with maculopapular palpable lesions in the lower limbs, which irradiated in a centripetal way to the anterior and posterior sides of the feet, legs and thighs. In addition, she developed itching, edema of the feet and limitation of movement. She went to the emergency department, where the diagnosis was Henoch Schonlein purpura and as outpatient was prescribed oral chlorpheniramine 7.5 ml every eight hours. There she denied abdominal pain. On the day of admission to the hospital, the lesions progressed to both buttocks. The Pediatricians hospitalized her with Henoch Schonlein purpura diagnosis.
Her measurements included weight of 25.5 kg, height 117.5 cm, and head circumference 49.5 cm. Vital signs: Blood pressure (BP) 90/60 mmHg (P95: 116/77), heart rate (HR) 100, respiratory rate (RR) 22. The patient was admitted in a generally good state, spontaneous ventilation, with reddish maculopapular lesions in upper and lower limbs and buttocks, but none in the inguinal region (Figures 1 and 2). Blood count, hematocrit, platelet count, peripheral blood profile, creatinina and urine test all were normal. Total abdominal ultrasound reported no abnormal findings.

Figure 1. Maculopapular lesions in both lower limbs.

Figure 2. Edema in the back of hand.
A skin biopsy (3 mm) was obtained from the thigh and stained with hematoxylin-eosin. Leukocytoclastic vasculitis was reported in small vessels at the reticular superficial dermis level, with superficial vascular plexus commitment (Figure 3). In addition, neutrophils invading and destroying the vessel wall were observed (Figure 4). Final pathological diagnosis included leukocytoclastic vasculitis.
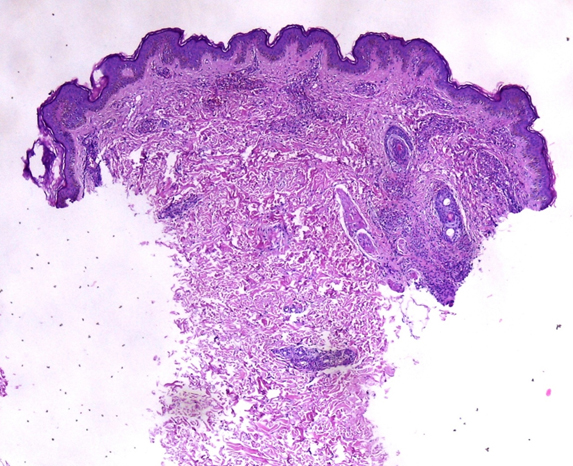
Figure 3. Skin biopsy, with hematoxylin-eosin staining.
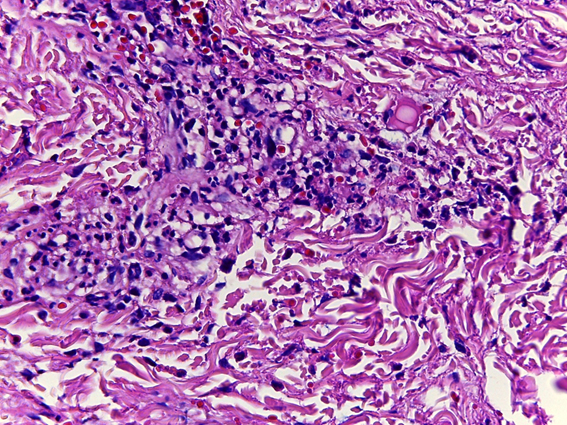
Figure 4. Skin biopsy, with hematoxylin-eosin staining.
During hospitalization the patient was afebrile. The edema was resolved five days after admission to the hospital and her evolution was favorable. The patient was resting, receiving orally hydration and paracetamol/acetaminophen conditional to fever during her hospitalization. She was discharged ten days after her admission to the hospital, with purpuric lesions in remission. The diagnosis upon discharge was Henoch Schonlein purpura.
Discussion
Henoch Schonlein purpura is a systemic vasculitis of small vessels, mediated by immunoglobulin A, also called leukocytoclastic vasculitis. This disease occurs frequently in childhood, usually between ages 3 and 15; it is infrequent in children under 2 years and adults [8],[9],[10],[11]. The most frequent age of presentation is between 6 and 7 years, with some seasonal variation, usually presenting in winter [12],[13]. In this case, the patient is six years nine months old.
Formerly known as anaphylactoid purpura, its name suggested an allergic process as the basis for its development. Currently and due to the presence of immunoglobulin A deposits, it is suggested as an immunologic origin, although there is a genetic component [1]. The etiology is unknown, but is often associated to infectious diseases, usually bacterial, as triggers [8],[12],[14],[15],[16],[17],[18],[19]. Others causes have been established; including viral infections, vaccination and even processes caused by insects [7].
At the histological level, it is characterized by leukocytoclastic vasculitis of small vessels with immunoglobulin A deposits [1]. Clinically, it presents as a palpable purpura associated with itching in areas dependent on pressure especially in the lower limbs and buttocks. Lesions can occur in different regions of the body [1],[20]. Skin lesions vary from small petechiae to large ecchymoses and hemorrhagic blisters. The color changes from erythematous to eritemato-violet and finally brown [1]. In very early stages of the disease, particularly in very young children, it can occur with subcutaneous edema in the back of the hands, feet, around the eyes, forehead, scalp and scrotum [1],[20]. Our patient showed reddish maculopapular manifestations, in different sizes, in upper and lower limbs and buttocks, but none in the inguinal region. In addition, she also had edema in the back of the hands.
Gastrointestinal manifestations are usually present in two thirds of the children [12],[21]; mostly within a week of the initial itching up to 30 days. In 14 to 36 % of the cases, abdominal pain precedes other manifestations [21],[22],[23]. Sub-mucosal edema and intramural hemorrhage resulting from vasculitis in the intestinal wall can lead to intussusception, gangrene and even perforation [1]. In many cases the abdominal pain can be intermittent, crampy [21] and located in the upper umbilical region [22],[24].
Renal compromise is present in a third of the children and of these, in less than 10 % becomes a complication that puts the patient’s life at risk. Arthralgias are present in various joints; although in children it mostly affects knees and ankles [8]. These are characterized by periarticular edema [12], stiffness, generally without erythema or drainage, but with considerable pain and limitation of movement. Our patient presented with abdominal pain and cramping three days before the presentation of maculopapular lesions, no renal compromise, but pain in the feet and with limitation of her movement.
Laboratory tests usually show no abnormalities, as evidenced in the case presented. Platelet count may be normal or high; this generates two types of Henoch Schonlein: with and without thrombocytopenia. Some children may have leukocytosis of up to 20,000 leukocytes with left deviation. Ultrasound can detect gastrointestinal abnormalities. In our case, all tests were normal. Treatment consists in support, hydration, nutrition, electrolytes balance and pain control with acetaminophen. Additionally, it is possible to use corticosteroids to reduce the articular compromise; however, there are no specific instructions on its use [1]. During hospitalization the patient rests, receiving hydration and paracetamol/acetaminophen conditional to fever.
There are few earlier reports related to bee stings [25],[26],[27],[28]. The first description in association with bee stings was made by Burke and Jellinek in a four-year-old girl with a sting, seven days prior the onset of symptoms. They reported a severe picture marked by joints swelling, watery diarrhea, hematuria, mane and shock, which resolved spontaneously [25]. Sharan et al. reported the second association with bee stings. They described a 10 year old patient with little skin symptomatology, abdominal pain, nausea and vomiting. These symptoms began one week after the bite and they hypothesized causation as a hypersensitive response to insect sting [26]. Quercia et al. were the third, which reported a twelve-year-old girl with a previous episode of Henoch Schonlein purpura associated with streptococcal sore throat. The patient was stung some days prior to the symptoms onset. She presented a moderate clinical picture and they performed an allergy test to hymenoptera which was positive [27]. Akgun et al. were the fourth to report a Henoch Schonlein purpura in a six-year-old boy. The boy presented diffuse abdominal severe pain and antecedent of bee sting ten days prior to the symptoms onset [28]. In our case the six years nine months old girl presented with purpuric manifestations, which began 48 hours after a bee sting. The evolution time is shorter in relation to previous reports. Clinical manifestations were mild. Nausea, vomiting and abdominal pain preceded sting.
Bee sting produces different clinical and physiopathological manifestations. Bee venom is composed mainly by mellitin. This protein hydrolyzes the cell membrane and modifies the cell permeability, causing the histamine and catecholamines release. Catecholamine generates intravascular hemolysis via phospholipase A2 [29],[30]. There have been reported hemorrhagic vasculitis [31], thrombocytopenic purpura [32],[33] and alterations at the abdominal and kidney level subsequent to bee stings [29],[30],[31],[34],[35]. Although some case studies have included the hymenoptera test [27], this was not performed because it was not available in our hospital.
Upper respiratory tract infection is the most frequent trigger of Henoch Schonlein purpura (between 42 and 65 %); however, this occurs, in the majority of cases, between seven to ten days before the symptoms onset [12],[13] . There is no differences in the clinical picture, age, sex, abdominal and articular manifestations in patients with and without previous respiratory infection. Patients with upper respiratory tract infection history present most frequently kidney complications [36]; this did not exist in our patient. The upper respiratory tract infection, in our patient, was treated with antibiotics; these could possibly trigger Henoch Schonlein purpura. However, no differences exist between patients who receive and patients who do not receive medication (including beta-lactams as amoxicillin) [36].
The patient showed crampy abdominal pain as an initial symptom; this symptom is infrequent as an initial symptom [37], but can indicate that Henoch Schonlein purpura has already begun. Approximately 25 % of the patients have abdominal pain, on average, five days before maculopapular lesions occurrence [21]. These details raise confusion in relation to the trigger and allow us to reconsider the role of bee stings as a trigger or an adjuvant in Henoch Schonlein purpura’s symptomatology. Case reports related to bee sting have been variable, both with and without complications. For this reason, we cannot say that the trigger has been either the respiratory infectious process or bee sting. However, we showed in our patient that both factors are related in the presentation and possible causation of Henoch Schonlein purpura.
Conclusion
Henoch Schonlein purpura presents various triggers, which can manifest either isolated or together, as in our case; i.e., characteristic clinical signs including palpable purpuric lesions occurring 48 hours after bee sting, skin and articular manifestations, no gastrointestinal or renal dysfunction at the time of her admission to the hospital.
Henoch Schonlein purpura is a vasculitis mediated by immunoglobulin A. At the histological level, it is characterized a small vessels leukocytoclastic vasculitis as is shown in this case.
It is important to conduct a good medical history in all patients in which Henoch Schonlein purpura is suspected, with information that includes, exposure to drugs, infectious diseases, and insect bites to decipher the potential trigger.
Henoch Schonlein purpura triggered by bee sting is a rare picture. In this case, it was documented in the patient medical history with potential associations for what might have been the trigger.
Notes
From the editor
This article was originally submitted in Spanish and was translated into English by the authors. The Journal has not copyedited this version.
Acknowledgements
The authors want to thank Dr. Alix Arce, pediatrician of Belen Hospital (Trujillo), for review and comments to this article; Dr. Diana Diaz, Dr. Julio Vicuña and Dr. Alan Diaz from the Pediatric service of the Hospital Regional Docente (Trujillo) for their support in the evaluation, diagnosis and management of the patient during hospitalization; and Dr. Erin Pias Hines for reviewing the English version.
Conflicts of interests
The authors completed the conflict of interests declaration form from the ICMJE, and declared not having any conflict of interests with the matter dealt herein. Forms can be requested to the responsible author or the editorial direction of the Journal.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

La púrpura de Henoch Schonlein es una vasculitis común en la infancia, caracterizada por una púrpura palpable no trombocitopénica y manifestaciones sistémicas. Está relacionada con patologías desencadenantes como las infecciones y las picaduras de insectos. Presentamos el caso de una escolar de 6 años, de sexo femenino, con lesiones maculopapulares palpables en miembros inferiores, prurito, dolor leve, edema de pies, limitación al movimiento y antecedente de picadura de abeja. Se realizó biopsia cutánea de muslo con reporte de vasculitis leucocitoclástica y se diagnosticó como púrpura de Henoch Schonlein. Se indicó reposo y se le administró hidratación oral. Evolucionó favorablemente y fue dada de alta a los cinco días. Este es el quinto caso de púrpura de Henoch Schonlein asociado a picadura de abeja, la que se presentó sin complicaciones a diferencia de los reportes de caso previos.
 Authors:
José Galvez-Olortegui[1,2], Mayita Álvarez-Vargas[1,2], Juan Durand-Vergara[3], Marisol Díaz-Lozano[2], Tomas Galvez-Olortegui[1,2,4], Indira Armas-Ramírez[1], Julio Hilario-Vargas[5]
Authors:
José Galvez-Olortegui[1,2], Mayita Álvarez-Vargas[1,2], Juan Durand-Vergara[3], Marisol Díaz-Lozano[2], Tomas Galvez-Olortegui[1,2,4], Indira Armas-Ramírez[1], Julio Hilario-Vargas[5]
Affiliation:
[1] Facultad de Medicina, Universidad Nacional de Trujillo, Trujillo, Perú
[2] Scientia Clinical and Epidemiological Research Institute, Trujillo, Perú
[3] Departamento de Pediatría, Hospital Regional Docente de Trujillo, Trujillo, Perú
[4] Instituto Regional de Oftalmología, Trujillo, Perú
[5] Departamento de Fisiología, Facultad de Medicina, Universidad Nacional de Trujillo, Trujillo, Perú
E-mail: jgalvezo@scientiaceri.com
Author address:
[1] Scientia Clinical and Epidemiological Research Institute
Mz. G Lt 22
Urb. Vista Hermosa
Trujillo
Perú

Citation: Galvez-Olortegui J, Álvarez-Vargas M, Durand-Vergara J, Díaz-Lozano M, Galvez-Olortegui T, Armas-Ramírez I, et al. Henoch Schonlein purpura associated with bee sting: case report. Medwave 2015 Oct;15(9):e6297 doi: 10.5867/medwave.2015.09.6297
Submission date: 21/8/2015
Acceptance date: 20/10/2015
Publication date: 30/10/2015
Origin: not requested
Type of review: reviewed by three external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Cassidy JT, Petty RE, Laxer RM, Lindsley CB. Textbook of Pediatric Rheumatology. 6 edition. Philadelphia: Saunders Elsevier; 2010.
- Rook A. William Heberden’s Cases of Anaphylactoid Purpura. Arch Dis Child. 1958 Jun 1;33(169):271–271. | CrossRef |
- Tarvin SE, Ballinger S. Henoch– Schoenlein purpura. Curr Paediatr. 2006 Aug;16(4):259–63. | CrossRef |
- Kamath N, Rao S. Henoch–Schonlein purpura: An update. Indian J Rheumatol [Internet]. Indian Rheumatology Association; 2012 May;7(1):92–8. | CrossRef |
- Gairdner D. The Schönlein-Henoch syndrome (anaphylactoid purpura). Q J Med. 1948 Apr;17(66):95-122. | PubMed |
- Meadow R. Schönlein-Henoch syndrome. Arch Dis Child. 1979 Nov;54(11):822-4. | PubMed |
- Rigante D, Castellazzi L, Bosco A, Esposito S. Is there a crossroad between infections, genetics, and Henoch-Schönlein purpura? Autoimmun Rev. 2013 Aug;12(10):1016-21. | CrossRef | PubMed |
- Saulsbury FT. Henoch-Schönlein purpura in children. Report of 100 patients and review of the literature. Medicine (Baltimore). 1999 Nov;78(6):395-409. | PubMed |
- Al-Sheyyab M, El-Shanti H, Ajlouni S, Sawalha D, Daoud A. The clinical spectrum of Henoch-Schönlein purpura in infants and young children. Eur J Pediatr. 1995 Dec;154(12):969-72. | PubMed |
- Lu S, Liu D, Xiao J, Yuan W, Wang X, Zhang X, Zhang J, Liu Z, Zhao Z. Comparison between adults and children with Henoch-Schönlein purpura nephritis. Pediatr Nephrol. 2015 May;30(5):791-6. | CrossRef | PubMed |
- García-Porrúa C, Calviño MC, Llorca J, Couselo JM, González-Gay MA. Henoch-Schönlein purpura in children and adults: clinical differences in a defined population. Semin Arthritis Rheum. 2002 Dec;32(3):149-56. | PubMed |
- Martínez López MM, Rodríguez Arranz C, Peña Carrión A, Merino Muñoz R, García-Consuegra Molina J. [Henoch-Schönlein purpura. Study of factors associated with the development and course of the disease]. An Pediatr (Barc). 2007 May;66(5):453-8. | PubMed |
- Trapani S, Micheli A, Grisolia F, Resti M, Chiappini E, Falcini F, De Martino M. Henoch Schonlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005 Dec;35(3):143-53. | PubMed |
- Allen DM, Diamond LK, Howell DA. Anaphylactoid purpura in children (Schonlein-Henoch syndrome): review with a follow-up of the renal complications. AMA J Dis Child. 1960 Jun;99:833-54. | PubMed |
- al-Sheyyab M, Batieha A, el-Shanti H, Daoud A. Henoch-Schonlein purpura and streptococcal infection: a prospective case-control study. Ann Trop Paediatr. 1999 Sep;19(3):253-5. | PubMed |
- Masuda M, Nakanishi K, Yoshizawa N, Iijima K, Yoshikawa N. Group A streptococcal antigen in the glomeruli of children with Henoch-chönlein nephritis. Am J Kidney Dis. 2003 Feb;41(2):366-70. | PubMed |
- al-Sheyyab M, el-Shanti H, Ajlouni S, Batieha A, Daoud AS. Henoch-Schonlein purpura: clinical experience and contemplations on a streptococcal association. J Trop Pediatr. 1996 Aug;42(4):200-3. | PubMed |
- Mandai S, Aoyagi M, Nagahama K, Arai Y, Hirasawa S, Aki S, et al. Post-staphylococcal infection Henoch-Schönlein purpura nephritis: a case report and review of the literature. Ren Fail. 2013 Jul;35(6):869-74. | CrossRef | PubMed |
- Parekh N, Patel P, Sirsikar S. A Case of Cellulitis and Palpable Purpura. Infect Dis Clin Pract. 2009;17(5):328-30. | Link |
- Woo P, Laxer R, Sherry D. Pediatric Rheymatology in Clinical Practice. 1st ed. Springer-Verlag London; 2007.
- Chen SY, Kong MS. Gastrointestinal manifestations and complications of Henoch-Schönlein purpura. Chang Gung Med J. 2004 Mar;27(3):175-81. | PubMed |
- Rosenblum ND, Winter HS. Steroid effects on the course of abdominal pain in children with Henoch-Schonlein purpura. Pediatrics. 1987 Jun;79(6):1018-21. | PubMed |
- Choong CK, Beasley SW. Intra-abdominal manifestations of Henoch-Schönlein purpura. J Paediatr Child Health. 1998 Oct;34(5):405-9. | PubMed |
- Ebert EC. Gastrointestinal manifestations of Henoch-Schonlein Purpura. Dig Dis Sci. 2008 Aug;53(8):2011-9. | CrossRef | PubMed |
- Sharan G, Anand RK, Sinha KP. Schönlein-Henoch syndrome after insect bite. Br Med J. 1966 Mar 12;1(5488):656. | PubMed |
- Burke D, Jellinek H. Nearly fatal case of Schoenlein-Henoch syndrome following insect bite. AMA Am J Dis Child. 1954 Dec;88(6):772-4. | PubMed |
- Quercia O, Emiliani F, Foschi FG, Stefanini GF. Unusual reaction to hymenoptera sting: a case of Schönlein-Henoch purpura. Allergy. 2007 Mar;62(3):333-4. | PubMed |
- Akgün C, Demir N, Tuncer O, Üstyol L, Akbayram S. A case of Henoch-Schönlein purpura triggered by wild bee sting. Indian J Allergy, Asthma Immunol. 2013;27(1):55. | CrossRef |
- Fitzgerald KT, Flood AA. Hymenoptera stings. Clin Tech Small Anim Pract. 2006 Nov;21(4):194-204. | PubMed |
- Przybilla B, Ruëff F. Insect stings: clinical features and management. Dtsch Arztebl Int. 2012 Mar;109(13):238-48. | CrossRef | PubMed |
- Mingomataj EÇ, Bakiri AH, Ibranji A, Sturm GJ. Unusual reactions to hymenoptera stings: what should we keep in mind? Clin Rev Allergy Immunol. 2014 Aug;47(1):91-9. | CrossRef | PubMed |
- Namdev R, Dutta SR, Singh H. Acute immune thrombocytopenic purpura triggered by insect bite. J Indian Soc Pedod Prev Dent. 2009 Jan-Mar;27(1):58-61. | CrossRef | PubMed |
- Akbayram S, Akgun C, Dogan M, Caksen H, Oner AF. Acute ITP due to insect bite: report of 2 cases. Clin Appl Thromb Hemost. 2011 Aug;17(4):408-9. | CrossRef | PubMed |
- Reisman RE. Unusual reactions to insect stings. Curr Opin Allergy Clin Immunol. 2005 Aug;5(4):355-8. | PubMed |
- Ellis AK, Day JH. Clinical reactivity to insect stings. Curr Opin Allergy Clin Immunol. 2005 Aug;5(4):349-54. | PubMed |
- Gonzalez-Gay MA, Calviño MC, Vazquez-Lopez ME, Garcia-Porrua C, Fernandez-Iglesias JL, Dierssen T, et al. Implications of upper respiratory tract infections and drugs in the clinical spectrum of Henoch-Schönlein purpura in children. Clin Exp Rheumatol. 2004 Nov-Dec;22(6):781-4. | PubMed |
- Chen O, Zhu XB, Ren P, Wang YB, Sun RP, Wei DE. Henoch Schonlein Purpura in children: clinical analysis of 120 cases. Afr Health Sci. 2013 Mar;13(1):94-9. | CrossRef | PubMed |
 Cassidy JT, Petty RE, Laxer RM, Lindsley CB. Textbook of Pediatric Rheumatology. 6 edition. Philadelphia: Saunders Elsevier; 2010.
Cassidy JT, Petty RE, Laxer RM, Lindsley CB. Textbook of Pediatric Rheumatology. 6 edition. Philadelphia: Saunders Elsevier; 2010.  Rook A. William Heberden’s Cases of Anaphylactoid Purpura. Arch Dis Child. 1958 Jun 1;33(169):271–271. | CrossRef |
Rook A. William Heberden’s Cases of Anaphylactoid Purpura. Arch Dis Child. 1958 Jun 1;33(169):271–271. | CrossRef | Tarvin SE, Ballinger S. Henoch– Schoenlein purpura. Curr Paediatr. 2006 Aug;16(4):259–63. | CrossRef |
Tarvin SE, Ballinger S. Henoch– Schoenlein purpura. Curr Paediatr. 2006 Aug;16(4):259–63. | CrossRef | Kamath N, Rao S. Henoch–Schonlein purpura: An update. Indian J Rheumatol [Internet]. Indian Rheumatology Association; 2012 May;7(1):92–8. | CrossRef |
Kamath N, Rao S. Henoch–Schonlein purpura: An update. Indian J Rheumatol [Internet]. Indian Rheumatology Association; 2012 May;7(1):92–8. | CrossRef | Gairdner D. The Schönlein-Henoch syndrome (anaphylactoid purpura). Q J Med. 1948 Apr;17(66):95-122. | PubMed |
Gairdner D. The Schönlein-Henoch syndrome (anaphylactoid purpura). Q J Med. 1948 Apr;17(66):95-122. | PubMed | Rigante D, Castellazzi L, Bosco A, Esposito S. Is there a crossroad between infections, genetics, and Henoch-Schönlein purpura? Autoimmun Rev. 2013 Aug;12(10):1016-21. | CrossRef | PubMed |
Rigante D, Castellazzi L, Bosco A, Esposito S. Is there a crossroad between infections, genetics, and Henoch-Schönlein purpura? Autoimmun Rev. 2013 Aug;12(10):1016-21. | CrossRef | PubMed | Saulsbury FT. Henoch-Schönlein purpura in children. Report of 100 patients and review of the literature. Medicine (Baltimore). 1999 Nov;78(6):395-409. | PubMed |
Saulsbury FT. Henoch-Schönlein purpura in children. Report of 100 patients and review of the literature. Medicine (Baltimore). 1999 Nov;78(6):395-409. | PubMed | Al-Sheyyab M, El-Shanti H, Ajlouni S, Sawalha D, Daoud A. The clinical spectrum of Henoch-Schönlein purpura in infants and young children. Eur J Pediatr. 1995 Dec;154(12):969-72. | PubMed |
Al-Sheyyab M, El-Shanti H, Ajlouni S, Sawalha D, Daoud A. The clinical spectrum of Henoch-Schönlein purpura in infants and young children. Eur J Pediatr. 1995 Dec;154(12):969-72. | PubMed | Lu S, Liu D, Xiao J, Yuan W, Wang X, Zhang X, Zhang J, Liu Z, Zhao Z. Comparison between adults and children with Henoch-Schönlein purpura nephritis. Pediatr Nephrol. 2015 May;30(5):791-6. | CrossRef | PubMed |
Lu S, Liu D, Xiao J, Yuan W, Wang X, Zhang X, Zhang J, Liu Z, Zhao Z. Comparison between adults and children with Henoch-Schönlein purpura nephritis. Pediatr Nephrol. 2015 May;30(5):791-6. | CrossRef | PubMed | García-Porrúa C, Calviño MC, Llorca J, Couselo JM, González-Gay MA. Henoch-Schönlein purpura in children and adults: clinical differences in a defined population. Semin Arthritis Rheum. 2002 Dec;32(3):149-56. | PubMed |
García-Porrúa C, Calviño MC, Llorca J, Couselo JM, González-Gay MA. Henoch-Schönlein purpura in children and adults: clinical differences in a defined population. Semin Arthritis Rheum. 2002 Dec;32(3):149-56. | PubMed | Martínez López MM, Rodríguez Arranz C, Peña Carrión A, Merino Muñoz R, García-Consuegra Molina J. [Henoch-Schönlein purpura. Study of factors associated with the development and course of the disease]. An Pediatr (Barc). 2007 May;66(5):453-8. | PubMed |
Martínez López MM, Rodríguez Arranz C, Peña Carrión A, Merino Muñoz R, García-Consuegra Molina J. [Henoch-Schönlein purpura. Study of factors associated with the development and course of the disease]. An Pediatr (Barc). 2007 May;66(5):453-8. | PubMed | Trapani S, Micheli A, Grisolia F, Resti M, Chiappini E, Falcini F, De Martino M. Henoch Schonlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005 Dec;35(3):143-53. | PubMed |
Trapani S, Micheli A, Grisolia F, Resti M, Chiappini E, Falcini F, De Martino M. Henoch Schonlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005 Dec;35(3):143-53. | PubMed | Allen DM, Diamond LK, Howell DA. Anaphylactoid purpura in children (Schonlein-Henoch syndrome): review with a follow-up of the renal complications. AMA J Dis Child. 1960 Jun;99:833-54. | PubMed |
Allen DM, Diamond LK, Howell DA. Anaphylactoid purpura in children (Schonlein-Henoch syndrome): review with a follow-up of the renal complications. AMA J Dis Child. 1960 Jun;99:833-54. | PubMed | al-Sheyyab M, Batieha A, el-Shanti H, Daoud A. Henoch-Schonlein purpura and streptococcal infection: a prospective case-control study. Ann Trop Paediatr. 1999 Sep;19(3):253-5. | PubMed |
al-Sheyyab M, Batieha A, el-Shanti H, Daoud A. Henoch-Schonlein purpura and streptococcal infection: a prospective case-control study. Ann Trop Paediatr. 1999 Sep;19(3):253-5. | PubMed | Masuda M, Nakanishi K, Yoshizawa N, Iijima K, Yoshikawa N. Group A streptococcal antigen in the glomeruli of children with Henoch-chönlein nephritis. Am J Kidney Dis. 2003 Feb;41(2):366-70. | PubMed |
Masuda M, Nakanishi K, Yoshizawa N, Iijima K, Yoshikawa N. Group A streptococcal antigen in the glomeruli of children with Henoch-chönlein nephritis. Am J Kidney Dis. 2003 Feb;41(2):366-70. | PubMed | al-Sheyyab M, el-Shanti H, Ajlouni S, Batieha A, Daoud AS. Henoch-Schonlein purpura: clinical experience and contemplations on a streptococcal association. J Trop Pediatr. 1996 Aug;42(4):200-3. | PubMed |
al-Sheyyab M, el-Shanti H, Ajlouni S, Batieha A, Daoud AS. Henoch-Schonlein purpura: clinical experience and contemplations on a streptococcal association. J Trop Pediatr. 1996 Aug;42(4):200-3. | PubMed | Mandai S, Aoyagi M, Nagahama K, Arai Y, Hirasawa S, Aki S, et al. Post-staphylococcal infection Henoch-Schönlein purpura nephritis: a case report and review of the literature. Ren Fail. 2013 Jul;35(6):869-74.
| CrossRef | PubMed |
Mandai S, Aoyagi M, Nagahama K, Arai Y, Hirasawa S, Aki S, et al. Post-staphylococcal infection Henoch-Schönlein purpura nephritis: a case report and review of the literature. Ren Fail. 2013 Jul;35(6):869-74.
| CrossRef | PubMed | Parekh N, Patel P, Sirsikar S. A Case of Cellulitis and Palpable Purpura. Infect Dis Clin Pract. 2009;17(5):328-30. | Link |
Parekh N, Patel P, Sirsikar S. A Case of Cellulitis and Palpable Purpura. Infect Dis Clin Pract. 2009;17(5):328-30. | Link | Woo P, Laxer R, Sherry D. Pediatric Rheymatology in Clinical Practice. 1st ed. Springer-Verlag London; 2007.
Woo P, Laxer R, Sherry D. Pediatric Rheymatology in Clinical Practice. 1st ed. Springer-Verlag London; 2007.  Chen SY, Kong MS. Gastrointestinal manifestations and complications of Henoch-Schönlein purpura. Chang Gung Med J. 2004 Mar;27(3):175-81. | PubMed |
Chen SY, Kong MS. Gastrointestinal manifestations and complications of Henoch-Schönlein purpura. Chang Gung Med J. 2004 Mar;27(3):175-81. | PubMed | Rosenblum ND, Winter HS. Steroid effects on the course of abdominal pain in children with Henoch-Schonlein purpura. Pediatrics. 1987 Jun;79(6):1018-21.
| PubMed |
Rosenblum ND, Winter HS. Steroid effects on the course of abdominal pain in children with Henoch-Schonlein purpura. Pediatrics. 1987 Jun;79(6):1018-21.
| PubMed | Choong CK, Beasley SW. Intra-abdominal manifestations of Henoch-Schönlein purpura. J Paediatr Child Health. 1998 Oct;34(5):405-9.
| PubMed |
Choong CK, Beasley SW. Intra-abdominal manifestations of Henoch-Schönlein purpura. J Paediatr Child Health. 1998 Oct;34(5):405-9.
| PubMed | Ebert EC. Gastrointestinal manifestations of Henoch-Schonlein Purpura. Dig Dis Sci. 2008 Aug;53(8):2011-9. | CrossRef | PubMed |
Ebert EC. Gastrointestinal manifestations of Henoch-Schonlein Purpura. Dig Dis Sci. 2008 Aug;53(8):2011-9. | CrossRef | PubMed | Sharan G, Anand RK, Sinha KP. Schönlein-Henoch syndrome after insect bite. Br Med J. 1966 Mar 12;1(5488):656. | PubMed |
Sharan G, Anand RK, Sinha KP. Schönlein-Henoch syndrome after insect bite. Br Med J. 1966 Mar 12;1(5488):656. | PubMed | Burke D, Jellinek H. Nearly fatal case of Schoenlein-Henoch syndrome following insect bite. AMA Am J Dis Child. 1954 Dec;88(6):772-4. | PubMed |
Burke D, Jellinek H. Nearly fatal case of Schoenlein-Henoch syndrome following insect bite. AMA Am J Dis Child. 1954 Dec;88(6):772-4. | PubMed | Quercia O, Emiliani F, Foschi FG, Stefanini GF. Unusual reaction to hymenoptera sting: a case of Schönlein-Henoch purpura. Allergy. 2007 Mar;62(3):333-4. | PubMed |
Quercia O, Emiliani F, Foschi FG, Stefanini GF. Unusual reaction to hymenoptera sting: a case of Schönlein-Henoch purpura. Allergy. 2007 Mar;62(3):333-4. | PubMed | Akgün C, Demir N, Tuncer O, Üstyol L, Akbayram S. A case of Henoch-Schönlein purpura triggered by wild bee sting. Indian J Allergy, Asthma Immunol. 2013;27(1):55. | CrossRef |
Akgün C, Demir N, Tuncer O, Üstyol L, Akbayram S. A case of Henoch-Schönlein purpura triggered by wild bee sting. Indian J Allergy, Asthma Immunol. 2013;27(1):55. | CrossRef | Fitzgerald KT, Flood AA. Hymenoptera stings. Clin Tech Small Anim Pract. 2006 Nov;21(4):194-204. | PubMed |
Fitzgerald KT, Flood AA. Hymenoptera stings. Clin Tech Small Anim Pract. 2006 Nov;21(4):194-204. | PubMed | Przybilla B, Ruëff F. Insect stings: clinical features and management. Dtsch Arztebl Int. 2012 Mar;109(13):238-48. | CrossRef | PubMed |
Przybilla B, Ruëff F. Insect stings: clinical features and management. Dtsch Arztebl Int. 2012 Mar;109(13):238-48. | CrossRef | PubMed | Mingomataj EÇ, Bakiri AH, Ibranji A, Sturm GJ. Unusual reactions to hymenoptera stings: what should we keep in mind? Clin Rev Allergy Immunol. 2014 Aug;47(1):91-9. | CrossRef | PubMed |
Mingomataj EÇ, Bakiri AH, Ibranji A, Sturm GJ. Unusual reactions to hymenoptera stings: what should we keep in mind? Clin Rev Allergy Immunol. 2014 Aug;47(1):91-9. | CrossRef | PubMed | Namdev R, Dutta SR, Singh H. Acute immune thrombocytopenic purpura triggered by insect bite. J Indian Soc Pedod Prev Dent. 2009 Jan-Mar;27(1):58-61. | CrossRef | PubMed |
Namdev R, Dutta SR, Singh H. Acute immune thrombocytopenic purpura triggered by insect bite. J Indian Soc Pedod Prev Dent. 2009 Jan-Mar;27(1):58-61. | CrossRef | PubMed | Akbayram S, Akgun C, Dogan M, Caksen H, Oner AF. Acute ITP due to insect bite: report of 2 cases. Clin Appl Thromb Hemost. 2011 Aug;17(4):408-9.
| CrossRef | PubMed |
Akbayram S, Akgun C, Dogan M, Caksen H, Oner AF. Acute ITP due to insect bite: report of 2 cases. Clin Appl Thromb Hemost. 2011 Aug;17(4):408-9.
| CrossRef | PubMed | Reisman RE. Unusual reactions to insect stings. Curr Opin Allergy Clin Immunol. 2005 Aug;5(4):355-8.
| PubMed |
Reisman RE. Unusual reactions to insect stings. Curr Opin Allergy Clin Immunol. 2005 Aug;5(4):355-8.
| PubMed | Ellis AK, Day JH. Clinical reactivity to insect stings. Curr Opin Allergy Clin Immunol. 2005 Aug;5(4):349-54. | PubMed |
Ellis AK, Day JH. Clinical reactivity to insect stings. Curr Opin Allergy Clin Immunol. 2005 Aug;5(4):349-54. | PubMed | Gonzalez-Gay MA, Calviño MC, Vazquez-Lopez ME, Garcia-Porrua C, Fernandez-Iglesias JL, Dierssen T, et al. Implications of upper respiratory tract infections and drugs in the clinical spectrum of Henoch-Schönlein purpura in children. Clin Exp Rheumatol. 2004 Nov-Dec;22(6):781-4.
| PubMed |
Gonzalez-Gay MA, Calviño MC, Vazquez-Lopez ME, Garcia-Porrua C, Fernandez-Iglesias JL, Dierssen T, et al. Implications of upper respiratory tract infections and drugs in the clinical spectrum of Henoch-Schönlein purpura in children. Clin Exp Rheumatol. 2004 Nov-Dec;22(6):781-4.
| PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








