Key Words: hiperhidrosis, diabetes mellitus, glucemia
Abstract
We present a clinical case that we did not find described in literature and yet is quite common in primary care. The patient described is female with a diagnosis of diabetes mellitus treated with insulin and poor clinical response according to glycated haemoglobin measurements. In addition to the main diagnosis, she also shows excessive sweating in palms and feet, which explains why her blood sugar levels were wrong. This also led to treatment adjustments that were carried out with disregard to her true plasma glucose concentration. To conclude, this case report highlights the importance of treating subjects in lieu of separate conditions, as well as the need of a team approach to patients in care.
Introduction
This case is about the importance of team work as well as considering the patient’s health as a total and not as individual diseases. The same patient suffers two diseases and the symptoms of one of them (hyperhidrosis), implies the incorrect technique of self-analysis (capillary blood glucose), which is of great importance for the other (diabetes mellitus). The ease with which this type of mistakes can be made is absolutely crucial when dealing with patients, and produced a feeling of disquiet in our health team when discovered. This report is being published due to its curiosity and interest for other professionals. We hope that it helps to understand that we should treat our patients as taking into account their heath as a whole and not as individual diseases, and value team work. Health care physicians should stop and reflect on this.
Clincal case
The present is a case of a 43 year old woman that consults for routine health control, asymptomatic and no personal background history of interest. Paternal background history of diabetes mellitus type 2. When asked for a routine analysis we found glucose levels of 326 and she is diagnosed of diabetes mellitus. Glycated hemoglobin test is requested (Hba1c) with levels of 8.9mmol/mol. Treatment is started directly with 20 IU of insulin glargine and she is referred to nurse for diabetic education. Since glucose levels are under 80mg/dl she lowers IU of insulin as recommended.
Three months after we carry out glycated hemoglobin test again with no significant changes (9.1mmol/mol). We insist on hygienic and dietary measures and the correct handling of insulin according to blood glucose levels because the patient is suspected not to be handling it correctly.
We refer once again to nursing staff for a stricter control. They observe hyperhidrosis on both palms of her hands and the patient indicates that she has been diagnosed with primary palmoplantar hyperhidrosis, this fact was not noted on her medical history.
The patient refers palmoplantar hyperhidrosis symptoms since 10 to 11 years of age with other family members affected: mother and maternal aunt, no records of other family members. We observe that she takes her capillary blood glucose readings without drying her hands, and therefore the blood and sweat mix. The glucometer interprets lower levels of glucose in blood than the current so the patient lowered the IU of insulin, consequently the glycated hemoglobin did not improve. The nursing staff explains the importance of washing and drying her hands very well before blood glucose levels. Results improved after this insignificant change presenting a favorable development of her diabetes.
Argument
This case report faces several limitations. The first limitation is supposing that the clinical history was complete without being confirmed in addition to not seeing the palmar hyperhidrosis with the first capillary blood glucose. Another is assuming that the patient fails to follow the diet or she was not using insulin. In support of the health team we must say that the diagnosis, treatment and diabetic education were correct at all times.
Sweating is a required function for thermoregulation. Hyperhidrosis is an excessive sweating in response to heat or an emotional stimulus that exceeds a physiological stimulus. Even though hyperhidrosis does not generate risks for the patient, it is cause of psychosocial and labor disruptions. In addition it predisposes them to skin diseases [1].
We can classify hyperhidrosis in primary and secondary:
Primary: there is no adjacent cause. It normally appears at the beginning of childhood and extends during the rest of life declining through puberty and improving with age. There is no ratio difference between sex and race. The incidence is of 2.8% of the population, 30 to 50% of patients present family background history and therefore it is thought that there may be a genetic link [1],[3].
Secondary: the cause is an adjacent disease, infectious, endocrine or other.
We can also classify hyperhidrosis by anatomical regions (craniofacial, underarms, palms, soles), laterality (uni or bilateral), symmetric location and generalized or focal. There are three types of sweat glands [1],[2]:
- Eccrine glands: Most sweat glands are eccrine glands. They are regulated by cholinergic fibers of the sympathetic nervous system (acetylcholine and atropine). Distributed by palms of hand, soles of feet and maxilla region. The secretion is a hypotonic aqueous solution with a serous appearance. These are the glands involved in hyperhidrosis.
- Apocrine glands: These are less common. Regulated by the adrenergic system. Located in underarms, urogenital region and activated by puberty. The secretion is produced by hair follicles, it is viscous and malodorous.
- Apoeccrine glands: These are distributed only in underarms and have characteristics of both glands.
The cause of hyperhidrosis is not well known. There is no glandular hypertrophy or hyperplasia. It seems to be related with an overstimulation of the eccrine glands. Sweating is unpredictable, spontaneous and intermittent. Those who suffer hyperhidrosis have a lower sweating threshold. The location of the sweating involves hands in 96.4% of cases, soles in 80.7% and underarms in 71.3% [4].
In the case of hyperhidrosis and diabetes mellitus if we take into account that hands are affected in 96.4% and that secretion is aqueous and hypotonic as we have already explained, it is very important to consider it an influent factor in glucose values and highlight the importance of the correct technique in measuring of capillary glucose blood levels [5]. This technique includes cleaning the puncture area (controversial subject, this case is a relevant topic and currently a subject under discussion) [6], the correct hand hygiene before puncture, turning on and checking the calibration of the glucometer and improving blood flow by slightly massaging the selected area.
Since the first appearance of glucose measuring devices, technological developments are primarily intended to make its use easier, not only in hospitals and primary health care centers for medical staff use, but also for auto-analysis by patients for a better control of glucose values. Currently they are provided with higher accuracy and precision, being of a greater diagnostic value and reliability [7].
However in addition to the correct handling of the auto-analysis technique, we must consider that even being very reliable there are many and various concepts than can modify glucose values. We can classify them into endogenous conditions (table 1), exogenous conditions (table 2), technical conditions (table 3) and post analysis (error in transcription of data, loss of data, delays on the initial registration of results). The error ranges from 6 to 68% depending on the glucometer and the interferer studied. In the case of endogenous conditions we would like to highlight household manipulation (juice, fruits, sweets and others) or at the health care center where being attended (for example furniture with traces of dextrose) [8],[9],[10],[11].
Table 1 Endogenous conditions that affect blood glucose values
Table 2: Exogenous conditions that affect blood glucose values.
Table 3. Technical conditions that affect blood glucose values.
The use of new procedures such as continuous glucose monitoring contributes information on values by monitoring every five minutes, and can program alarms if these pass the established levels. These devices are connected to a sensor that is inserted in interstitial fluid, usually in the abdomen and together (transmitter and sensor) are of the size of a two euro coin. Despite the 288 measurements a day that can be carried out, two to four capillary blood glucose levels a day are necessary because these devices need to be calibrated at least every twelve hours. They are very useful in nocturnal hypoglycemia and for blood glucose profiles. They often are associated to a maintenance therapy that mainly pumps short acting insulin to the subcutaneous tissue. This is carried out continuously with amounts of insulin that can cover basic needs. These doses can substitute the basic functions of beta cells adapted as much as possible to the physiological situation.
The present day devices are small and lightweight (similar to a mobile phone), programmable and easy to use, able to improve glucose blood level controls and minimize risks of hypoglycemia. The main indications are diabetes type 1 with unstable blood glucose levels with difficult control, and in the case of frequent or unnoticed severe hypoglycemia [12],[13]. The abdomen is normally the zone of choice.
Henceforth, not only is it important to use a correct technique but also to consider the whole chain or factors that can modify the blood glucose values obtained by capillary puncture. This is necessary even when using new procedures such as continuous monitoring of glucose or insulin pumps.
Conclusion
A correct clinical history of patients is crucial despite the lack of time. Likewise it is essential to evaluate them as a whole, we must remember that we are not dealing with diseases but patients. Besides this, a medical staff does not work alone; team work is primary in health care. In this case in particular, both nurse and doctor worked correctly but hyperhidrosis was taken into account the disease did not improve. Both doctor and nurse treated the disease and did not the patient.
Notes
From the editor
This article was originally submitted in Spanish and was translated into English by the authors. The Journal has not copyedited this version.
Ethical issues
The patient that is reported in this article has given written, informed consent to publish the case in the Journal.
Conflicts of interests
The authors have completed the ICMJE Conflict of Interest form and have no relevant interests to declare.

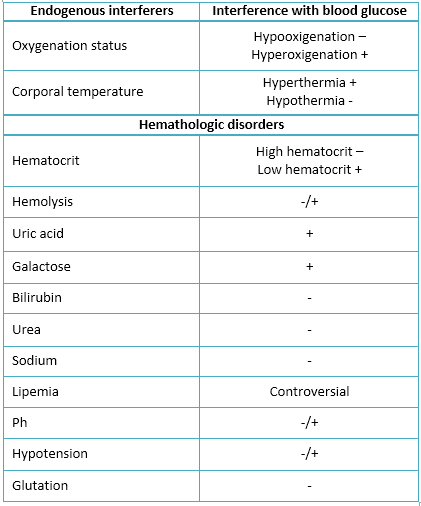 Table 1 Endogenous conditions that affect blood glucose values
Table 1 Endogenous conditions that affect blood glucose values

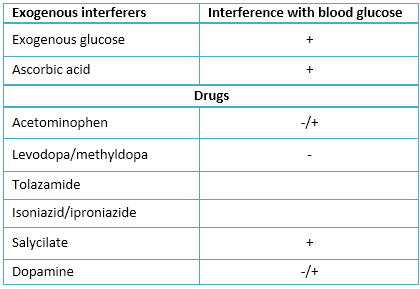 Table 2: Exogenous conditions that affect blood glucose values.
Table 2: Exogenous conditions that affect blood glucose values.

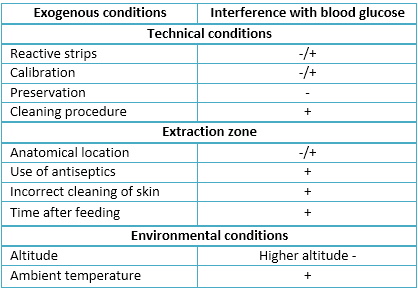 Table 3. Technical conditions that affect blood glucose values.
Table 3. Technical conditions that affect blood glucose values.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Se da cuenta de un caso clínico que puede presentarse con frecuencia en atención primaria, aunque no se registran casos similares en la literatura. Se trata de una mujer con diagnóstico de diabetes mellitus en tratamiento con insulina y con mala evolución según las hemoglobinas glicosiladas. Además del diagnóstico principal, también presenta hiperhidrosis palmo-plantar, lo que conducía a error en los controles glucémicos. Ello es de gran importancia, dado que se ajustaba tratamiento sin considerar que el control no se realizaba de forma adecuada. De este reporte se concluye la relevancia de tratar al paciente como tal y no como patologías individuales, así como la importancia del trabajo en equipo.
 Authors:
Eva Buller Viqueira[1], Juana Cabello Pulido[2], José Antonio Jiménez Fernández[1]
Authors:
Eva Buller Viqueira[1], Juana Cabello Pulido[2], José Antonio Jiménez Fernández[1]
Affiliation:
[1] Centro de Salud de Barbate, Cádiz, España
[2] Centro de Salud de Vejer, Vejer de la Frontera, Cádiz, España
E-mail: miji_77@yahoo.com
Author address:
[1] Avda. Del Mar s/n
cp 11.160,
Barbate, Cádiz

Citation: Buller Viqueira E, Cabello Pulido J, Jiménez Fernández JA. Case report of excessive hand sweating that alters blood sugar measurements. Medwave 2015 Jul;15(6):e6187 doi: 10.5867/medwave.2015.06.6187
Submission date: 24/4/2015
Acceptance date: 30/6/2015
Publication date: 21/7/2015
Origin: not requested
Type of review: reviewed by two external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Fernández DG, Oliva NP. Actualización en hiperhidrosis focal primaria. Med Cutan Ibero Lat Am. 2012;40(6);173-180. | Link |
- Callejas MA, Grimalt R, Cladellas E. Actualizacion en hiperhidrosis. Actas dermosifiliogr. 2010;101(2);110-118. | Link |
- Ro KM, Cantor RM, Lange KL, Ahn SS. Palmar Hyperhidrosis: evidence of genetic transmission. J Vasc Surg. 2002;35:382-6. | Link |
- Ramos R, Moya J, Pérez J, Villalonga R, Morera R, Pujol R, Ferrre G. Hiperhidrosis pirmaria: estudio prospectivo de 338 pacientes. Med Clin (Barc). 2003;121(6):201-203. | Link |
- Perry AG, Potter PA. Guía Mosby de técnicas y procedimientos en enfermería. Séptima Edición. Barcelona, España: Elsevier; 2011.
- Hurtado FL. Limpieza y/o desinfección previa a determinación de glucemia capilar. Enfermería Docente. 2010;92:39. | Link |
- Parramón M. Particularidades de la medición de la glucemia capilar: aspectos técnicos, clínicos y legales. Endocrinol Nutr. 2004;51(7):433-439. | Link |
- Campos Palomo AD, Campos Palomo LD. Enfermería y variables en el autocontrol de glucemia capilar. Resumen de evidencias científicas. Enfermería Docente. 2013;101:41-44. | Link |
- Kinchiku S, Kotani K, Kajiya S, Yodo K, Maruguchi Y, Uenomach H. Influence of ambient temperature on the correlation between self-monitoring of blood glucose and plasma glucose values in diabetes management. J Prim Health Care. 2012;4(4):294-298. | PubMed |
- Polo Martín M, Palomo de los Reyes MJ, Baeza Nadal MV, Parras García de León N, Aguilar Florit JL, Julián Jiménez A. Correlación entre glucemia capilar y venosa en urgencias: un apunte metodológico. Emergencias: Revista de la Sociedad Española de Medicina de Urgencias y Emergencias. 2008;20(5):332-334. | Link |
- Izquierdo Quince F, Fatela Cantillo D, Chueca Rodríguez MP, Díaz Ondina M. Detección de interferencias y otros errores en la medición en la medición de la glucemia en glucómetros portátiles. Documentos de la SEQC – Diciembre 2012.
- Vázquez F, Barrio R, Goñi MJ, Díaz-Soto G, Muela IS, Blanco CG. Documento de consenso sobre el tratamiento con infusión subcutánea continua de insulina en el medio hospitalario. Avances en Diabetología. 2015. | Link |
- Papargyri P, Rodríguez SO, Hernández JJC, Álvarez MTM, Córdova JMR, Gómez MD, et al. Estudio observacional de infusión subcutánea continua de insulina a lo largo de 7 años en el tratamiento de la diabetes mellitus tipo 1. Endocrinología y Nutrición. 2014;61(3):141-146. | Link |
 Fernández DG, Oliva NP. Actualización en hiperhidrosis focal primaria. Med Cutan Ibero Lat Am. 2012;40(6);173-180. | Link |
Fernández DG, Oliva NP. Actualización en hiperhidrosis focal primaria. Med Cutan Ibero Lat Am. 2012;40(6);173-180. | Link | Callejas MA, Grimalt R, Cladellas E. Actualizacion en hiperhidrosis. Actas dermosifiliogr. 2010;101(2);110-118. | Link |
Callejas MA, Grimalt R, Cladellas E. Actualizacion en hiperhidrosis. Actas dermosifiliogr. 2010;101(2);110-118. | Link | Ro KM, Cantor RM, Lange KL, Ahn SS. Palmar Hyperhidrosis: evidence of genetic transmission. J Vasc Surg. 2002;35:382-6. | Link |
Ro KM, Cantor RM, Lange KL, Ahn SS. Palmar Hyperhidrosis: evidence of genetic transmission. J Vasc Surg. 2002;35:382-6. | Link | Ramos R, Moya J, Pérez J, Villalonga R, Morera R, Pujol R, Ferrre G. Hiperhidrosis pirmaria: estudio prospectivo de 338 pacientes. Med Clin (Barc). 2003;121(6):201-203. | Link |
Ramos R, Moya J, Pérez J, Villalonga R, Morera R, Pujol R, Ferrre G. Hiperhidrosis pirmaria: estudio prospectivo de 338 pacientes. Med Clin (Barc). 2003;121(6):201-203. | Link | Perry AG, Potter PA. Guía Mosby de técnicas y procedimientos en enfermería. Séptima Edición. Barcelona, España: Elsevier; 2011.
Perry AG, Potter PA. Guía Mosby de técnicas y procedimientos en enfermería. Séptima Edición. Barcelona, España: Elsevier; 2011.  Hurtado FL. Limpieza y/o desinfección previa a determinación de glucemia capilar. Enfermería Docente. 2010;92:39. | Link |
Hurtado FL. Limpieza y/o desinfección previa a determinación de glucemia capilar. Enfermería Docente. 2010;92:39. | Link | Parramón M. Particularidades de la medición de la glucemia capilar: aspectos técnicos, clínicos y legales. Endocrinol Nutr. 2004;51(7):433-439. | Link |
Parramón M. Particularidades de la medición de la glucemia capilar: aspectos técnicos, clínicos y legales. Endocrinol Nutr. 2004;51(7):433-439. | Link | Campos Palomo AD, Campos Palomo LD. Enfermería y variables en el autocontrol de glucemia capilar. Resumen de evidencias científicas. Enfermería Docente. 2013;101:41-44. | Link |
Campos Palomo AD, Campos Palomo LD. Enfermería y variables en el autocontrol de glucemia capilar. Resumen de evidencias científicas. Enfermería Docente. 2013;101:41-44. | Link | Kinchiku S, Kotani K, Kajiya S, Yodo K, Maruguchi Y, Uenomach H. Influence of ambient temperature on the correlation between self-monitoring of blood glucose and plasma glucose values in diabetes management. J Prim Health Care. 2012;4(4):294-298. | PubMed |
Kinchiku S, Kotani K, Kajiya S, Yodo K, Maruguchi Y, Uenomach H. Influence of ambient temperature on the correlation between self-monitoring of blood glucose and plasma glucose values in diabetes management. J Prim Health Care. 2012;4(4):294-298. | PubMed | Polo Martín M, Palomo de los Reyes MJ, Baeza Nadal MV, Parras García de León N, Aguilar Florit JL, Julián Jiménez A. Correlación entre glucemia capilar y venosa en urgencias: un apunte metodológico. Emergencias: Revista de la Sociedad Española de Medicina de Urgencias y Emergencias. 2008;20(5):332-334. | Link |
Polo Martín M, Palomo de los Reyes MJ, Baeza Nadal MV, Parras García de León N, Aguilar Florit JL, Julián Jiménez A. Correlación entre glucemia capilar y venosa en urgencias: un apunte metodológico. Emergencias: Revista de la Sociedad Española de Medicina de Urgencias y Emergencias. 2008;20(5):332-334. | Link | Izquierdo Quince F, Fatela Cantillo D, Chueca Rodríguez MP, Díaz Ondina M. Detección de interferencias y otros errores en la medición en la medición de la glucemia en glucómetros portátiles. Documentos de la SEQC – Diciembre 2012.
Izquierdo Quince F, Fatela Cantillo D, Chueca Rodríguez MP, Díaz Ondina M. Detección de interferencias y otros errores en la medición en la medición de la glucemia en glucómetros portátiles. Documentos de la SEQC – Diciembre 2012.  Vázquez F, Barrio R, Goñi MJ, Díaz-Soto G, Muela IS, Blanco CG. Documento de consenso sobre el tratamiento con infusión subcutánea continua de insulina en el medio hospitalario. Avances en Diabetología. 2015. | Link |
Vázquez F, Barrio R, Goñi MJ, Díaz-Soto G, Muela IS, Blanco CG. Documento de consenso sobre el tratamiento con infusión subcutánea continua de insulina en el medio hospitalario. Avances en Diabetología. 2015. | Link | Papargyri P, Rodríguez SO, Hernández JJC, Álvarez MTM, Córdova JMR, Gómez MD, et al. Estudio observacional de infusión subcutánea continua de insulina a lo largo de 7 años en el tratamiento de la diabetes mellitus tipo 1. Endocrinología y Nutrición. 2014;61(3):141-146. | Link |
Papargyri P, Rodríguez SO, Hernández JJC, Álvarez MTM, Córdova JMR, Gómez MD, et al. Estudio observacional de infusión subcutánea continua de insulina a lo largo de 7 años en el tratamiento de la diabetes mellitus tipo 1. Endocrinología y Nutrición. 2014;61(3):141-146. | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








