
 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
INTRODUCTION
Transurethral resection is currently considered as standard endoscopic treatment for lower urinary tract obstruction due to benign hyperplasia under 80 cc. Monopolar resection loops has been traditionally used but bipolar energy has recently displaced precedent technology. The purpose of this summary is to evaluate the efficacy and safety of both technologies.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
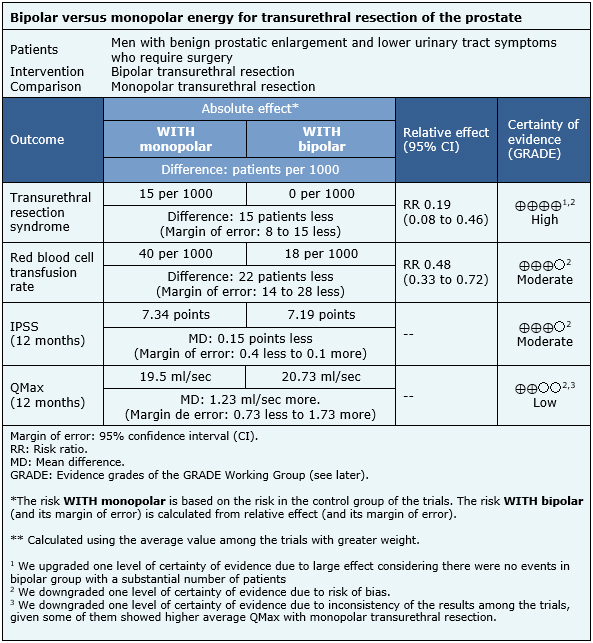
We identified 13 systematic reviews including 32 primary studies, among them 31 randomized trials. We concluded although there may be no difference in terms of efficacy among both techniques, the use of bipolar energy reduces the incidence of transurethral resection syndrome and probably reduces the risk of bleeding that requires red blood cell transfusion.
Lower urinary tract obstruction caused by benign prostatic hyperplasia is a prevalent condition that causes bothersome symptoms and impaired quality of life. Occasionally, it can lead to complications that determine morbidity and mortality.
Transurethral resection has been traditionally considered standard endoscopic treatment for prostates of less than 80cc, being monopolar loops the most broadly used. However, its use is not free of complications such as transurethral resection syndrome, a clinical entity caused by the absorption of hypoosmolar fluids used in monopolar techniques. Bipolar diathermy emerged as an alternative that could be associated with a lower incidence of complications, provided by the use of isotonic solutions for the resection of the prostate. The purpose of this summary is to evaluate the clinical efficacy and safety of both techniques.
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We identified 13 systematic reviews [1],[2],[3],[4],[5],[6],[7], This table and the review in general are based on the latter, since the observational study [57] did not improve the certainty of the evidence or provided additional relevant information. |
|
What types of patients were included* |
Patients with lower urinary tract obstruction due to benign prostatic hyperplasia who required endoscopic treatment were included. Patients with suspicion of prostate cancer or other causes of lower urinary tract obstruction were excluded. Average age ranged between 59 and 73 years in the different trials. Average prostate volume ranged between 39.5 and 82.5 cc. |
|
What types of interventions were included* |
Seventeen trials [15],[22],[26],[27],[31],[38],[39],[40],[42], Eight trials [14],[16],[20],[28],[32],[41],[50],[55] used Olympus TURis bipolar resectoscope. Three trials [43],[49],[58] used Vista CTR bipolar resectoscope. One trial [45], used AUTOCON II Storz resectoscope. The systematic reviews identified did not report which monopolar resectoscope was used in each trial. |
|
What types of outcomes |
Multiple outcomes were measured in the trials. They were grouped in the systematic reviews as follows: magnitude of the obstruction (maximum urinary output (QMax) in ml/seg measured by uroflowmetry, postvoid residual volume, symptoms and quality of life using the International Prostate Symptoms Score (IPSS). Perioperative parameters (duration of surgery, hospital stay, urinary catheterization time, red blood cell transfusion rate and incidence of transurethral resection syndrome were also measured), and late postoperative complications such as erectile dysfunction, urethral stenosis, bladder neck contracture, urinary incontinence, reintervention rate, among others were assessed as well. Follow-up median among the trials was 12 months with a range of 1 to 60 months. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
The information about the effects of bipolar versus monopolar transurethral resection of the prostate is based on 31 randomized trials that include 4670 patients.
Twenty-five trials reported red blood cell transfusion rate (3585 patients) [14],[15],[16],[19],[20],[22],[26],[27],[28],[30],[31],[32],[39],[42],[44],[45],[49],[50],[53],[54],[58],[59],[60],[61],[62], 25 trials reported the incidence of transurethral resection syndrome (3436 patients), [14],[15],[16],[19],[20],[22],[26],[27],[30],[31],[32],[39],[42],[44],[45],[49],[50],[53],[54],[55],[58],[59],[60],[61],[62], 11 trials measured IPSS at 12 months (1452 patients) [16],[20],[27],[39],[45],[53],[56],[57],[59],[60],[62] and 13 trials measured QMax at 12 months (1649 patients) [16],[19],[20],[27],[31],[39],[45],[53],[56],[57],[59],[60],[62].
The summary of findings is:
| Following the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
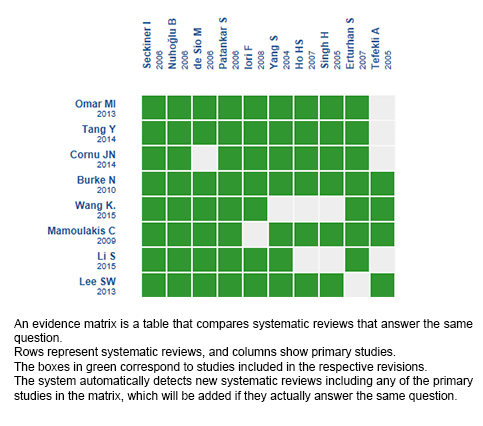
Follow the link to access the interactive version: Bipolar versus monopolar transurethral resection of the prostate for benign hyperplasia
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
Transurethral resection is currently considered as standard endoscopic treatment for lower urinary tract obstruction due to benign hyperplasia under 80 cc. Monopolar resection loops has been traditionally used but bipolar energy has recently displaced precedent technology. The purpose of this summary is to evaluate the efficacy and safety of both technologies.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified 13 systematic reviews including 32 primary studies, among them 31 randomized trials. We concluded although there may be no difference in terms of efficacy among both techniques, the use of bipolar energy reduces the incidence of transurethral resection syndrome and probably reduces the risk of bleeding that requires red blood cell transfusion.
 Autores:
Gabriel Inzunza[1,2], Gabriel Rada[2,3,4,5,6], Alejandro Majerson[2,7]
Autores:
Gabriel Inzunza[1,2], Gabriel Rada[2,3,4,5,6], Alejandro Majerson[2,7]

Citación: Inzunza G, Rada G, Majerson A. Bipolar or monopolar transurethral resection for benign prostatic hyperplasia?. Medwave 2018 Ene-Feb;18(1):e7134 doi: 10.5867/medwave.2018.01.7134
Fecha de envío: 26/12/2017
Fecha de aceptación: 29/12/2017
Fecha de publicación: 17/1/2018
Origen: Este artículo es producto del Epistemonikos Evidence Synthesis Project de la Fundación Epistemonikos, en colaboración con Medwave para su publicación.
Tipo de revisión: Con revisión por pares sin ciego por parte del equipo metodológico del Epistemonikos Evidence Synthesis Project.

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, Speakman MJ, Stief CG. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. European urology. 2010;58(3):384-97.
Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, Speakman MJ, Stief CG. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. European urology. 2010;58(3):384-97.  Baazeem A, Elhilali MM. Surgical management of benign prostatic hyperplasia: current evidence. Nature clinical practice. Urology. 2008;5(10):540-9.
Baazeem A, Elhilali MM. Surgical management of benign prostatic hyperplasia: current evidence. Nature clinical practice. Urology. 2008;5(10):540-9.  Burke N, Whelan JP, Goeree L, Hopkins RB, Campbell K, Goeree R, Tarride JE. Systematic review and meta-analysis of transurethral resection of the prostate versus minimally invasive procedures for the treatment of benign prostatic obstruction. Urology. 2010;75(5):1015-22.
Burke N, Whelan JP, Goeree L, Hopkins RB, Campbell K, Goeree R, Tarride JE. Systematic review and meta-analysis of transurethral resection of the prostate versus minimally invasive procedures for the treatment of benign prostatic obstruction. Urology. 2010;75(5):1015-22.  Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, McVary K, Novara G, Woo H, Madersbacher S. A Systematic Review and Meta-analysis of Functional Outcomes and Complications Following Transurethral Procedures for Lower Urinary Tract Symptoms Resulting from Benign Prostatic Obstruction: An Update. European urology. 2014;67(6):1066-96.
Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, McVary K, Novara G, Woo H, Madersbacher S. A Systematic Review and Meta-analysis of Functional Outcomes and Complications Following Transurethral Procedures for Lower Urinary Tract Symptoms Resulting from Benign Prostatic Obstruction: An Update. European urology. 2014;67(6):1066-96.  da Silva RD, Bidikov L, Michaels W, Gustafson D, Molina WR, Kim FJ. Bipolar energy in the treatment of benign prostatic hyperplasia: a current systematic review of the literature. The Canadian journal of urology. 2015;22(5 Suppl 1):30-44.
da Silva RD, Bidikov L, Michaels W, Gustafson D, Molina WR, Kim FJ. Bipolar energy in the treatment of benign prostatic hyperplasia: a current systematic review of the literature. The Canadian journal of urology. 2015;22(5 Suppl 1):30-44.  Health Quality Ontario. Energy delivery systems for treatment of benign prostatic hyperplasia: an evidence-based analysis. Ontario health technology assessment series. 2006;6(17):1-121.
Health Quality Ontario. Energy delivery systems for treatment of benign prostatic hyperplasia: an evidence-based analysis. Ontario health technology assessment series. 2006;6(17):1-121.  Lee SW, Choi JB, Lee KS, Kim TH, Son H, Jung TY, Oh SJ, Jeong HJ, Bae JH, Lee YS, Kim JC. Transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement: a quality and meta-analysis. International neurourology journal. 2013;17(2):59-66.
Lee SW, Choi JB, Lee KS, Kim TH, Son H, Jung TY, Oh SJ, Jeong HJ, Bae JH, Lee YS, Kim JC. Transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement: a quality and meta-analysis. International neurourology journal. 2013;17(2):59-66.  Li S, Kwong JS, Zeng XT, Ruan XL, Liu TZ, Weng H, Guo Y, Xu C, Yan JZ, Meng XY, Wang XH. Plasmakinetic resection technology for the treatment of benign prostatic hyperplasia: evidence from a systematic review and meta-analysis. Scientific reports. 2015;5:12002.
Li S, Kwong JS, Zeng XT, Ruan XL, Liu TZ, Weng H, Guo Y, Xu C, Yan JZ, Meng XY, Wang XH. Plasmakinetic resection technology for the treatment of benign prostatic hyperplasia: evidence from a systematic review and meta-analysis. Scientific reports. 2015;5:12002.  Lourenco T, Pickard R, Vale L, Grant A, Fraser C, MacLennan G, N'Dow J, Benign Prostatic Enlargement team. Alternative approaches to endoscopic ablation for benign enlargement of the prostate: systematic review of randomised controlled trials. BMJ (Clinical research ed.). 2008;337(7660):a449.
Lourenco T, Pickard R, Vale L, Grant A, Fraser C, MacLennan G, N'Dow J, Benign Prostatic Enlargement team. Alternative approaches to endoscopic ablation for benign enlargement of the prostate: systematic review of randomised controlled trials. BMJ (Clinical research ed.). 2008;337(7660):a449.  Mamoulakis C, Ubbink DT, de la Rosette JJ. Bipolar versus monopolar transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. European urology. 2009;56(5):798-809.
Mamoulakis C, Ubbink DT, de la Rosette JJ. Bipolar versus monopolar transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. European urology. 2009;56(5):798-809.  Omar MI, Lam T, Alexander CE, Graham J, Mamoulakis C, Imamura M, Maclennan S, Stewart F, N'dow J. Systematic review and meta-analysis of the clinical effectiveness of bipolar compared with monopolar transurethral resection of the prostate (TURP). BJU international. 2013;113(1):24-35.
Omar MI, Lam T, Alexander CE, Graham J, Mamoulakis C, Imamura M, Maclennan S, Stewart F, N'dow J. Systematic review and meta-analysis of the clinical effectiveness of bipolar compared with monopolar transurethral resection of the prostate (TURP). BJU international. 2013;113(1):24-35.  Tang Y, Li J, Pu C, Bai Y, Yuan H, Wei Q, Han P. Bipolar transurethral resection versus monopolar transurethral resection for benign prostatic hypertrophy: a systematic review and meta-analysis. Journal of endourology / Endourological Society. 2014;28(9):1107-14.
Tang Y, Li J, Pu C, Bai Y, Yuan H, Wei Q, Han P. Bipolar transurethral resection versus monopolar transurethral resection for benign prostatic hypertrophy: a systematic review and meta-analysis. Journal of endourology / Endourological Society. 2014;28(9):1107-14.  Wang K., Li Y., Teng J.-F., Zhou H.-Y., Xu D.-F., Fan Y.. Transurethral plasmakinetic resection of the prostate is a reliable minimal invasive technique for benign prostate hyperplasia: A meta-analysis of randomized controlled trials. Asian Journal of Andrology. 2015;17(1):135-142.
Wang K., Li Y., Teng J.-F., Zhou H.-Y., Xu D.-F., Fan Y.. Transurethral plasmakinetic resection of the prostate is a reliable minimal invasive technique for benign prostate hyperplasia: A meta-analysis of randomized controlled trials. Asian Journal of Andrology. 2015;17(1):135-142.  Abascal Junquera JM, Cecchini Rosell L, Salvador Lacambra C, Martos Calvo R, Celma Domenech A, Morote Robles J. [Bipolar versus monopolar transurethral resection of the prostate: peroperative analysis of the results]. Actas urologicas espanolas. 2006;30(7):661-6.
Abascal Junquera JM, Cecchini Rosell L, Salvador Lacambra C, Martos Calvo R, Celma Domenech A, Morote Robles J. [Bipolar versus monopolar transurethral resection of the prostate: peroperative analysis of the results]. Actas urologicas espanolas. 2006;30(7):661-6.  Akçayöz M, Kaygisiz O, Akdemir O, Aki FT, Adsan O, Cetinkaya M. Comparison of transurethral resection and plasmakinetic transurethral resection applications with regard to fluid absorption amounts in benign prostate hyperplasia. Urologia internationalis. 2006;77(2):143-7.
Akçayöz M, Kaygisiz O, Akdemir O, Aki FT, Adsan O, Cetinkaya M. Comparison of transurethral resection and plasmakinetic transurethral resection applications with regard to fluid absorption amounts in benign prostate hyperplasia. Urologia internationalis. 2006;77(2):143-7.  Akman T, Binbay M, Tekinarslan E, Tepeler A, Akcay M, Ozgor F, Ugurlu M, Muslumanoglu A. Effects of bipolar and monopolar transurethral resection of the prostate on urinary and erectile function: a prospective randomized comparative study. BJU international. 2013;111(1):129-36.
Akman T, Binbay M, Tekinarslan E, Tepeler A, Akcay M, Ozgor F, Ugurlu M, Muslumanoglu A. Effects of bipolar and monopolar transurethral resection of the prostate on urinary and erectile function: a prospective randomized comparative study. BJU international. 2013;111(1):129-36.  Muslumanoglu AY, Yuruk E, Binbay M, Akman T. Transurethral resection of prostate with plasmakinetic energy: 100 months results of a prospective randomized trial. BJU Int 2012;110:546–9.
Muslumanoglu AY, Yuruk E, Binbay M, Akman T. Transurethral resection of prostate with plasmakinetic energy: 100 months results of a prospective randomized trial. BJU Int 2012;110:546–9.  Tefekli A, Muslumanoglu AY, Baykal M, Binbay M, Tas A, et al. A hybrid technique using bipolar energy in transurethral prostate surgery: a prospective, randomized comparison. J Urol 2005; 174: 1339–43.
Tefekli A, Muslumanoglu AY, Baykal M, Binbay M, Tas A, et al. A hybrid technique using bipolar energy in transurethral prostate surgery: a prospective, randomized comparison. J Urol 2005; 174: 1339–43.  Bhansali M, Patankar S, Dobhada S, Khaladkar S. Management of large (>60 g) prostate gland: PlasmaKinetic Superpulse (bipolar) versus conventional (monopolar) transurethral resection of the prostate. Journal of endourology / Endourological Society. 2009;23(1):141-5.
Bhansali M, Patankar S, Dobhada S, Khaladkar S. Management of large (>60 g) prostate gland: PlasmaKinetic Superpulse (bipolar) versus conventional (monopolar) transurethral resection of the prostate. Journal of endourology / Endourological Society. 2009;23(1):141-5.  Chen Q, Zhang L, Fan QL, Zhou J, Peng YB, Wang Z. Bipolar transurethral resection in saline vs traditional monopolar resection of the prostate: results of a randomized trial with a 2-year follow-up. BJU international. 2010;106(9):1339-43.
Chen Q, Zhang L, Fan QL, Zhou J, Peng YB, Wang Z. Bipolar transurethral resection in saline vs traditional monopolar resection of the prostate: results of a randomized trial with a 2-year follow-up. BJU international. 2010;106(9):1339-43.  Chen Q, Zhang L, Liu YJ, Lu JD, Wang GM. Bipolar transurethral resection in saline system versus traditional monopolar resection system in treating large-volume benign prostatic hyperplasia. Urol Int 2009; 83: 55–9.
Chen Q, Zhang L, Liu YJ, Lu JD, Wang GM. Bipolar transurethral resection in saline system versus traditional monopolar resection system in treating large-volume benign prostatic hyperplasia. Urol Int 2009; 83: 55–9.  de Sio M, Autorino R, Quarto G, Damiano R, Perdonà S, di Lorenzo G, Mordente S, D'Armiento M. Gyrus bipolar versus standard monopolar transurethral resection of the prostate: a randomized prospective trial. Urology. 2006;67(1):69-72.
de Sio M, Autorino R, Quarto G, Damiano R, Perdonà S, di Lorenzo G, Mordente S, D'Armiento M. Gyrus bipolar versus standard monopolar transurethral resection of the prostate: a randomized prospective trial. Urology. 2006;67(1):69-72.  Autorino R, Damiano R, Di LG et al. Four-year outcome of a prospective randomised trial comparing bipolar plasmakinetic and monopolar transurethral resection of the prostate. Eur Urol 2009; 55: 922–31.
Autorino R, Damiano R, Di LG et al. Four-year outcome of a prospective randomised trial comparing bipolar plasmakinetic and monopolar transurethral resection of the prostate. Eur Urol 2009; 55: 922–31.  Autorino R, De Sio M, D’Armiento M. Bipolar plasmakinetic technology for the treatment of symptomatic benign prostatic hyperplasia: evidence beyond marketing hype? BJU Int 2007; 100: 983–5.
Autorino R, De Sio M, D’Armiento M. Bipolar plasmakinetic technology for the treatment of symptomatic benign prostatic hyperplasia: evidence beyond marketing hype? BJU Int 2007; 100: 983–5.  De Sio M, Autorino R, Quarto G, et al. Gyrus bipolar versus standard monopolar transurethral resection of the prostate: a randomized prospective trial [Abstract no. MP10-01]. J Endourol. 2005; 19(suppl 1):A43.
De Sio M, Autorino R, Quarto G, et al. Gyrus bipolar versus standard monopolar transurethral resection of the prostate: a randomized prospective trial [Abstract no. MP10-01]. J Endourol. 2005; 19(suppl 1):A43.  Engeler DS, Schwab C, Neyer M, Grun T, Reissigl A, et al. Bipolar versus monopolar TURP: a prospective controlled study at two urology centers. Prostate Cancer Prostatic Dis 2010; 13: 285–91.
Engeler DS, Schwab C, Neyer M, Grun T, Reissigl A, et al. Bipolar versus monopolar TURP: a prospective controlled study at two urology centers. Prostate Cancer Prostatic Dis 2010; 13: 285–91.  Erturhan S, Erbagci A, Seckiner I, Yagci F, Ustun A. Plasmakinetic resection of the prostate versus standard transurethral resection of the prostate: a prospective randomized trial with 1-year follow-up. Prostate cancer and prostatic diseases. 2007;10(1):97-100.
Erturhan S, Erbagci A, Seckiner I, Yagci F, Ustun A. Plasmakinetic resection of the prostate versus standard transurethral resection of the prostate: a prospective randomized trial with 1-year follow-up. Prostate cancer and prostatic diseases. 2007;10(1):97-100.  Fagerström T, Nyman CR, Hahn RG. Complications and clinical outcome 18 months after bipolar and monopolar transurethral resection of the prostate. Journal of endourology / Endourological Society. 2011;25(6):1043-9.
Fagerström T, Nyman CR, Hahn RG. Complications and clinical outcome 18 months after bipolar and monopolar transurethral resection of the prostate. Journal of endourology / Endourological Society. 2011;25(6):1043-9.  Fagerstrom T, Nyman CR, Hahn RG. Bipolar transurethral resection of the prostate causes less bleeding than the monopolar technique: a single-centre randomized trial of 202 patients. BJU Int 2010; 105:1560–4.
Fagerstrom T, Nyman CR, Hahn RG. Bipolar transurethral resection of the prostate causes less bleeding than the monopolar technique: a single-centre randomized trial of 202 patients. BJU Int 2010; 105:1560–4.  Geavlete B, Georgescu D, Multescu R, Stanescu F, Jecu M, Geavlete P. Bipolar plasma vaporization vs monopolar and bipolar TURP-A prospective, randomized, long-term comparison. Urology. 2011;78(4):930-5.
Geavlete B, Georgescu D, Multescu R, Stanescu F, Jecu M, Geavlete P. Bipolar plasma vaporization vs monopolar and bipolar TURP-A prospective, randomized, long-term comparison. Urology. 2011;78(4):930-5.  Giulianelli R, Albanesi L, Attisani F, Gentile BC, Vincenti G, Pisanti F, Shestani T, Mavilla L, Granata D, Schettini M. Comparative randomized study on the efficaciousness of endoscopic bipolar prostate resection versus monopolar resection technique. 3 year follow-up. Archivio italiano di urologia, andrologia: organo ufficiale [di] Società italiana di ecografia urologica e nefrologica / Associazione ricerche in urologia. 2013;85(2):86-91.
Giulianelli R, Albanesi L, Attisani F, Gentile BC, Vincenti G, Pisanti F, Shestani T, Mavilla L, Granata D, Schettini M. Comparative randomized study on the efficaciousness of endoscopic bipolar prostate resection versus monopolar resection technique. 3 year follow-up. Archivio italiano di urologia, andrologia: organo ufficiale [di] Società italiana di ecografia urologica e nefrologica / Associazione ricerche in urologia. 2013;85(2):86-91.  Ho HS, Yip SK, Lim KB, Fook S, Foo KT, Cheng CW. A prospective randomized study comparing monopolar and bipolar transurethral resection of prostate using transurethral resection in saline (TURIS) system. European urology. 2007;52(2):517-22.
Ho HS, Yip SK, Lim KB, Fook S, Foo KT, Cheng CW. A prospective randomized study comparing monopolar and bipolar transurethral resection of prostate using transurethral resection in saline (TURIS) system. European urology. 2007;52(2):517-22.  Ho H, Yip S, Lim K, Foo K, Cheng C. A prospective randomized controlled trial comparing bipolar transurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: a 1 year’s clinical efficacy and safety. J Urol 2006; 175 (Suppl. 4): 461.
Ho H, Yip S, Lim K, Foo K, Cheng C. A prospective randomized controlled trial comparing bipolar transurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: a 1 year’s clinical efficacy and safety. J Urol 2006; 175 (Suppl. 4): 461.  Ho H, Yip S, Lim K, Foo K, Cheng C. A prospective randomized controlled trial comparing bipolar transurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: a 1 year’s clinical efficacy and safety. Eur Urol Suppl 2006; 5: 308.
Ho H, Yip S, Lim K, Foo K, Cheng C. A prospective randomized controlled trial comparing bipolar transurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: a 1 year’s clinical efficacy and safety. Eur Urol Suppl 2006; 5: 308.  Ho H, Yip S, Lim K, et al. A prospective randomised controlled trial comparing bipolartransurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: 1 year’s clinical efficacy and safety [Abstract no. 1143]. Eur Urol Suppl. 2006;5:308.
Ho H, Yip S, Lim K, et al. A prospective randomised controlled trial comparing bipolartransurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: 1 year’s clinical efficacy and safety [Abstract no. 1143]. Eur Urol Suppl. 2006;5:308.  Ho H, Yip S, Foo KT, et al. A prospective randomized controlled trial comparing bipolar transurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: a 1 year’s clinical efficacy and safety [Abstract no. MP10-18]. J Endourol. 2005; 19(suppl 1):A47.
Ho H, Yip S, Foo KT, et al. A prospective randomized controlled trial comparing bipolar transurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: a 1 year’s clinical efficacy and safety [Abstract no. MP10-18]. J Endourol. 2005; 19(suppl 1):A47.  Ho H, Yip S, Lim K, et al. A prospective randomized controlled trial comparing bipolar transurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: a 1 year’s clinical efficacy and safety [Abstract no. 1429]. J Urol. 2006;175(suppl4):S461.
Ho H, Yip S, Lim K, et al. A prospective randomized controlled trial comparing bipolar transurethral resection in saline (TURIS) system and conventional monopolar transurethral resection of prostate in men with benign prostate hyperplasia: a 1 year’s clinical efficacy and safety [Abstract no. 1429]. J Urol. 2006;175(suppl4):S461.  Huang X, Wang L, Wang XH, Shi HB, Zhang XJ, Yu ZY. Bipolar transurethral resection of the prostate causes deeper coagulation depth and less bleeding than monopolar transurethral prostatectomy. Urology. 2012;80(5):1116-20.
Huang X, Wang L, Wang XH, Shi HB, Zhang XJ, Yu ZY. Bipolar transurethral resection of the prostate causes deeper coagulation depth and less bleeding than monopolar transurethral prostatectomy. Urology. 2012;80(5):1116-20.  Iori F, Franco G, Leonardo C, Laurenti C, Tubaro A, D-Amico F, Dini D, De Nunzio C. Bipolar transurethral resection of prostate: clinical and urodynamic evaluation. Urology. 2008;71(2):252-5.
Iori F, Franco G, Leonardo C, Laurenti C, Tubaro A, D-Amico F, Dini D, De Nunzio C. Bipolar transurethral resection of prostate: clinical and urodynamic evaluation. Urology. 2008;71(2):252-5.  Kim, Ji Yoon, Moon, Ki Hak, Yoon, Chang Jun, Park, Tong Choon. Bipolar Transurethral Resection of the Prostate: A Comparative Study with Monopolar Transurethral Resection. Korean Journal of Urology. 2006;47(5):493-497.
Kim, Ji Yoon, Moon, Ki Hak, Yoon, Chang Jun, Park, Tong Choon. Bipolar Transurethral Resection of the Prostate: A Comparative Study with Monopolar Transurethral Resection. Korean Journal of Urology. 2006;47(5):493-497.  Komura K, Inamoto T, Takai T, Uchimoto T, Saito K, Tanda N, Minami K, Uehara H, Takahara K, Hirano H, Nomi H, Kiyama S, Watsuji T, Azuma H. Could transurethral resection of the prostate using the TURis system take over conventional monopolar transurethral resection of the prostate? A randomized controlled trial and midterm results. Urology. 2014;84(2):405-11.
Komura K, Inamoto T, Takai T, Uchimoto T, Saito K, Tanda N, Minami K, Uehara H, Takahara K, Hirano H, Nomi H, Kiyama S, Watsuji T, Azuma H. Could transurethral resection of the prostate using the TURis system take over conventional monopolar transurethral resection of the prostate? A randomized controlled trial and midterm results. Urology. 2014;84(2):405-11.  Kong CH, Ibrahim MF, Zainuddin ZM. A prospective, randomized clinical trial comparing bipolar plasma kinetic resection of the prostate versus conventional monopolar transurethral resection of the prostate in the treatment of benign prostatic hyperplasia. Annals of Saudi medicine. 2009;29(6):429-32.
Kong CH, Ibrahim MF, Zainuddin ZM. A prospective, randomized clinical trial comparing bipolar plasma kinetic resection of the prostate versus conventional monopolar transurethral resection of the prostate in the treatment of benign prostatic hyperplasia. Annals of Saudi medicine. 2009;29(6):429-32.  Lin MS, Wu JC, Hsieh HL, Lin TC, Chen CC, Lin E. Comparison between monopolar and bipolar TURP in treating benign prostatic hyperplasia: 1-year report. Mid-Taiwan J Med. 2006;11(8):143.
Lin MS, Wu JC, Hsieh HL, Lin TC, Chen CC, Lin E. Comparison between monopolar and bipolar TURP in treating benign prostatic hyperplasia: 1-year report. Mid-Taiwan J Med. 2006;11(8):143.  Lv L, Wang L, Fan M, Ju W, Pang Z, et al. Two‑year outcome of high‑risk benign prostate hyperplasia patients treated with transurethral prostate resection by plasmakinetic or conventional procedure. Urology 2012; 80: 389–94.
Lv L, Wang L, Fan M, Ju W, Pang Z, et al. Two‑year outcome of high‑risk benign prostate hyperplasia patients treated with transurethral prostate resection by plasmakinetic or conventional procedure. Urology 2012; 80: 389–94.  Mamoulakis C, Schulze M, Skolarikos A, Alivizatos G, Scarpa RM, Rassweiler JJ, de la Rosette JJ, Scoffone CM. Midterm results from an international multicentre randomised controlled trial comparing bipolar with monopolar transurethral resection of the prostate. European urology. 2013;63(4):667-76.
Mamoulakis C, Schulze M, Skolarikos A, Alivizatos G, Scarpa RM, Rassweiler JJ, de la Rosette JJ, Scoffone CM. Midterm results from an international multicentre randomised controlled trial comparing bipolar with monopolar transurethral resection of the prostate. European urology. 2013;63(4):667-76.  Mamoulakis C, Skolarikos A, Schulze M et al. Results from an international multicentre double-blind randomized controlled trial on the perioperative efficacy and safety of bipolar vs monopolar transurethral resection of the prostate. BJU Int 2012; 109: 240–8.
Mamoulakis C, Skolarikos A, Schulze M et al. Results from an international multicentre double-blind randomized controlled trial on the perioperative efficacy and safety of bipolar vs monopolar transurethral resection of the prostate. BJU Int 2012; 109: 240–8.  Rioja Zuazu J, Mamoulakis C, Skolarikos A et al. Bipolar versus monopolar transurethral resection of the prostate: results of an international multicenter blinded randomized clinical trial. Eur Urol Suppl 2009; 8 (Suppl 4): 266.
Rioja Zuazu J, Mamoulakis C, Skolarikos A et al. Bipolar versus monopolar transurethral resection of the prostate: results of an international multicenter blinded randomized clinical trial. Eur Urol Suppl 2009; 8 (Suppl 4): 266.  Schulze M, Mamoulakis C, Rioja J et al. Preliminary results from an international multicenter blinded randomized clinical trial comparing bipolar with monopolar transurethral resection of the prostate. J Urol 2009; 181: 699.
Schulze M, Mamoulakis C, Rioja J et al. Preliminary results from an international multicenter blinded randomized clinical trial comparing bipolar with monopolar transurethral resection of the prostate. J Urol 2009; 181: 699.  Méndez-Probst CE, Nott L, Pautler SE, Razvi H. A multicentre single-blind randomized controlled trial comparing bipolar and monopolar transurethral resection of the prostate. Canadian Urological Association journal = Journal de l'Association des urologues du Canada. 2011;5(6):385-9.
Méndez-Probst CE, Nott L, Pautler SE, Razvi H. A multicentre single-blind randomized controlled trial comparing bipolar and monopolar transurethral resection of the prostate. Canadian Urological Association journal = Journal de l'Association des urologues du Canada. 2011;5(6):385-9.  Michielsen DP, Debacker T, De Boe V, et al. Bipolar transurethral resection in saline-an alternative surgical treatment for bladder outlet obstruction? J Urol. 2007;178:2035-2039.
Michielsen DP, Debacker T, De Boe V, et al. Bipolar transurethral resection in saline-an alternative surgical treatment for bladder outlet obstruction? J Urol. 2007;178:2035-2039.  Michielsen DP, Coomans D. Urethral strictures and bipolar transurethral resection in saline of the prostate: fact or fiction? J Endourol 2010; 24: 1333–7.
Michielsen DP, Coomans D. Urethral strictures and bipolar transurethral resection in saline of the prostate: fact or fiction? J Endourol 2010; 24: 1333–7.  Michielsen DP, Coomans D, Braeckman JG, Umbrain V. Bipolar transurethral resection in saline: the solution to avoid hyponatraemia and transurethral resection syndrome. Scand J Urol Nephrol 2010; 44: 228–35.
Michielsen DP, Coomans D, Braeckman JG, Umbrain V. Bipolar transurethral resection in saline: the solution to avoid hyponatraemia and transurethral resection syndrome. Scand J Urol Nephrol 2010; 44: 228–35.  Nuhoğlu B, Ayyildiz A, Karagüzel E, Cebeci O, Germiyanoğlu C. Plasmakinetic prostate resection in the treatment of benign prostate hyperplasia: results of 1-year follow up. International journal of urology: official journal of the Japanese Urological Association. 2006;13(1):21-4.
Nuhoğlu B, Ayyildiz A, Karagüzel E, Cebeci O, Germiyanoğlu C. Plasmakinetic prostate resection in the treatment of benign prostate hyperplasia: results of 1-year follow up. International journal of urology: official journal of the Japanese Urological Association. 2006;13(1):21-4.  Patankar S, Jamkar A, Dobhada S, Gorde V. PlasmaKinetic Superpulse transurethral resection versus conventional transurethral resection of prostate. Journal of endourology / Endourological Society. 2006;20(3):215-9.
Patankar S, Jamkar A, Dobhada S, Gorde V. PlasmaKinetic Superpulse transurethral resection versus conventional transurethral resection of prostate. Journal of endourology / Endourological Society. 2006;20(3):215-9.  Rose A, Suttor S, Goebell PJ, Rossi R, Rübben H. [Transurethral resection of bladder tumors and prostate enlargement in physiological saline solution (TURIS). A prospective study]. Der Urologe. Ausg. A. 2007;46(9):1148-50.
Rose A, Suttor S, Goebell PJ, Rossi R, Rübben H. [Transurethral resection of bladder tumors and prostate enlargement in physiological saline solution (TURIS). A prospective study]. Der Urologe. Ausg. A. 2007;46(9):1148-50.  Seckiner I, Yesilli C, Akduman B, Altan K, Mungan NA. A prospective randomized study for comparing bipolar plasmakinetic resection of the prostate with standard TURP. Urologia internationalis. 2006;76(2):139-43.
Seckiner I, Yesilli C, Akduman B, Altan K, Mungan NA. A prospective randomized study for comparing bipolar plasmakinetic resection of the prostate with standard TURP. Urologia internationalis. 2006;76(2):139-43.  Sinanoglu O, Ekici S, Tatar MN, Turan G, Keles A, et al. Postoperative outcomes of plasmakinetic transurethral resection of the prostate compared to monopolar transurethral resection of the prostate in patients with comorbidities. Urology 2012; 80: 402–6.
Sinanoglu O, Ekici S, Tatar MN, Turan G, Keles A, et al. Postoperative outcomes of plasmakinetic transurethral resection of the prostate compared to monopolar transurethral resection of the prostate in patients with comorbidities. Urology 2012; 80: 402–6.  Singh H, Desai MR, Shrivastav P, Vani K. Bipolar versus monopolar transurethral resection of prostate: randomized controlled study. Journal of endourology / Endourological Society. 2005;19(3):333-8.
Singh H, Desai MR, Shrivastav P, Vani K. Bipolar versus monopolar transurethral resection of prostate: randomized controlled study. Journal of endourology / Endourological Society. 2005;19(3):333-8.  Singhania P, Nandini D, Sarita F, Hemant P, Hemalata I. Transurethral resection of prostate: a comparison of standard monopolar versus bipolar saline resection. International braz j urol : official journal of the Brazilian Society of Urology. 2010;36(2):183-9.
Singhania P, Nandini D, Sarita F, Hemant P, Hemalata I. Transurethral resection of prostate: a comparison of standard monopolar versus bipolar saline resection. International braz j urol : official journal of the Brazilian Society of Urology. 2010;36(2):183-9.  Xie CY, Zhu GB, Wang XH, Liu XB. Five-year follow-up results of a randomized controlled trial comparing bipolar plasmakinetic and monopolar transurethral resection of the prostate. Yonsei medical journal. 2012;53(4):734-41.
Xie CY, Zhu GB, Wang XH, Liu XB. Five-year follow-up results of a randomized controlled trial comparing bipolar plasmakinetic and monopolar transurethral resection of the prostate. Yonsei medical journal. 2012;53(4):734-41.  Yang S, Lin WC, Chang HK, Hsu JM, Lin WR, Chow YC, Tsai WK, Lee TA, Lo KY, Chow K, Chen M. Gyrus plasmasect: is it better than monopolar transurethral resection of prostate?. Urologia internationalis. 2004;73(3):258-61.
Yang S, Lin WC, Chang HK, Hsu JM, Lin WR, Chow YC, Tsai WK, Lee TA, Lo KY, Chow K, Chen M. Gyrus plasmasect: is it better than monopolar transurethral resection of prostate?. Urologia internationalis. 2004;73(3):258-61.  Yoon CJ, Kim JY, Moon KH, Jung HC, Park TC. Transurethral resection of the prostate with a bipolar tissue management system compared to conventional monopolar resectoscope: one‑year outcome. Yonsei Med J 2006; 47: 715–20.
Yoon CJ, Kim JY, Moon KH, Jung HC, Park TC. Transurethral resection of the prostate with a bipolar tissue management system compared to conventional monopolar resectoscope: one‑year outcome. Yonsei Med J 2006; 47: 715–20.  Cleves A, Dimmock P, Hewitt N, Carolan-Rees G. The TURis System for Transurethral Resection of the Prostate: A NICE Medical Technology Guidance. Applied Health Economics and Health Policy. 2016;14:267-279. | CrossRef |
Cleves A, Dimmock P, Hewitt N, Carolan-Rees G. The TURis System for Transurethral Resection of the Prostate: A NICE Medical Technology Guidance. Applied Health Economics and Health Policy. 2016;14:267-279. | CrossRef | Treharne C, Crowe L, Booth D, Ihara Z. Economic value of the transurethral resection in saline system for treatment of benign prostatic hyperplasia in England and Wales: systematic review, meta-analysis, and cost–consequence model. Eur Urol Focus 2016.
Treharne C, Crowe L, Booth D, Ihara Z. Economic value of the transurethral resection in saline system for treatment of benign prostatic hyperplasia in England and Wales: systematic review, meta-analysis, and cost–consequence model. Eur Urol Focus 2016.  Oelke, Matthias, et al. "EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction." European urology 64.1 (2013): 118-140.
Oelke, Matthias, et al. "EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction." European urology 64.1 (2013): 118-140.